Chapter 20 The Neurologic Examination
NEUROLOGIC EXAMINATION—OVERVIEW
The differential diagnosis must be based on the anatomic diagnosis, and the order of significance of these disorders will depend on your evaluation of the signalment and history. Be sure to consider all five major kinds of lesions in your differential diagnosis or a list of these with which you are comfortable. Our list is described in Chapter 1 and includes malformation, injury, inflammation, neoplasia, and degeneration (MIIND). Your experience with the anatomic diagnosis together with the signalment and history will often lead to a presumptive clinical diagnosis. Further examination of the patient with ancillary procedures must depend on your differential diagnosis and what you consider to be the most likely clinical diagnosis. Many factors will be considered in this selection, including the cost to the patient’s owner.
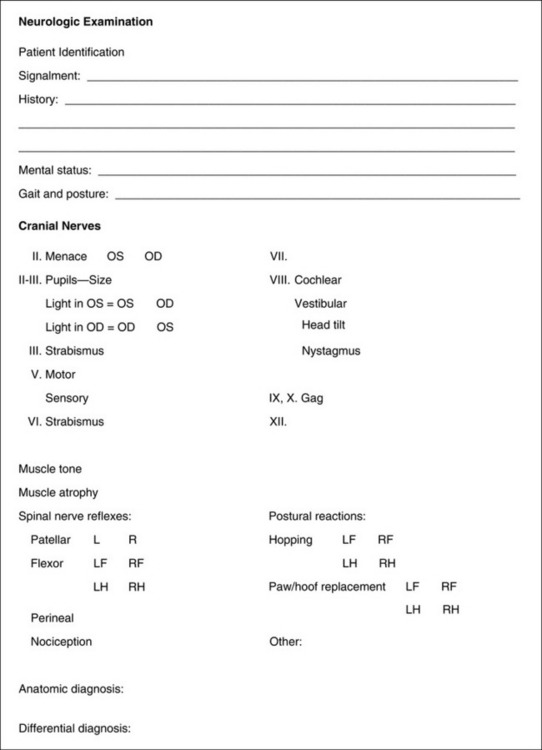
Be sure to record carefully all your observations from the neurologic examination, and never rely on your memory. Many forms are available for recording your observations. Some of these forms list in detail every possible response that is present or absent, with numbers to estimate the level of response. The considerable variation between individual patients of the same species makes the recording of the degree of a response less reliable and often misleading. We prefer a less time-consuming form that is easier to follow and adaptable to all species (Fig. 20-1).
Signalment
The signalment of the patient provides the examiner with the age, sex, breed, and use of the patient. When considered together with the chief complaint, this information may help direct the line of questioning as you take the history. For example, canine patients younger than 1 year that are presented for seizures are more likely to have an inflammatory lesion than a neoplasm, and lead poisoning is more common in dogs younger than 1 year. Toy breeds with functional hypoglycemia usually have seizures when they are younger than 6 months. Hypoglycemic seizures caused by a functional neoplasm of the pancreatic islet beta cells are rarely seen before 4 years of age. Neoplasms of the nervous system usually occur in the older patient, except for lymphosarcoma, which can occur at any age, and a spinal cord nephroblastoma, which occurs in young dogs. Exceptions are common. Intervertebral disk extrusion-protrusion is a concern in the chondrodystrophic breeds anytime after 1 year of age, whereas in the nonchondrodystrophic breeds, it is rarely a concern before 5 years of age.
History
When a patient is brought in with the complaint of seizures, you need to obtain as thorough a description of the seizure event as possible to be certain of its authenticity and to determine the kind (classification) of seizure. The majority of seizures seen in domestic animals are generalized seizures. This type of seizure is the one that most commonly occurs in idiopathic epilepsy, most intoxications, and many prosencephalic structural disorders. Complex partial seizures (psychomotor) are more common in lead poisoning and diseases that affect the limbic system. Descriptions of these seizures often include episodic activities of the patient that the owner will describe as bizarre behavior or hysteria. Simple partial seizures may occur with or without confusion but with no loss of consciousness. The episodic activity is limited to groups of skeletal muscles such as the facial muscles or the muscles of one or both limbs on one side. Distinguishing between a simple partial seizure and a movement disorder may be difficult. The latter is described in Chapter 8. It is very useful to have the owner provide a video of the episodic event for you to study, given that these seizures rarely occur in your hospital. A thorough description or a video evaluation of a dog that is exhibiting episodes of collapsing will help distinguish among a seizure, cataplexy, movement disorder, syncope, or neuromuscular disorder. Episodic behavioral disorders are also best evaluated on videos.
Be sure to ask about the patient’s behavior in its home environment. The owner will be aware of subtle changes that you cannot appreciate in your hands-on examination.
The following additional questions should be asked as part of the historical examination:
What diet do you feed? Raw or homemade diets may affect the nervous system.
NEUROLOGIC EXAMINATION— SPECIFICS
The neurologic examination can be divided into five parts:
Remember that, as described in Chapter 5, spinal nerve reflexes require only the specific peripheral nerves that innervate the area being tested and the spinal cord segments with which they connect. Postural reactions depend on the same components as the spinal nerve reflexes plus the cranial projecting pathways in the spinal cord white matter to the brainstem, cerebellum, and frontoparietal portion of the cerebral hemisphere and the caudal-projecting upper motor neuron (UMN) pathways that return from the cerebrum and brainstem and comprise tracts in the white matter of the spinal cord that terminate in the cervical and lumbosacral intumescences. These postural reactions test the integrity of nearly the entire peripheral and central nervous systems. By themselves, the postural reactions are relatively less reliable for lesion location.
Sensorium—Mental Attitude
An assessment should be made and recorded of the patient’s sensorium, its mental attitude, and response to the immediate environment and attitude to being handled by you. The owner is the best judge of subtle changes in the patient’s behavior in its normal environment. Be sure to explore this issue when you obtain the history. Considerable patient variation exists in how alert and responsive the patient may be in the examination room of a veterinary hospital. Do not mistake a very laidback behavior for depression. Descriptive terms for this portion of your examination include alert and responsive, depressed, lethargic, obtunded, semicoma (stupor), and coma. These states are described with the discussion of the ascending reticular activating system (ARAS) in Chapter 19. Other descriptions include acting vague, disoriented, hyperactive, propulsive, and aggressive.
As a rule, alterations in the patient’s normal sensorium reflect disturbances in the ARAS and limbic system components of the cerebrum or rostral brainstem. Be sure to evaluate the sensorium of a recumbent patient thoroughly. Recumbency from diffuse neuromuscular disease or focal cervical spinal cord disease will not alter the patient’s sensorium. A horse that is recumbent as a result of botulism may appear to be severely depressed or lethargic because it has no voluntary movement to show a response. The quality of the tetraparesis or tetraplegia with a cervical spinal cord lesion is the same as that caused by a mid- to caudal brainstem lesion, but the latter circumstance will often alter the patient’s level of response to its environment. Be aware that horses that suddenly become recumbent from an aortic thromboembolism or spinal cord ischemia and hemorrhage from an equine herpesvirus infection may act delirious as they struggle to stand. Horses that become acutely recumbent from a pontomedullary lesion that involves the vestibular system may be extremely disoriented and thrash wildly and appear maniacal as they try to recover their balance. The behavior is often remarkably altered in horses that have acute encephalitis from infection with the rabies, eastern equine encephalomyelitis, or West Nile viruses, as well as from hepatic encephalopathy. In human neurology, the Glasgow scale is used to report the patient’s sensorium objectively. Scales of this nature are presently being modified and evaluated for animals but are not routinely used in veterinary medicine at this time.
Gait and Posture
Ataxia is a synonym for incoordination, and we recognize three qualities of ataxia: (1) GP, (2) vestibular (special proprioception [SP]), and (3) cerebellar. GP ataxia reflects the lack of information reaching the central nervous system (CNS) that informs the CNS of where the neck, trunk, and limbs are in space and the state of muscle contraction at any time. Without this GP information, the onset of protraction of a limb may be delayed, and the stride may be lengthened. During protraction, the limb may swing to the side (abduct) or swing under the body (adduct), overflex during protraction, scuff or drag one or more digits, and in the support phase, stand on the dorsal aspect of one or more digits. Remember that these clinical signs overlap with those caused by dysfunction of the UMN. The gait pattern of a patient with a focal cervical spinal cord lesion between the C1 and C5 segments reflects dysfunction of the UMN and GP systems and is observed as spastic tetraparesis and ataxia. This cervical spinal cord pattern is often recognized by the overextension of the thoracic limbs creating an overreaching or floating action. This clinical sign can be augmented by holding the head and neck extended as the patient is led, especially in horses. This unique form of hypermetria must not be confused with cerebellar ataxia in which the limb is overflexed on protraction. At no time do we try to differentiate between conscious (cerebral) and unconscious (cerebellar) GP pathways! No examination will clearly differentiate these two pathways from each other or from the UMN pathways. No pure conscious proprioceptive deficit exists. This term should be dropped from the clinician’s vocabulary. See Video 10–36 for this combination of UMN and GP clinical signs. Vestibular ataxia reflects the loss of orientation of the head with the eyes, neck, trunk, and limbs, which results in a loss of balance. Lesions in this system cause the patient to lean, drift, or fall to one side. However, the patient’s strength and awareness of where its limbs are in space are normal with lesions confined to this system. This ataxia is usually accompanied by a head tilt and sometimes abnormal nystagmus. We will occasionally blindfold our patients with bandage material in small animals or a towel in horses and cattle to exacerbate vestibular ataxia. See Video 12-1. Cerebellar ataxia most commonly causes hypermetric ataxia characterized by sudden bursts of motor activity with a marked overflexion of the limbs on protraction. Vestibular system components exist in the cerebellum that, if dysfunctional, may cause loss of balance, head tilt, and abnormal nystagmus. Cerebellar ataxia in horses produces more hypertonia than hypermetria when compared with other species of domestic animal. See Videos 13-9 and 13–21.
Postural Reactions
Hopping responses, in our opinion, are the most reliable of the postural reactions that we test. While still straddling the patient, move back to the thoracic limbs, and while elevating the abdomen with one hand, pick up the thoracic limb on the opposite side with your other hand. With all the weight supported on the other thoracic limb, hop the patient laterally on that thoracic limb. Go as far as you can without moving your pelvic limbs. Then switch hands and hop the patient back on the other thoracic limb. Repeat this test many times until you are sure the thoracic limbs are normal or abnormal. As you stand over your patient and look down the lateral aspect of the limb that is being hopped, the limb should move as soon as you move the shoulder region laterally over the paw or hoof. Any delay in this response is abnormal. The hopping movements should be smooth and fairly rapid and not irregular or excessive. The paw or hoof should never drag or land on its dorsal surface. Carefully compare one thoracic limb with the other. To test the hopping responses in the pelvic limbs, stand beside the patient, and place your forelimb that is closest to the patient’s head between its thoracic limbs with your hand on its sternum. Lift up on the thorax just enough to take the weight off of the thoracic limbs. With the other hand, pick up the pelvic limb on the side where you are standing and push the patient toward the pelvic limb that is bearing the weight. This action will force the patient to hop on that pelvic limb in a direction away from you. After a few hops, switch sides, and hop the patient back on the other pelvic limb. Keep repeating this test until you have determined that the response is normal or abnormal. The responses should be brisk and smooth but will not be quite as rapid as in the thoracic limbs. While you are hopping the patient, you will also be aware of the degree of tone in the limb that is bearing all the weight. In large dogs or small farm animals that are too heavy to lift for this testing, the same observations can be made while the patient is walked on one side (hemiwalking). Hemiwalking is performed by standing on one side of the patient. Grasp each limb on that side and lift the limbs off the ground surface and push the patient toward its opposite side. The patient will hop with both limbs on that side. Switch sides and repeat the hemiwalking performance on the opposite limbs. Be sure to compare one thoracic limb with the other and one pelvic limb with the opposite pelvic limb.
One might conclude that these postural reactions are relatively nonspecific. This conclusion is absolutely correct. Why then are they useful? First, testing postural reactions acts as a screen for detecting abnormalities in the nervous system. Abnormal responses will be the first clinical sign of any progressive lesion in any part of the central or peripheral nervous system that is involved in limb movement. One or more of these postural reactions may be abnormal before any detectable abnormality in the gait is observed. Second, their importance in localizing lesions is dependent on the results of the rest of the neurologic examination. If the gait is normal in the environment of your examination and one or more of the postural reactions are abnormal in the limbs on one side of the body, a contralateral prosencephalic lesion is strongly suggested. This test is the most useful of the three clinical tests that we use for prosencephalic disorders. If you have a patient with clinical signs of a unilateral vestibular system disorder with a normal gait but the postural reactions are abnormal, then the lesion is in the central components of the vestibular system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree