Chapter 42The Metatarsophalangeal Joint
Anatomy
The MTP joint is nearly identical to the metacarpophalangeal joint and is composed of the distal articular surface of the third metatarsal bone (MtIII), its sagittal ridge, and the medial and lateral condyles; the medial and lateral proximal sesamoid bones (PSBs); and the proximal articular surface of the proximal phalanx, which has a prominent axially located sagittal groove (see Chapter 36). Minor differences exist in the shape and length of the proximal phalanx between the forelimbs and hindlimbs but are not clinically relevant. The MTP joint normally is more upright than the metacarpophalangeal joint and can achieve a greater degree of flexion. The lateral-to-medial width of the lateral condyle of the MtIII is less than that of the medial condyle. In racehorses, based on the results of scintigraphic examination, stress-related bone injury occurs predominantly in the lateral aspect of the hindlimb, which may be related to the smaller surface area of the lateral condyle. The joint capsule, intersesamoidean and collateral sesamoidean ligaments, suspensory ligament (SL) attachments, and digital flexor tendons all function to move and support the MTP joint. The dense collateral ligaments have short deep, and long superficial components. In the hindlimb the lateral digital extensor tendon joins with the long digital extensor tendon in the proximal dorsal metatarsal region. Therefore only the long digital extensor tendon is encountered during arthrocentesis or surgical procedures performed in the dorsal aspect of the MTP joint.
Conformation
Fetlock valgus and varus deformities affect the MTP joint in foals, but fetlock varus deformity is of most concern and needs to be corrected early (see Chapter 58). Most normal horses are slightly toed out in the hindlimbs, but in some horses toed-out conformation may play a role in uneven load distribution and affect hindlimb gait. Horses with toed-out conformation tend to travel close behind and stab laterally during limb advancement, a gait that may cause excessive lateral shoe wear and hoof imbalance. Such gait and hoof imbalance may predispose the lateral aspect of the MTP joint to stress-related bone injury. Horses that are excessively straight behind have an abnormal degree of extension (or dorsiflexion) of the MTP joint. This conformation is undesirable because it places abnormal load on the SL and predisposes to suspensory desmitis, stifle joint lameness, and secondary osteoarthritis (OA) of the MTP joint. Horses with bull-nose foot conformation and long, weak hind pasterns may be predisposed to injury (see Chapter 4, Figure 4-34). When viewed from behind when walking and trotting, some horses—especially those with a base-narrow conformation—appear to collapse laterally over each hind fetlock.
Clinical Characteristics and Diagnosis of Metatarsophalangeal Joint Lameness
Lameness of the MTP joint occurs in most sports horses and is common in the racehorse. Both Standardbred (STB) and Thoroughbred (TB) racehorses are prone to injury of this joint, but MTP joint lameness is more common in the STB, because gait and load distribution predispose to hindlimb lameness in this breed (see Chapter 2). Lameness of the MTP joint should never be discounted in the TB racehorse, and in both the STB and TB racehorse in my referral practice, conditions of this joint are the most common cause of undiagnosed hindlimb lameness. Curiously, MTP joint lameness is apparently uncommon in Western performance horses despite the predominant use of the hindlimbs for many maneuvers and thus tremendous forces applied to the MTP joint (see Chapter 120). With Western performance horses, sporting activity may play a role because in barrel horses and team roping heading horses, lameness of the distal aspect of the hindlimb including the MTP joint was uncommon, but in team roping heeling horses, the MTP joint contributed substantially to lameness and poor performance.3,4 There is no pathognomonic historical information that incriminates the MTP joint more than other sources of hindlimb lameness, but racehorses are usually worse in turns. Absence of palpable abnormalities and clinical signs incriminating other areas of pain in the hindlimb, particularly in a racehorse, would make me consider the MTP joint region, because it is the most commonly overlooked area in my practice. In horses with bilateral MTP joint lameness, poor performance may be the only historical finding and overt signs of lameness may not be present, but a short, choppy gait or intermittent, shifting hindlimb lameness is seen. A gait typical of bilateral stress-related bone injury of the distal aspect of the MtIII in TB racehorses being trotted in hand is described as an “exaggerated pelvic excursion” in a dorsoventral direction (see Chapter 107).
Intermittent, Severe Lameness
Horses with intermittent, severe lameness of the MTP joint may be able to train and perform at some level but develop severe lameness afterward. When exhibiting clinical signs, horses are lame at the walk, even toe-touching lame, and are obviously lame at the trot (grade 3 or 4 of 5), but after resting and receiving nonsteroidal antiinflammatory drugs (NSAIDs), horses are often able to gallop, jog, or train within 1 to 5 days. In some instances horses may be able to race, only to become lame once again. When walking in hand, horses often show marked lameness while turning, even if they are sound while walking in a straight line. Obvious signs of inflammation usually are not present, but horses generally respond positively to the lower limb flexion test and may show a painful response to deep palpation. Horses with incomplete midsagittal or dorsal (frontal) fractures of the proximal phalanx often manifest a painful response when firm digital pressure is placed on the proximal, dorsal aspect (see Figure 6-37). Effusion may be present, but it is often absent or minimal even in horses with incomplete fractures. Because clinical signs may be difficult to detect, diagnostic analgesia is often necessary. Radiographs are usually diagnostic, but if findings are equivocal or the radiographs are obtained before radiological changes develop, scintigraphic examination or follow-up radiographic examination in 10 to 14 days is required. Digital and computed radiography can be helpful. Conditions such as incomplete fractures of the MtIII, the proximal phalanx, and the PSBs and moderate OA are in this category.
Diagnostic Analgesia
Articular pain originating from the MTP joint can usually be abolished or at least partially alleviated by intraarticular analgesia. Because only one injection is required, intraarticular analgesia is easier and safer to perform than perineural techniques, but pain originating from subchondral bone may not abate or may be only partially alleviated by intraarticular analgesia. Therefore, it is extremely important to recognize that the low plantar perineural technique or a variation must be used, because it is more effective in alleviating pain from all sources (see Chapter 10).
A variation of the low plantar block, the lateral plantar metatarsal block, can be performed in horses with stress-related bone injury of the distal plantarolateral aspect of the MtIII (see Chapter 107).5 This block is particularly valuable in horses with bilateral lameness, because after one limb is blocked, the horse becomes obviously lame in the other. Other sources of pain located laterally in the MTP joint, such as sesamoiditis, small fractures of the PSBs, can be blocked by this technique, but the most common reason horses improve after lateral plantar metatarsal analgesia is alleviation of subchondral bone pain of the distal aspect of the MtIII.
The clinician should be aware that it is possible to inadvertently block pain associated with subchondral bone of the MTP joint when performing plantar digital or plantar perineural analgesia. This occurs most frequently in racehorses with midsagittal fracture of the proximal phalanx but can occur in horses with OA or other conditions (see Chapters 10 and 41).
Imaging Considerations
Radiography and Radiology
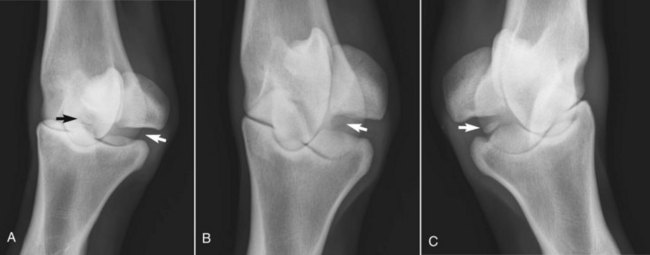
Horizontal oblique images are useful to evaluate the proximal-dorsal aspect of the proximal phalanx for the presence of osteochondral fragments, but overlap between the base of the PSBs and the proximal aspect of the proximal phalanx can hide lesions associated with the distal-plantar aspect of the joint. Overlap in the plantar aspect of this joint is more common than in the metacarpophalangeal joint and occurs when the distal hindlimb is not vertically positioned. The x-ray beam should be angled down 15 to 20 degrees to separate the PSBs and proximal phalanx (Figure 42-1).
Scintigraphic Examination
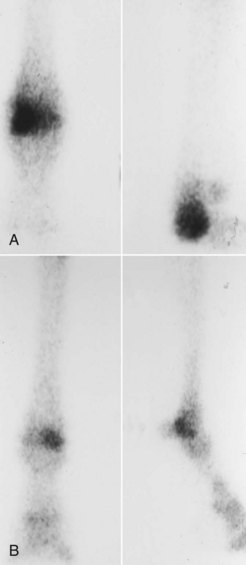
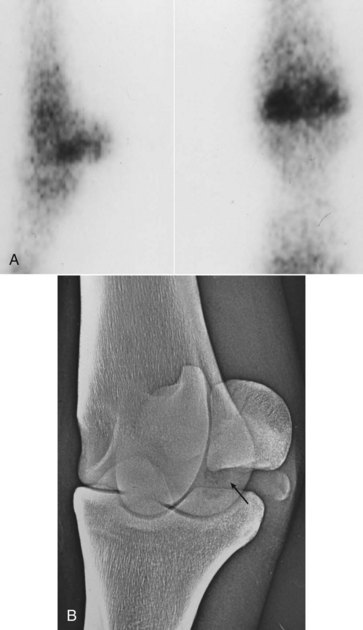
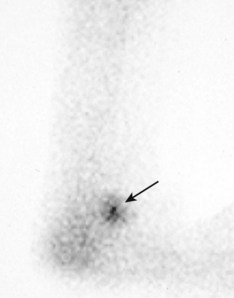
Scintigraphic examination is the best way to establish a diagnosis in many horses with intermittent, severe, or chronic low-grade lameness of the MTP joint. The most common scintigraphic findings in the MTP joint of STB and TB racehorses are focal areas of increased radiopharmaceutical uptake (IRU) that involve the distal plantarolateral aspect of the MtIII (see Figure 19-20, A; Figures 42-2 and 42-3).7 This IRU is a form of stress-related bone injury and early OA that is found in many racehorses with chronic, low-grade lameness, bilateral hindlimb lameness, and poor performance. Special radiographic images may then reveal increased radiopacity or radiolucent defects (see Figures 42-1 and 42-3). Similar scintigraphic findings are seen in horses with lateral condylar fractures of the MtIII. Focal areas of IRU are seen in horses with midsagittal or dorsal frontal fractures of the proximal phalanx (see Figure 19-20, C), sesamoiditis (Figure 42-4), and osteochondrosis of the plantar process of the proximal phalanx (see Figure 23-1; Figure 42-5). Often areas of IRU are found in unusual sites, such as those associated with the medial PSB (osteochondral fragments of the abaxial border and sesamoiditis), intersesamoidean ligament injury with radiolucent defects in one or both PSBs, incomplete fractures of the PSBs, and medial condylar fractures of the MtIII. Any focal area of IRU located medially in the MTP joint should be investigated, because incidental findings are unusual in this location.
Scintigraphic changes are usually less pronounced in nonracehorses, and negative or equivocal results often occur. The most common scintigraphic findings in jumpers and dressage horses with MTP joint lameness are diffuse mild areas of IRU in all bones or focal mild or moderate IRU in the dorsal or central aspects of the joint that involve the distal aspect of the MtIII and proximal aspect of the proximal phalanx and are associated with radiological evidence of marginal osteophytes and enthesophytes. There is a distinct difference in the scintigraphic and radiological appearance of the MTP joint of nonracehorses and racehorses, because in racehorses IRU is generally focal in nature and IRU and radiological changes involve the plantar aspect of the joint. In a 2004 study of clinically sound horses, generalized, even radiopharmaceutical uptake across the distal aspect of the MtIII and the proximal aspect of the proximal phalanx was found.8 Radiopharmaceutical uptake was significantly higher in the condyles of the MtIII of hindlimbs than in forelimbs, there was no effect of age, and there was a trend for region of interest ratios to be higher in the right hind MTP joint when compared with the left.8 In some nonracehorses arthroscopic examination has revealed full-thickness cartilage damage that primarily involves the distal dorsomedial aspect of the MtIII (medial condyle) and is consistent with OA. Focal IRU in the proximal aspect of the plantar pouch is seen in horses with severe OA (an ominous finding) (see Figure 19-20, B). I believe this finding is caused by accumulation of subchondral bone fragments in this location or modeling of the distal plantar aspect of the MtIII.
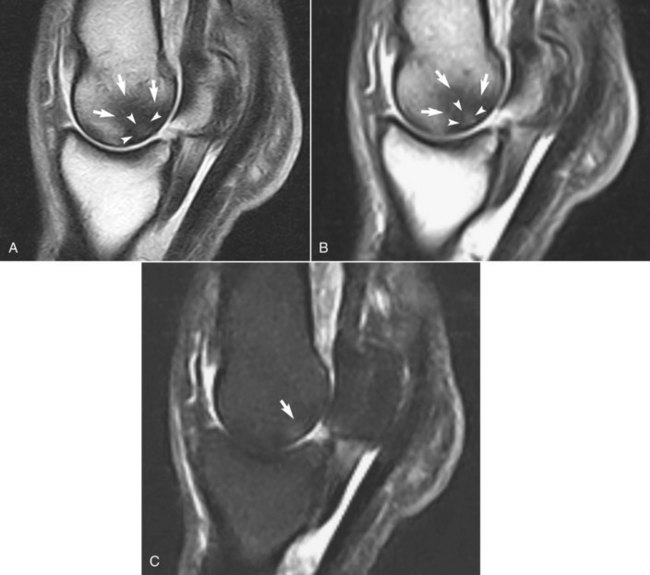
Magnetic Resonance Imaging
MRI is useful to evaluate bone and soft tissue abnormalities in the MTP joint and nearby structures (see Chapters 21, 107, and 108). In fact, in some horse-dense locations such as Newmarket, England, examination of the metacarpophalangeal and MTP joints using standing low-field MRI has become as commonplace as scintigraphic examination and is often preferentially requested by TB trainers.9 In TB and STB racehorses with maladaptive or nonadaptive bone remodeling of the distal aspect of the MtIII, MRI examination reveals extensive subchondral bone damage characterized predominately by low signal intensity of the plantar aspect of the lateral condyle of MtIII on T1- and T2-weighted images, a finding supporting the existence of chronic, sclerotic subchondral bone (Figure 42-6, A and B). Within the areas of low signal intensity is often a small area of high signal intensity near the articular cartilage (see Figure 42-6, A and B). In fat-suppressed short tau inversion recovery (STIR) image sequences, small, focal areas of high signal intensity within sclerotic bone are often found, indicating the presence of necrotic, and perhaps ischemic, bone, but widespread areas of high signal intensity consistent with bone edema from acute trauma are not often seen (Figure 42-6, C). Although numerous authors or speakers have characterized these lesions as bone bruises, bone edema (fluid accumulation) characteristic of bone bruises found in subchondral bone in people is not a hallmark of this common lesion in horses. Large areas of increased signal intensity likely indicated the presence of a fracture of the MtIII. Areas of increased signal intensity within sclerotic subchondral bone in horses with repetitive stress injuries could represent proteinaceous fluid, but likely represent regions of necrotic bone or granulation tissue.9 Areas of necrotic bone seen on magnetic resonance (MR) images correspond to radiolucent defects. Areas of bone loss, necrotic subchondral bone, or areas of intense resorption within sclerotic bone may warrant consideration when trying to manage horses with this lesion (see later). In horses with acute-onset clinical signs consistent with acute subchondral bone injury or fracture, bone edema can be more prominent. In 13 horses, most of which were nonracehorses, with lameness of metacarpophalangeal or MTP joints and without radiological abnormalities, the most common finding was decreased signal intensity in T1-weighted images, indicating the presence of sclerotic subchondral bone.10 In nine horses, decreased signal intensity in T-2*-weighted images was consistent with sclerosis, but five had increased signal intensity in fat-suppressed STIR images consistent with what was described as fluid accumulation within the sclerotic regions.10 Importantly, MRI abnormalities and subchondral bone lesions were found not only in racehorses but in horses used for show jumping and general purpose riding.10 Lesions similar to those described for racehorses were seen in the MTP joint of sports horses.11 Focal areas of IRU seen scintigraphically appeared in MR images as areas of low signal intensity on T1- and T2-weighted images with or without small areas of increased signal intensity in STIR images, indicating the presence of chronic, repetitive stress injuries of the distal aspect of the MtIII in sports horses in addition to acute, traumatic injuries.11 In an earlier study of 11 horses (eight racehorses), subchondral bone damage was identified using MRI, although there were no or equivocal radiological abnormalities.12 Four horses had lesions in the metacarpophalangeal or MTP joints. Horses with acute-onset lameness had subchondral bone injury characterized by increased signal intensity in STIR and T2-weighted images.12 In two horses, decreased signal intensity in proton density images (similar to T1-weighted images) indicated the presence of sclerotic subchondral bone of the distal aspect of the MtIII, but dense bone was surrounded by areas of increased signal intensity in STIR sequences.12 Only two horses had bone scintigraphy performed, and areas of IRU in the damaged subchondral bone were seen.12 Horses with acute subchondral bone injury should improve with rest, whereas those with chronic, sclerotic, and osteoarthritic subchondral bone may improve temporarily with rest but long-term prognosis is guarded. MRI was useful in the evaluation of horses with oblique and straight distal sesamoidean desmitis in 27 horses with lameness localized to the metacarpophalangeal or MTP joint region, of which 17 had lameness and injury in the hindlimb.13 Careful examination of soft tissue structures associated with the MTP joint, including use of diagnostic ultrasonographic examination, is necessary, because in some horses the results of diagnostic analgesia will be ineffective at differentiating authentic sources of pain in the region.
Ultrasonographic Examination
Ultrasonographic examination of the MTP joint region is indicated for suspensory branch desmitis (see Chapter 72). The abaxial aspect of the PSBs should be examined carefully to identify tearing and small avulsion fractures. Proliferative synovitis (villonodular synovitis) is unusual in the MTP joint. The DDFT should be evaluated carefully if tenosynovitis of the DFTS is present14 (see Chapter 74). Ultrasonographic examination is useful in horses with intersesamoidean and collateral ligament injuries or those with wounds and draining tracts to look for foreign material or communication with the articular surface. The distal sesamoidean ligaments should also be examined carefully, because intraarticular analgesia of the MTP joint has the potential to resolve lameness associated with injury to these ligaments, which can be present with no localizing clinical signs.