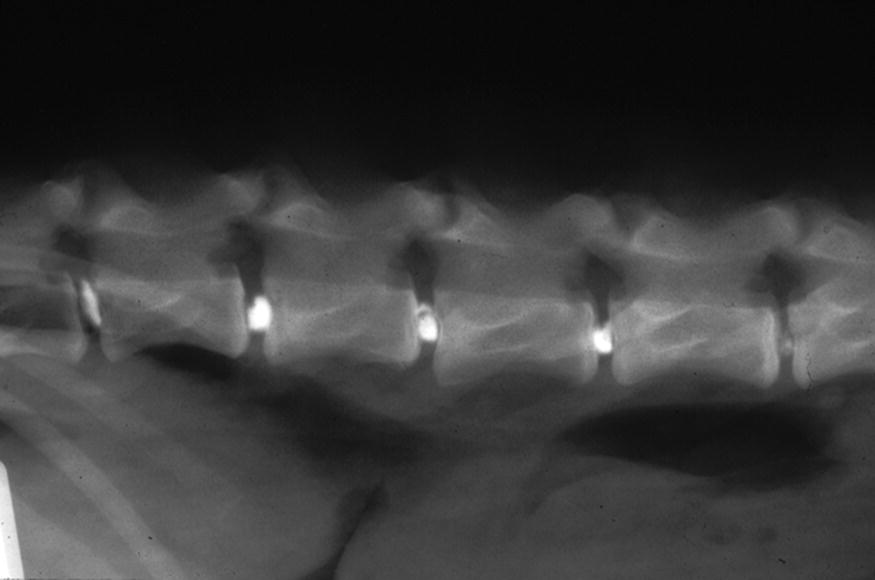
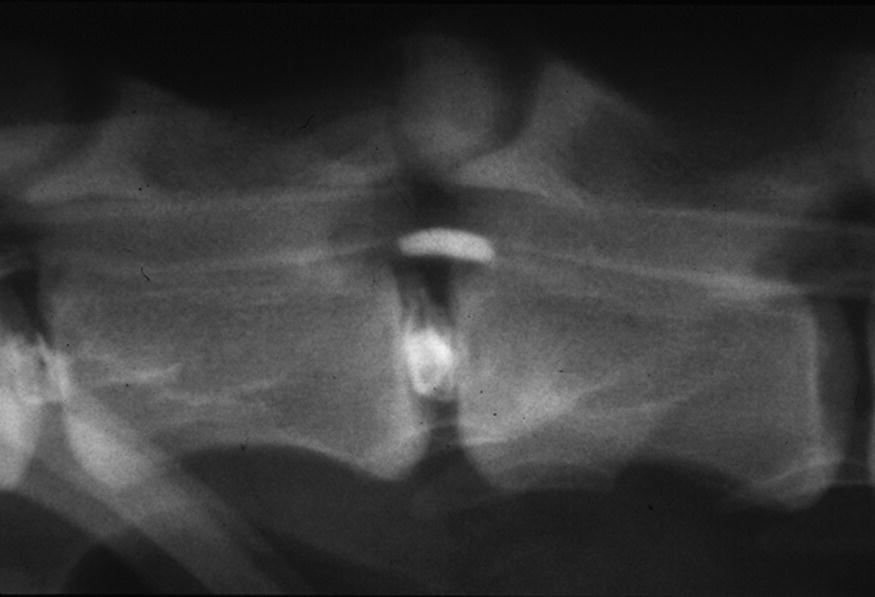
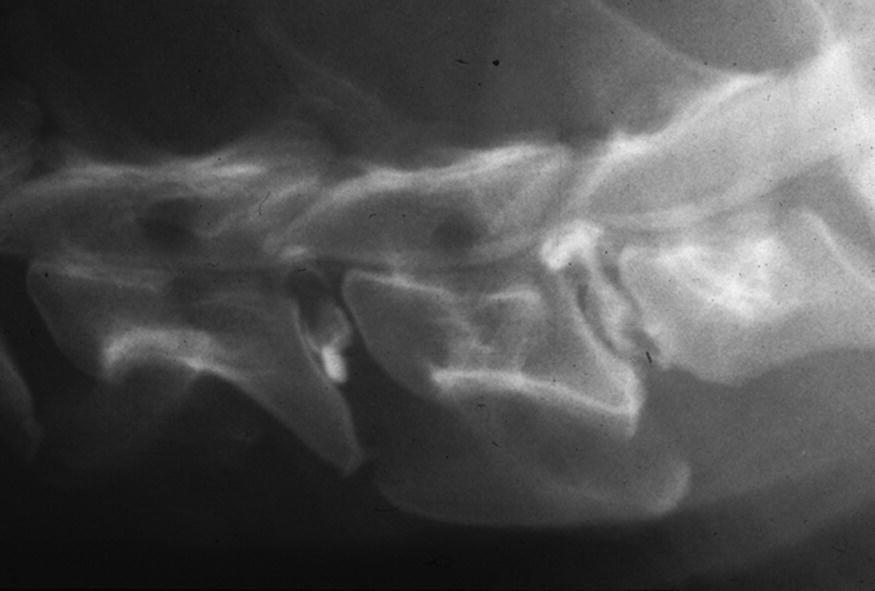
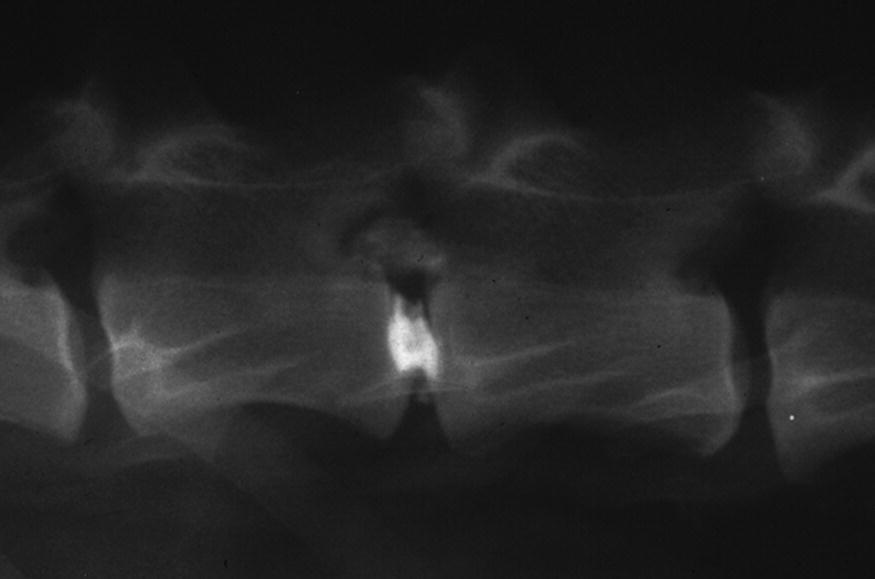
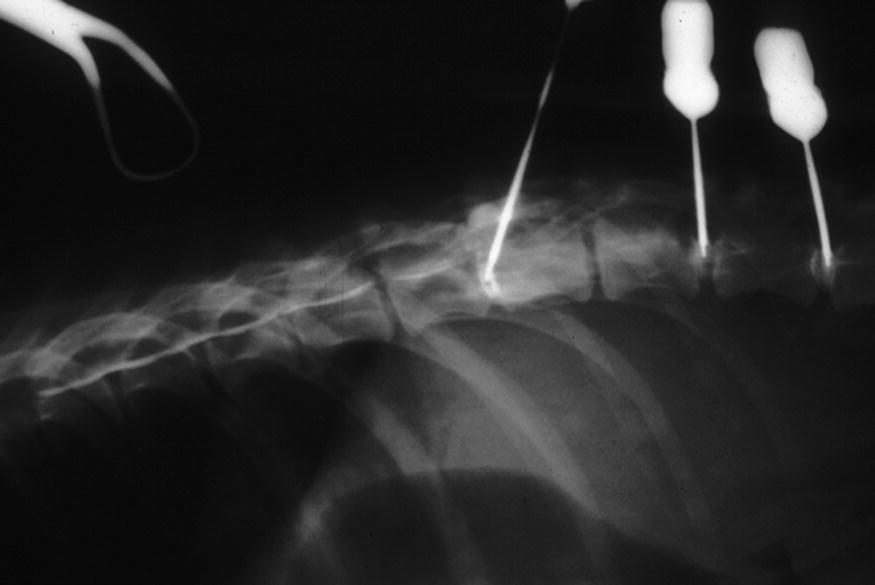
26 James F. (Jeff) Biggart Discography is the imaging of the intervertebral disc by radio-opaque contrast material introduced percutaneously into the nucleus pulposus. It is primarily a diagnostic technique testing the integrity of the annulus and nucleus. Traditionally, physicians and veterinarians use this technique to diagnose herniated discs in the last several lumbar spaces of the vertebral canal. Access to the vertebral canal has traditionally been dorsally, between the facets of the cranial and caudal lamina over a disc space. To avoid penetration of the spinal cord and dura mater, a more lateral or dorsolateral approach has been used [1, 2]. This technique is minimally invasive with the use of fluoroscopy. Used in conjunction with nucleolysis, both diagnosis and treatment of herniated discs can be accomplished with one needle placement. It aids in the diagnosis of disc herniation in cases of suspected false negative myelograms without requiring surgical exploration of these suspected disc levels. Herniations within large areas devoid of myelographic contrast due to spinal cord swelling may be identified. In veterinary patients, discography requires general anesthesia, negating one value found in humans, namely, where disc injection can reproduce clinical symptoms in a conscious patient and aid in lesion localization. Classically, fluoroscopy is necessary for needle placement; however, needle placement can be accomplished successfully with newer high-definition digital radiographic systems. In addition, with the advent of magnetic resonance imaging, it is possible to distinguish normal-appearing discs from those that have undergone degeneration (with and without herniation) using a completely noninvasive methodology (see Chapter 16). Normal discs demonstrate a contrast pattern of a small, oval, pearl-like image of the nucleus pulposus (Figure 26.1). Depending on the volume of the contrast material injected, complete or incomplete filling of the nucleus pulposus may be the result. Introduction of contrast material into a normal disc with an intact annulus is difficult, as a volume of the nucleus must be replaced by contrast material. Since this is a closed confined space, considerable pressure may be needed to introduce additional material [3]. Figure 26.1 Normal discograms. Abnormal discs can demonstrate several patterns after contrast introduction. Long-standing disc disease may produce complete collapse of the intervertebral space leaving minimal space between the end plates for contrast deposition. Generally, these discs have minimal annular confinement of the nucleus and contrast may leak into adjacent tissues, resulting in no useful images (Figure 26.2). Figure 26.2 Protruded discogram. Contrast leaks into the annulus with bulging outside the traditional confines of the annulus (Figure 26.3). Figure 26.3 Protruded discogram. Contrast leaks through the annulus but is still contiguous with the disc space (Figures 26.4 and 26.5). Figure 26.4 Extruded discogram. Figure 26.5 Extruded discogram. Contrast leaks into the vertebral canal with no continuity with the disc space (Figure 26.6). Figure 26.6 Sequestered discogram. These patterns are seldom seen without continuously recorded dynamic fluoroscopy. Further study is needed, but these patterns may be related to and help explain the etiology of fibrocartilaginous emboli with spinal cord infarction (see Chapter 9), ascending/descending myelomalacia (see Chapter 12), and possibly other spinal cord pathologies. Contrast media extrudes into the adjacent vertebral body medullary spaces. This produces an instantaneous and very transient blush of contrast into the vertebral body. Contrast flows into the vertebral venous sinuses in the ventral vertebral canal. This is a very transient pattern with flow toward the heart (Figure 26.7). Figure 26.7 Intravenous discogram. Contrast medium flows into the arterial system of the vertebral canal and vertebral body, characterized by a tortuous pattern without obvious connection to the vertebral canal. Nucleolysis (chemonucleolysis, discolysis, disc injection, intradiscal therapy) is the enzymatic dissolution of the nucleus pulposus of the intervertebral disc. The technique involves percutaneously placing needles into the nucleus with the deposition of proteolytic enzymes such as chymopapain or collagenase. The goal is to have these enzymes follow the path of the herniated disc, mix with and dissipate the disc in the vertebral canal, and thus relieve pressure on the spinal cord and nerve roots. Early in the development of nucleolysis, controversy arose when two human cases of transverse myelitis were produced by radiologists who inadvertently placed chymopapain into the subarachnoid space following posterior transdural discograms. The risk for this error was reduced by development of a more lateral approach avoiding the spinal cord altogether. However, the medicolegal damage was done, and controversy ensued as to whether radiologists, orthopedists, neurologists or other specialists should perform this procedure. The U.S. Federal Drug Administration became involved as it had oversight for the use of these enzymes and their clinical application. Clinical outcome reports revealed a success rate of between 70 and 80% for nucleolysis using these enzymes, which, by comparison to traditional surgical outcomes, was less than an ideal result. Eventually legal issues reduced the use of chymopapain and collagenase in the United States to such a point that production of the enzymes was unprofitable and clinical availability ceased. The popularity of this type of minimally invasive procedure continued in Canada and Europe, however. The finding that failed nucleolysis did not preclude later surgery, and that nearly 70% of patients avoided surgery, encouraged the continued use of these enzymes as a treatment for disc herniation in humans [4].
The Use of Discography and Nucleolysis in Dogs
Discography
Advantages
Disadvantages
Discographic patterns
Collapsed discs
Protruded discs
Extruded discs


Sequestered discs
Intravascular discograms
A. End plate penetration
B. Intravenous discograms
C. Intra-arterial discograms
Nucleolysis
Historical perspectives
Use of nucleolysis in dogs
Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


