Chapter 43The Metatarsal Region
Anatomy
The plantar surface of the MtIII and the origin of the SL are oblique and not parallel to the dorsal surface of MtIII. During ultrasonographic examination, care should be taken to account for obliquity and to position the transducer perpendicular to SL fibers (see Chapter 72). The SL is bordered by the MtII and the MtIV and is thus trapped within a bony and dense soft tissue encasement. In the midmetatarsal region the body of the SL can be palpated as it emerges from this bony encasement and courses distally to divide into the medial and lateral branches that attach to the abaxial border of each PSB. The accessory ligament of the DDFT (ALDDFT) is usually present and is a variably sized structure ranging from thin to thick and occasionally has two or three parts; in a small proportion of horses (10 of 165, or 6.1%) there was no identifiable ALDDFT.4 Although the ALDDFT is anatomically present in most horses, injury is rare (see Chapter 71). Desmotomy to manage flexural deformity is rarely performed and generally would be ineffective because of the small size of the ALDDFT. I examined an aged Quarter Horse gelding with enlarged ALDDFTs with unusual flexural deformity characterized by intermittent, dynamic heel elevation; during walking the heels would land flat, but during standing the heels elevated bilaterally (see Chapter 71). I severed the ALDDFT in each hindlimb, and although improvement was seen temporarily, flexural deformity recurred. The DDFT is located plantar to the SL for most of the metatarsal region, but in the proximal metatarsal region it is positioned plantaromedially. The SDFT is located plantar to both the SL and DDFT. Because the tarsal sheath ends in the proximal metatarsal region, distention can sometimes be palpated (see Chapter 76). The digital flexor tendon sheath (DFTS) begins in the plantar, distal third of the metatarsal region and encompasses the DDFT and SDFT (see Chapter 74).
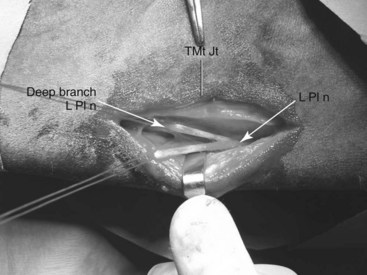
Distal continuation of the superficial fibular and saphenous nerves provides dorsal skin sensation. The tibial nerve divides to form the medial and lateral plantar nerves in the plantar tarsal region. The lateral plantar nerve, which courses plantar to the origin of the SL, gives off a deep branch that innervates the proximal aspect of the SL and gives off branches, which continue distally as the lateral and medial plantar metatarsal nerves that course on the axial aspects of each respective splint bone (see Figure 10-22; Figure 43-1). Neurectomy of the deep branch of the lateral plantar nerve provides analgesia of the origin of the SL and the plantar cortex of the MtIII and partial analgesia of sites more distal to the level of and including the metatarsophalangeal joint. Accurate interpretation of diagnostic analgesia is critical when planning this surgical procedure. Neurectomy has received considerable attention recently as a surgical approach for management of proximal suspensory desmitis (PSD; see later).5,6 Histological changes consistent with nerve compression have been identified in horses undergoing neurectomy of the deep branch of the lateral plantar nerve, and nerve compression was proposed as a possible cause of residual pain in horses even after desmitis resolved.6 In that study, 62% of horses returned to soundness after neurectomy,6 whereas in a different study 19 of 20 horses treated by neurectomy and laminar fasciotomy returned to the previous level of performance.5 The deep branch of the lateral plantar nerve that was examined histologically6 lies within the dense metatarsal but outside the laminar fascial planes. Recognition of neuritis in this segment indicates that compression of the deep branch may be occurring within this fascial compartment. The lateral plantar nerve and its counterpart, the medial plantar nerve, continue distally between the SL and DDFT.
Clinical Characteristics and Diagnosis of Lameness in the Metatarsal Region
There are no pathognomonic historical findings related to metatarsal region pain causing lameness. Palpation of the metatarsal region should be done with the horse in standing and non–weight-bearing positions. The metatarsal region cannot be adequately palpated when the horse is standing, because soft tissue structures in the proximal metatarsal region are not readily palpable in this position. Careful palpation for signs of inflammation and bony swelling should be performed with the limb in both positions. Even when the limb is flexed, it is still difficult to define the SL and DDFT proximally. However, it is possible to apply pressure over the proximal aspect of the SL to check for a painful response. In some horses with PSD, edema may be present or the area may feel full or slightly thickened, but dense fascia covering the SL and DDFT prevents expansion, and swelling may go undetected. A painful response to deep palpation over the proximal aspect of the medial splint bone and distal aspect of the tarsus, referred to as the Churchill test, may indicate the presence of referred pain and primary distal hock joint lameness, but in my experience this is a nonspecific test. Many horses with hindlimb lameness originating from sites other than the distal hock joints manifest a positive response to compression of both the medial and lateral splint bones and distal, medial aspect of the tarsus. Palpation of the dorsal cortex of the MtIII may reveal pain in trotters or other horses that interfere and may be an important finding, but palpation may not necessarily localize the primary source of pain that is causing lameness. Careful palpation of the abaxial and axial aspects of both splint bones is necessary to uncover hidden splint exostoses. Even subtle enlargement of the SL body, as it emerges from the bony encasement of the splint bones, that is accompanied by a painful response can indicate early suspensory desmitis. Both branches of the SL and attachments to the PSBs should be carefully palpated. Horses with a history of curb may develop progressive SDF tendonitis in the proximal metatarsal region, but this can easily be overlooked unless the area is carefully palpated (see Chapters 6, 69, and 78).
Diagnostic Analgesia
The high plantar perineural block (see Chapter 10) should be used to localize pain to the metatarsal region. Medial and lateral plantar nerves and medial and lateral plantar metatarsal nerves are blocked just distal (approximately 1.5 cm) to the tarsometatarsal joint (see Chapter 10). Variations of this block are often used, but it is important to recognize that subtarsal analgesic techniques targeting the lateral plantar nerve, or its deep branch, will not block the medial plantar nerve, and false-negative results could be obtained. More important, false-positive results incriminating the proximal aspect of the SL as a source of pain can occur. Subtarsal analgesia should be performed only after results of low plantar analgesia are observed, because most injection techniques in the subtarsal region are likely to desensitize the plantar metatarsal nerves, important contributors to innervation of the metatarsophalangeal joint. An injection technique was recently described for the diagnosis of PSD; the lateral plantar nerve is blocked approximately 15 mm distal to the head of the MtIV, just axial to the MtIV, at a depth of 25 mm.7 Although in theory this block is done in close proximity to the deep branch of the lateral plantar nerve, it is within the same fascial compartment as the parent branch, leading to the possibility of blocking this important contributor to distal limb innervation. If completed as a stand-alone technique without first performing low plantar analgesia, subtarsal analgesia may lead the clinician to the erroneous impression that pain is emanating from the proximal aspect of the SL. Management of horses with PSD by desmoplasty and fasciotomy was recently described, but criteria for inclusion of cases suggested that pain was localized to the proximal metacarpal or metatarsal region by use of only subcarpal or subtarsal analgesia without first blocking the distal aspect of the limb.8
Imaging Considerations
Routine radiographic examination includes the dorsoplantar (DPl), lateromedial (LM), dorsolateral-plantaromedial oblique (DL-PlMO), and dorsomedial-plantarolateral oblique (DM-PlLO) images. In a DPl image of the proximal aspect of the MtIII, there is a normal area of mild increased radiopacity that should not be interpreted as modeling that is associated with stress reaction of the origin of the SL (Figure 43-2). Accurate assessment of the proximal aspect of the MtIII for the presence of increased radiopacity or avulsion fracture requires that radiographic views be centered at this level.
Pool and delayed (bone) phase scintigraphic examination is quite useful to differentiate bone from soft tissue injury in horses with proximal plantar metatarsal pain and osteoarthritis. It is also useful to differentiate other conditions of the tarsometatarsal joint from those involving the proximal aspect of the MtIII. Focal increased radiopharmaceutical uptake (IRU) seen in delayed (bone) phase images involving the proximal plantar aspect of the MtIII is the most important scintigraphic finding in the metatarsal region. In TB and STB racehorses there is normally mild to mild-moderate IRU of the dorsal cortex of the MtIII, from the most proximal aspect to the mid-to-distal diaphysis. This finding was originally proposed to be age dependent because the dorsal cortex of the McIII could be “seen” scintigraphically as a normal finding in young but not older TB racehorses.11 In a population of predominantly sports horses and few racehorses the dorsal cortex was evident visually and with use of profile analysis in all horses regardless of age.12 When normal plantar scintigraphic images of the proximal metatarsal region are evaluated, there is usually asymmetrical radiopharmaceutical uptake (RU), with greater RU of the lateral aspect involving the lateral aspect of the MtIII and the MtIV. A central area of increased radiopacity seen radiologically (see Figure 43-2) does not appear to be active scintigraphically in normal horses. Asymmetrical RU was confirmed in a recent scintigraphic study of the proximal metacarpal and metatarsal regions in normal horses.13 Using region of interest analysis there was significantly higher RU in the lateral aspect of the metatarsal region compared with the medial aspect in plantar images, and significantly higher RU in the right proximal metatarsal region compared with the left. In lateral images there was maximum RU in the central and plantar aspect of the proximal metatarsal region. There was no effect of age on RU.13 In horses with PSD, visual appraisal and profile analysis of scintigraphic images failed to reveal abnormalities in most of 126 horses with forelimb or hindlimb lameness, but quantitative analysis using region of interest analysis revealed greater RU ratios in plantar images of lame limbs compared with nonlame limbs.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree