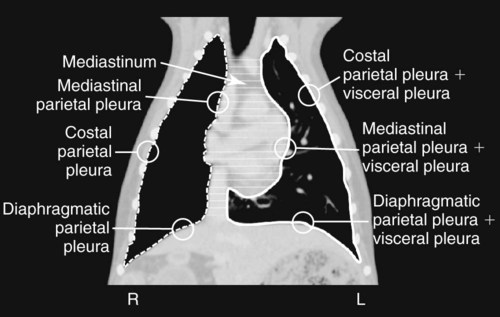
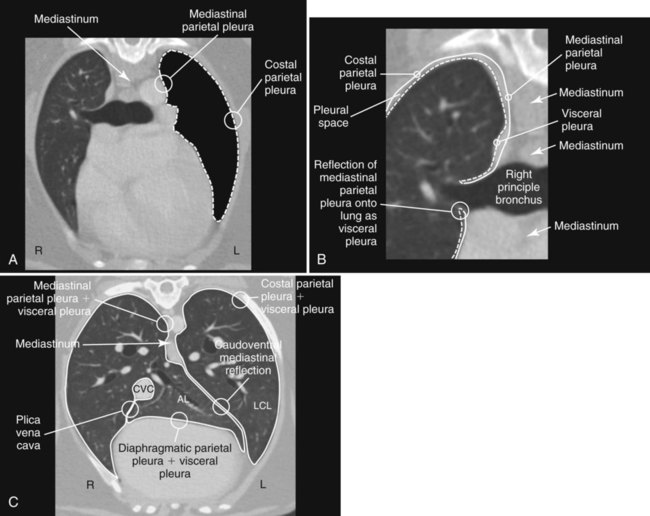
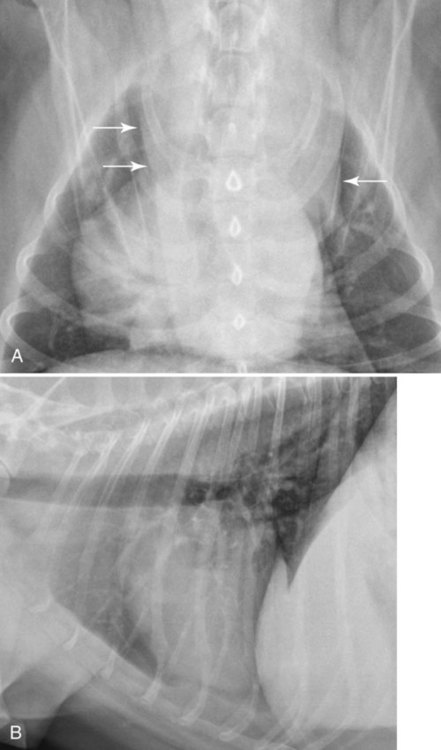
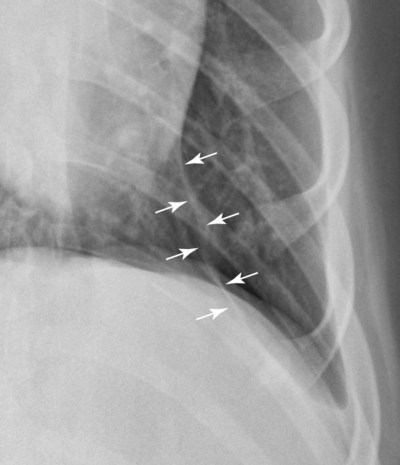
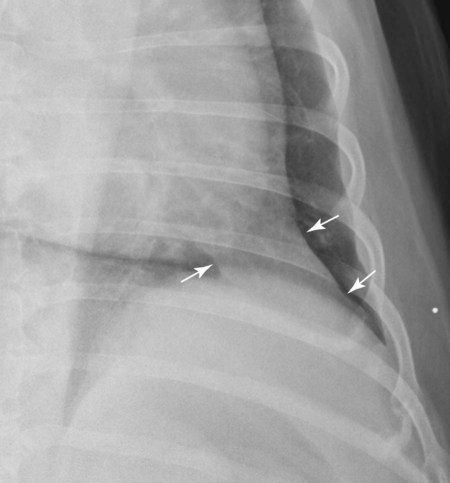
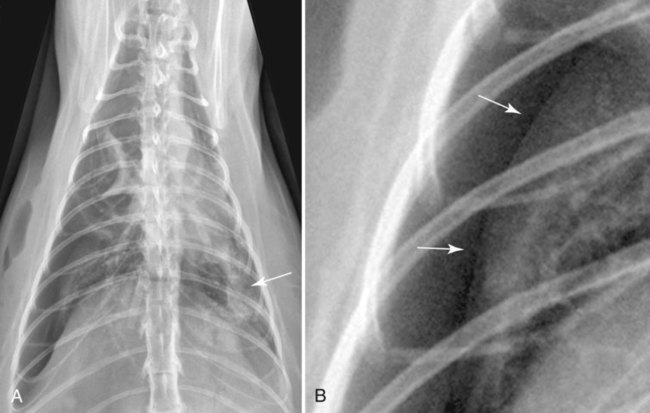
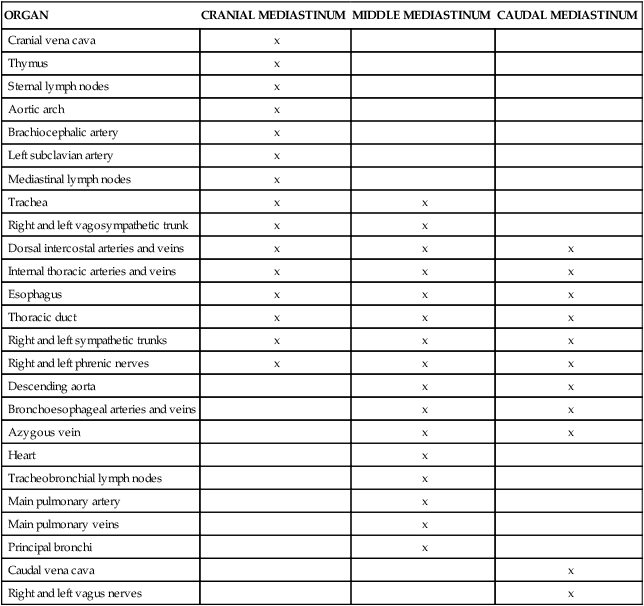
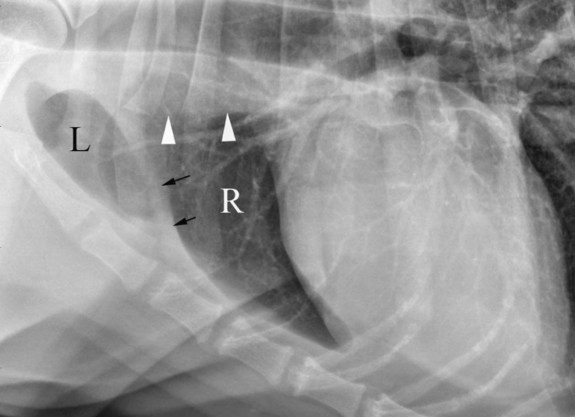
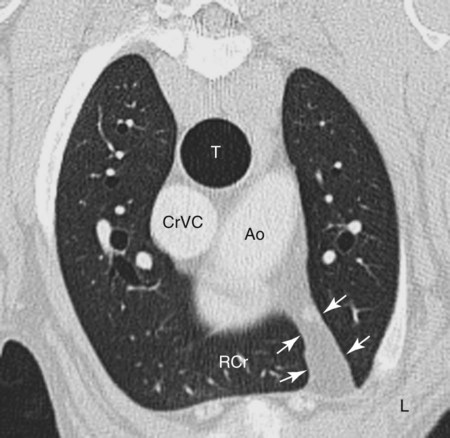
The mediastinum, which is the region between the right and left pleural sacs, contains many important organs and structures (Table 30-1). The mediastinum is bounded on each side by a layer of mediastinal pleura. The mediastinal pleural is just one part of each pleural sac. An understanding of pleural morphology is required to fully comprehend the morphologic aspects of mediastinal disease (Figs. 30-1 and 30-2). Table • 30-1 Each right and left pleural sac is composed of parietal and visceral pleura. Parietal pleura is further designated as costal, diaphragmatic, or mediastinal parietal pleura, depending on the tissue or compartment that it covers. Visceral pleura covers the lung. At the hilus of the lung, the mediastinal parietal pleura is reflected onto the surface of the lung to become visceral pleura (see Fig. 30-2); thus the parietal and visceral pleural layers are continuous and form the left and right pleural sacs. The mediastinum extends from the thoracic inlet to the diaphragm and is located mainly in the midsagittal plane of the thorax, thereby dividing the thoracic cavity into right and left halves (see Figs. 30-1 and 30-2). The mediastinum may be subdivided into a cranial portion cranial to the heart, a middle portion at the level of and containing the heart, and a caudal portion caudal to the heart. The mediastinum may also be divided into dorsal and ventral portions by a dorsal plane through the tracheal bifurcation. The mediastinum communicates cranially with the fascial planes of the neck by way of the thoracic inlet and caudally with the retroperitoneal space through the aortic hiatus. These communications provide the means for the spread of mediastinal disease to the neck and abdomen, and vice versa. In most dogs and cats, the mediastinal pleura does not form an effective anatomic separation between the left and right sides of the thoracic cavity. Normal mediastinal pleural layers are fragile and contain fenestrations. Thus, pleural fluid or gas occurring unilaterally is not usually contained to one side by the mediastinum. For example, in a study of induced pneumothorax, 22 of 24 dogs having air injected into one pleural space quickly developed bilateral pneumothorax.1 Pleural fluid or gas may remain unilateral if (1) the mediastinal pleura is not fenestrated, and the mediastinal pleura remains intact; (2) any existing fenestration becomes closed as a result of inflammation or plugging; or (3) the pleural fluid is too viscid to pass through an existing mediastinal fenestration. Of all of the structures in the mediastinum (see Table 30-1), only the heart, trachea, caudal vena cava, aorta, and, in young animals, thymus are visible normally. Occasionally, a portion of the normal esophagus may be seen (see Chapter 27). The other mediastinal structures are not seen normally either because (1) they are too small or (2) insufficient fat is interposed between them to provide contrast, leading to border effacement. The normal homogeneous appearance of the cranial mediastinum in a lateral thoracic radiograph is the result of border effacement. Cranial mediastinal structures in this region create a homogeneous opacity ventral to the trachea, but individual structures cannot be discerned (Fig. 30-3). This homogeneous opacity ventral to the trachea is caused by the collective opacity of the left subclavian artery, brachiocephalic trunk, cranial vena cava, and mediastinal lymph nodes. These structures are not seen individually because they are in contact with each other and insufficient interposed fat is present. Thus the border of these structures is effaced. The cranioventral mediastinum is more radiopaque ventral to the trachea than dorsal to the sternum on a lateral thoracic radiograph because it is thicker just ventral to the trachea (Fig. 30-4). In ventrodorsal (VD) or dorsoventral (DV) thoracic radiographs, most of the cranial mediastinum is superimposed on the spine—that is, in the midsagittal plane of the thorax. The normal width of the cranial mediastinum in VD or DV views is usually less than approximately twice the width of the vertebral column (Fig. 30-5). In obese patients, the cranial mediastinum may become enlarged because of fat accumulation and be confused with an abnormal mediastinal mass (Fig. 30-6). Other imaging modalities, such as ultrasound or computed tomography (CT), may be necessary to distinguish fat from a mass as a cause for a widened mediastinum in obese patients. The cranioventral mediastinal reflection appears in VD or DV radiographs as a curving radiopaque line, on the patient’s left, extending from approximately T1 or T2 to the region of the main pulmonary artery. The concave side of the line is to the patient’s right (see Figs. 30-4 and 30-5). As already noted, the cranioventral mediastinal reflection is caused by extension of the right cranial lobe across the midline, pushing the mediastinum to the left (see Fig. 30-4). The thickness of the cranioventral mediastinal reflection is affected by the amount of fat it contains (see Fig. 30-6). On the lateral view, the cranioventral mediastinal reflection is often identified approximately midway between the thoracic inlet and the heart (see Fig. 30-3). The thymus lies in the cranioventral mediastinal reflection, and sometimes a subinvoluted thymus can be identified in VD or DV radiographs of young animals (Fig. 30-7). An incompletely involuted thymus is not usually visible in lateral thoracic radiographs. The internal thoracic arteries and veins are also located in the cranioventral mediastinal reflection. The caudoventral mediastinal reflection is seen only on VD or DV radiographs; it is not seen in lateral projections. It is created by extension of the accessory lobe of the right lung across the midline to the left, thereby pushing the mediastinum to the left (see Fig. 30-2). The caudoventral mediastinal reflection therefore consists of four pleural layers: (1) the visceral pleura of the accessory lobe, (2) the mediastinal parietal pleura of the right pleural sac, (3) the mediastinal parietal pleura of the left pleural sac, and (4) the visceral pleura of the left caudal lobe (see Fig. 30-2). The caudoventral mediastinal reflection appears as a relatively straight radiopaque line in the caudal left hemithorax, extending from the region of the cardiac apex in a caudolateral direction toward the gastric fundus (Fig. 30-8). The caudoventral mediastinal reflection has been incorrectly termed the sternopericardiac ligament (also called the cardiophrenic or phrenicopericardial ligament), but the sternopericardiac ligament, which is a continuation of the apex of the fibrous pericardium, is not visible radiographically.2 The thickness of the caudoventral mediastinal reflection depends on the amount of fat it contains (Fig. 30-9); this thickness can change in individual animals as body habitus changes. Mediastinal shift occurs as a result of a unilateral decrease in lung volume (ipsilateral mediastinal shift), a unilateral increase in lung volume (contralateral mediastinal shift), the presence of an intrathoracic mass (contralateral mediastinal shift), or unilateral increased pleural pressure (contralateral mediastinal shift). A mediastinal shift is detected in VD or DV radiographs by noting a change in position of visible mediastinal organs or the position of mediastinal reflections. Displacement of the heart to the left or right is the most reliable sign of a mediastinal shift (Fig. 30-10). Improper patient positioning with rotation of the sternum to the right or left will create the false impression of a mediastinal shift. Detection of a mediastinal shift is often the first clue of a thoracic abnormality (Fig. 30-11). Pulmonary atelectasis, resulting from reduced ventilation or prolonged lateral recumbency, is the most common cause of a mediastinal shift. Atelectasis will result in decreased lung volume and increased lung opacity, and the heart will be shifted toward the abnormally opaque lung. Distinguishing normal atelectatic from diseased atelectatic lung is not possible radiographically (see Fig. 30-11).
The Mediastinum
Normal Anatomy
ORGAN
CRANIAL MEDIASTINUM
MIDDLE MEDIASTINUM
CAUDAL MEDIASTINUM
Cranial vena cava
x
Thymus
x
Sternal lymph nodes
x
Aortic arch
x
Brachiocephalic artery
x
Left subclavian artery
x
Mediastinal lymph nodes
x
Trachea
x
x
Right and left vagosympathetic trunk
x
x
Dorsal intercostal arteries and veins
x
x
x
Internal thoracic arteries and veins
x
x
x
Esophagus
x
x
x
Thoracic duct
x
x
x
Right and left sympathetic trunks
x
x
x
Right and left phrenic nerves
x
x
x
Descending aorta
x
x
Bronchoesophageal arteries and veins
x
x
Azygous vein
x
x
Heart
x
Tracheobronchial lymph nodes
x
Main pulmonary artery
x
Main pulmonary veins
x
Principal bronchi
x
Caudal vena cava
x
Right and left vagus nerves
x

Pathologic Mediastinal Conditions
Mediastinal Shift
The Mediastinum