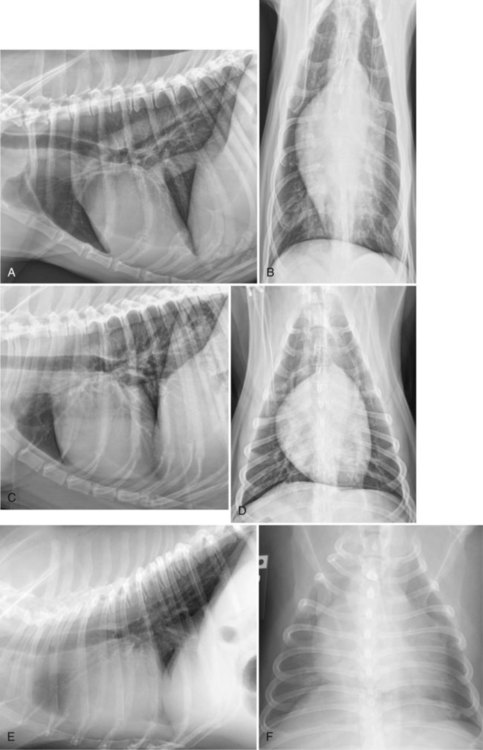
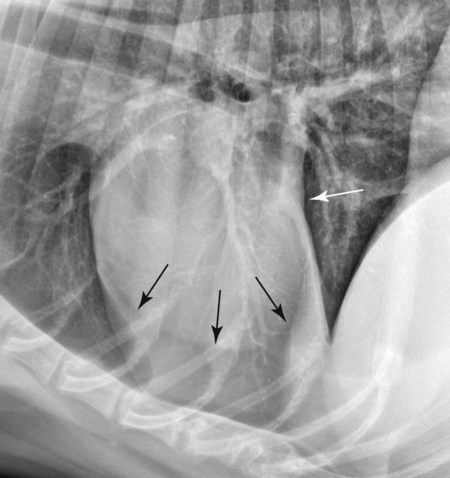
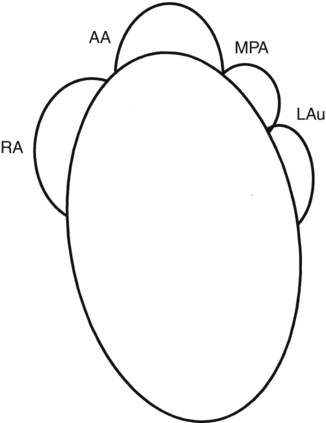
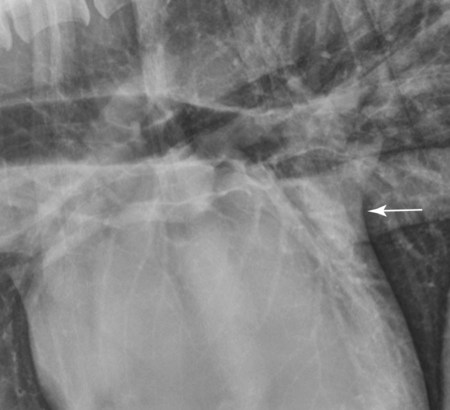
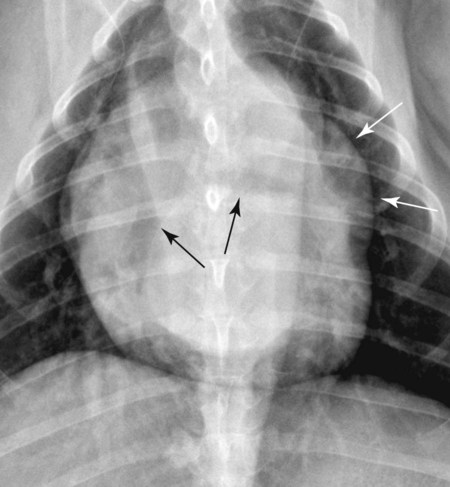
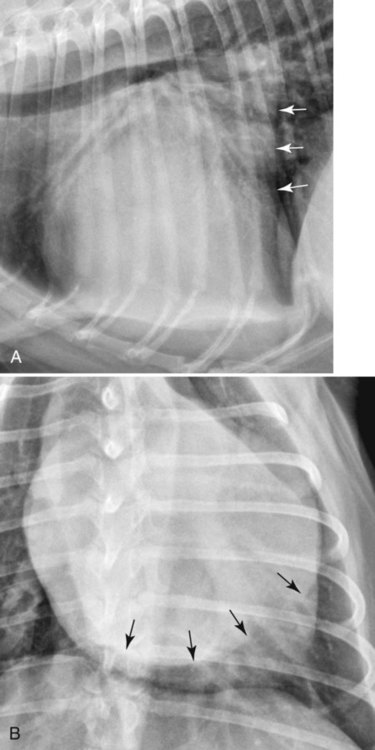
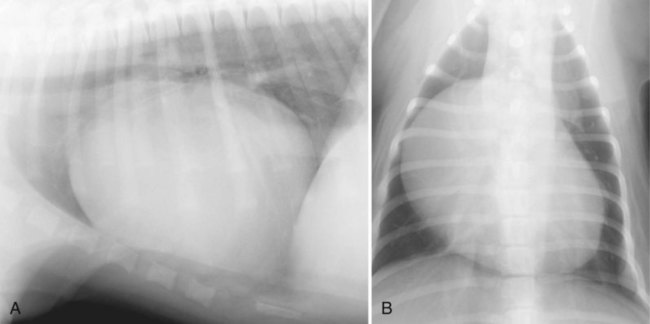
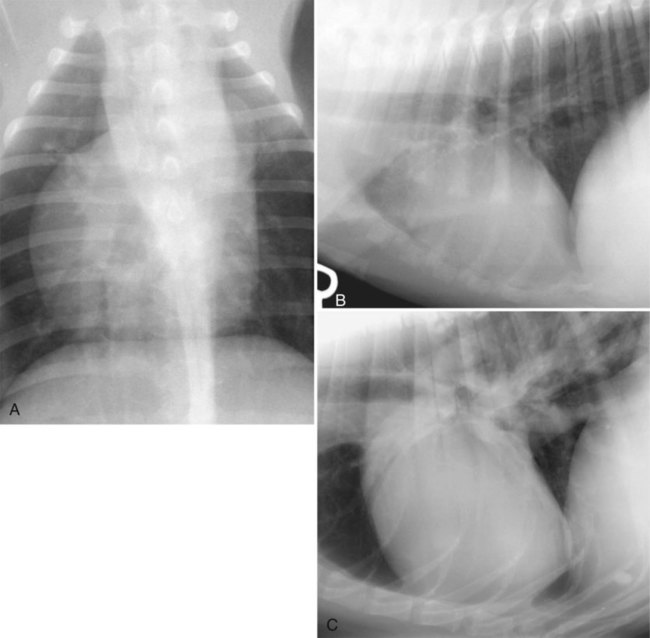
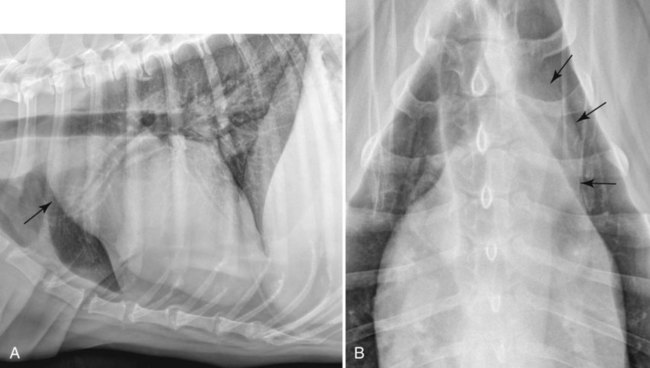
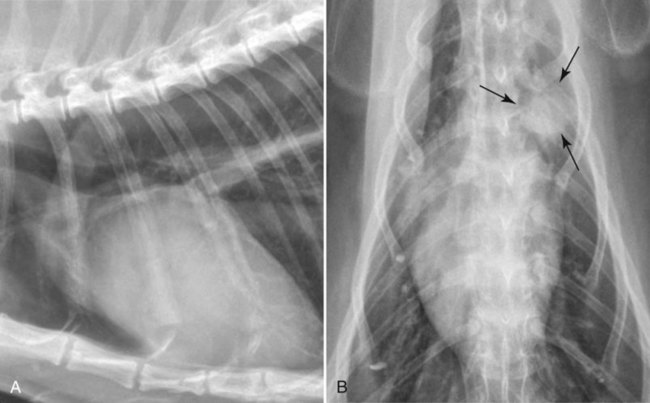
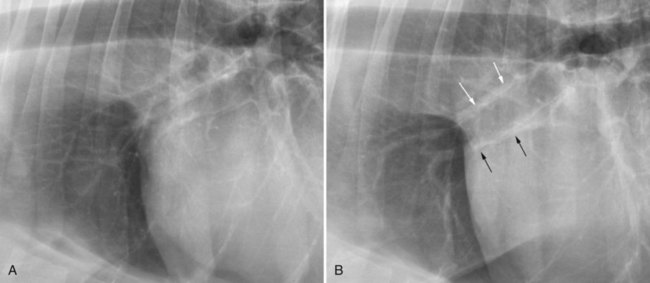
Assessing cardiovascular function becomes important when decisions must be made regarding staging a patient with suspected cardiac disease, deciding about therapy, and monitoring response to therapy or progression of disease. Unfortunately, radiographs are not very accurate for assessing either cardiovascular function or morphology because the range of the normal cardiac appearance is very wide in dogs and the appearance of the cardiac silhouette is affected by radiographic positioning.1–4 See Chapter 25 for a comprehensive discussion of these issues With regard to the wide range of the normal cardiac appearance, muscular dogs or those with a barrel-shaped thorax often have a heart that looks large. Conversely, the normal heart in breeds with a laterally compressed but deep thoracic cavity, such as greyhounds and collies, can look abnormally small (Fig. 32-1). Thus the breed and body physique of the dog should always be considered when the heart is evaluated radiographically. If any suspicion of a cardiac abnormality exists, because of either radiographic appearance or clinical or historical information, then echocardiography should be performed.5 Radiographic positioning can have a profound effect on the appearance of the cardiac silhouette (see Chapter 25).3 Perhaps the most important effect is the difference in cardiac silhouette appearance in ventrodorsal (VD) versus dorsoventral (DV) radiographs. In DV radiographs, the diaphragm is displaced cranially, which will physically push the heart cranially and into the left hemithorax. The magnitude of this displacement is more pronounced in medium and large dogs than in cats or small dogs (Fig. 32-2).6 Alternately, VD views of the heart in large-breed dogs will have significant magnification when compared with DV views of the same heart. It is important to realize that the cardiac silhouette is composed of tissues other than the heart. The pericardium, any fluid or tissue in the pericardial space, and any tissue or fluid in the mediastinum immediately adjacent to the heart will blend with the heart, thereby contributing to the overall size and shape of the cardiac silhouette. This principle is perhaps most important when attempting to assess heart size in obese patients because fat in the mediastinum silhouettes with the heart, increasing the size of the cardiac silhouette. Occasionally, this fat will be visible as a region of decreased opacity immediately adjacent to the heart (Fig. 32-3). Despite these normal variations, a starting point for radiographic evaluation is necessary. In this chapter, the qualitative radiographic signs of enlargement are discussed for each heart chamber, the aorta, and the caudal vena cava. A quantitative method of cardiac measurement, called the vertebral heart scale, has been devised to take into account the inherent breed variation in cardiac size.7 In this method, the length of the long and short axis of the heart is measured, summed, and scaled against the length of the vertebral bodies dorsal to the heart, beginning with T4, to quantify heart size. Based on 100 clinically normal dogs, the mean normal vertebral heart scale was 9.7 vertebrae, with a standard deviation of 0.5 vertebrae. By definition, 95% of any normal population lie within the mean plus or minus two standard deviations of the mean; therefore the normal vertebral heart scale ranges from 8.7 to 10.7 vertebral body lengths. The span of this range is too wide for it to be of use in an individual patient, and it has not proved superior to subjective radiographic assessment of heart size.8,9 There is also variation between readers in the transformation of long- and short-axis dimensions into vertebral heart scale units.10 Perhaps the best use of the vertebral heart scale is to compare cardiac size on radiographs of the same patient made on different dates to monitor disease progression or response to treatment.11,12 For ease of recognition of various parts of cardiac anatomy as well as certain cardiac abnormalities in the DV or VD radiograph, the cardiac silhouette can be visualized in terms of a clock face. The origin of bulges on the cardiac silhouette caused by dilation of different parts of the heart or great vessels can be predicted by using this clock analogy (Fig. 32-4). In the lateral view, dilation of the left atrium causes a change in shape of the dorsocaudal aspect of the cardiac silhouette. Rather than this region of the heart coursing in a dorsal and cranial direction toward the tracheal bifurcation, it tends to course more in a dorsal or dorsocaudal direction, with the formation of a slight concavity on the caudal margin of the heart (Fig. 32-5; see Fig. 32-3). This shape change has been referred to as loss of the caudal cardiac waist, but the normal cardiac waist is not well defined, and this term is best avoided. Left atrial dilation also causes an increase in height of the caudodorsal heart border and elevation of the tracheal bifurcation. If left atrial dilation is severe, the left principal bronchus may become selectively elevated or even compressed between the left atrium and adjacent tissues dorsally (Fig. 32-6). Dogs with bronchial compression secondary to left atrial dilation may exhibit a cough, which may lead the clinician to think erroneously that the patient is in heart failure. Dilation of the left atrium may also cause divergence of the principal bronchi in the VD or DV view. This appearance is similar to the bronchial displacement occurring secondary to tracheobronchial lymph node enlargement as described in Chapter 30 (see Fig. 30-20), with the normal acute angle between the principal bronchi appearing wider because of the interposed enlarged lymph nodes (Fig. 32-7). A massively dilated left atrium may also lead to a region of increased opacity superimposed over the cardiac silhouette in the VD or DV view that creates the appearance of a double wall. This is caused by a summation effect of the enlarged left atrium being projected superimposed on the remainder of the heart (Fig. 32-8). Dilation of the left atrial appendage (auricle) occurs less frequently than dilation of the left atrium and, when present, appears as a focal bulge along the left cardiac border in the 2 to 3 o’clock position according to the clock face analogy (see Fig. 32-7). An extremely enlarged left atrium can also result in lateral displacement of the left auricle, resulting in its visualization without the auricle actually being dilated. Radiographic detection of an enlarged right atrium is uncommon. Visualization of isolated right atrial enlargement can be found in dogs with tricuspid dysplasia. As with the left atrium, enlargement of the right atrium is usually caused by dilation. When visible in the lateral view, right atrial enlargement causes a bulge or mass effect in the craniodorsal aspect of the cardiac silhouette. However, other cardiovascular enlargements, including dilation of the aortic arch and main pulmonary artery, can also cause this radiographic appearance. In the VD or DV projection, an increased bulge in the right heart border from the 9 o’clock to 11 o’clock position may be present (Fig. 32-9). As with the left ventricle, the right ventricle may enlarge as a result of hypertrophy or dilation. Common causes of hypertrophy are heartworm infection and pulmonic stenosis. Hypertrophy mainly occurs at the expense of lumen volume and may lead to no or unrecognizable radiographic signs. However, radiographs are more sensitive for detection of right ventricular hypertrophy than for left ventricular hypertrophy; this may be related to the normally thinner wall of the right ventricle, with hypertrophy then causing more obvious changes in cardiac size and shape. Because the right ventricle is normally in contact with the sternum, its enlargement, whether from dilation or hypertrophy, often causes an increased sternal contact in the lateral view (Fig. 32-10, B). The average dog has an amount of cardiac contact with the sternum ranging from 2.5 to 3 intercostal spaces; thus sternal contact in excess of 3 intercostal spaces suggests right ventricular enlargement. Some deep-chested breeds, such as Doberman pinschers and Irish wolfhounds, may normally have only approximately 1.5 to 2 intercostal spaces of sternal contact, so 2.5 to 3 spaces would be consistent with right ventricular enlargement for those breeds. Likewise, some barrel-chested breeds, such as the bulldog, can normally have more than 3 to 3.5 intercostal spaces of contact. Right ventricular hypertrophy can also lead to the cardiac apex being displaced dorsally from the sternum in lateral views (Fig. 32-10, C). In VD or DV views, a hypertrophic right ventricle appears more rounded and protrudes farther into the right hemithorax than normal, giving the cardiac silhouette a reversed letter D shape (Fig. 32-10, A). It is important not to confuse this with the normal shape of the heart in VD and DV views, which might also be described as a reversed letter D shape. Generalized enlargement of the cardiac silhouette results from combinations of chamber enlargement, or all four chambers may be enlarged. Myocardial dysfunction is a common cause of generalized cardiomegaly. Subjectively, the cardiac silhouette appears larger than expected, but specific chamber enlargement may or may not be evident. Generalized cardiomegaly may also be misinterpreted because of underinflation of the lungs, making the thoracic cavity appear smaller than normal. This, in turn, makes the heart appear larger relative to the amount of aerated lung surrounding it. This was discussed in detail in Chapter 25.7 Echocardiography should be used to confirm a cardiac abnormality when generalized cardiomegaly is suspected radiographically. The caudal vena cava is extremely variable in size depending on the phase of respiration and cardiac cycle. It can be judged to be enlarged only if it is consistently larger in diameter than the length of the fifth or sixth thoracic vertebral bodies of the spine as measured in the lateral view. Another measure of caudal vena cava size is that enlargement can be inferred only if the diameter of the caudal vena cava is more than 1.5 times the diameter of the descending aorta.13 The caudal vena cava can enlarge in response to increased central venous pressure, but the size of the vena cava is not an accurate way to attempt to assess central venous pressure. Valid inferences on cardiovascular disease cannot typically be made on the basis of the size of the caudal vena cava only. Widening of the precardiac mediastinum, as seen in the VD or DV views, can indicate dilation of the aortic arch. A focal bulge in the descending aorta in VD or DV views can be seen in patients with aortic stenosis and patent ductus arteriosus (Fig. 32-11). In the lateral views, an enlarged aortic arch can create increased mass at the cranial aspect of the cardiac silhouette (see Fig. 32-11). Some older cats will have a tortuous appearing aorta in the lateral view, with a more vertical aortic arch orientation. The aortic arch then curves upward and caudally, assuming a serpentine contour as it progresses caudally toward the diaphragm (Fig. 32-12, A). In the DV or VD views, this aortic contour may be projected away from the mediastinum and be misinterpreted as a pulmonary nodule when projected end-on (Fig. 32-12, B).14 A tortuous aorta is clinically insignificant in aged cats. The main pulmonary artery is not seen normally as a separate structure, but when it dilates sufficiently in dogs, it will appear as a focal bulge in the 1 o’clock position in VD or DV views (Fig. 32-13). A dilated main pulmonary artery is not recognized routinely in lateral views. Common causes of main pulmonary artery dilation include pulmonary hypertension, as from heartworm infection, and turbulence, as from pulmonic stenosis or patent ductus arteriosus. In lateral projections, when arteries can be seen as separate structures from veins, the arteries are dorsal and veins are ventral to the intervening bronchus.15 This applies mainly to cranial lobe arteries and veins because the caudal lobar arteries and veins are superimposed in the lateral projection and caudal lobe pulmonary arteries cannot be differentiated from veins in the lateral projection. The right cranial lobar pulmonary artery and vein can serve as reference vessels because they are best seen as individual structures when the animal is placed in left lateral recumbency (Fig. 32-14).3 This is because the right cranial lung lobe is better inflated with the animal in left recumbency, resulting in better definition of these vessels. Although the left cranial lobe will be better inflated in right recumbency, the left and right pairs of cranial lobe vessels will be more superimposed in that particular view, making their assessment more difficult (see Fig. 32-14).
The Heart and Pulmonary Vessels
Radiographic Signs
Radiographic Signs of Specific Cardiac Chamber Enlargement
Left Atrium
Right Atrium
Right Ventricle
Generalized Cardiomegaly
Radiographic Signs of Major Vessel Enlargement
Caudal Vena Cava
Aorta
Main Pulmonary Artery
Radiographic Signs of Pulmonary Vascular Changes

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Heart and Pulmonary Vessels