Chapter 26 The Genus Francisella
Francisella tularensis was isolated in 1912, during studies of a plaguelike disease in rodents in Tulare County, California, from which the specific name is derived. This organism spent many decades in the genus Pasteurella, but was reclassified in 1947 into a new genus named for Edward Francis, a U.S. Public Health Service physician who first cultivated the organism and described its transmission and the clinical syn dromes resulting from infection. Tularemia (rabbit fever, hare fever, deerfly fever, lemming fever, or Ohara’s disease) remains an important zoonosis, as well as a primary pathogen of wild and domestic animals. The high infectivity of F. tularensis, its ready dissemination by aerosol, its ability to cause severe respiratory disease, and its documented weaponization by various biological warfare programs worldwide have led to its classification as a Category A select agent. Before and during World War II, Japanese research units studied weaponization of F. tularensis, as did the United States from the war’s end until biological weapons programs were dismantled in 1969.
DISEASE
Based on both 16S rDNA sequence comparisons and DNA–DNA hybridizations, F. tularensis has no close relatives, although the family Francisellaceae is relatively closely related to Piscirickettsia salmonis and ciliate and tick endosymbionts. The most closely related human pathogens (which are nonetheless distant) are Coxiella burnetii and Legionella spp., both of which have lifestyle similarities with F. tularensis.
Tularemia can take multiple clinical forms, depending on the portal of entry (Table 26-1). On the whole, it is plaguelike, and the infectious dose of highly virulent strains is astonishingly low, at only 10 to 50 colony-forming units. Most human cases result from arthropod bites (usually mosquitoes and ticks) previously fed on infected animals. If bacterial replication in skin at the point of entry causes formation of a distinct ulcer (Figure 26-1), the ensuing disease is called ulceroglandular tularemia. Organisms are transported from the ulcer to regional lymph nodes, where subsequent lesions resemble the buboes encountered in plague. Flulike signs appear after an incubation period of 3 to 5 days, with malaise, chills and fever, headache, sore throat, and myalgia; early misdiagnosis is common as a result of symptom nonspecificity. The organism may disseminate from the lymph node lesions to other sites throughout the body, including the lungs, in which case secondary pneumomic tularemia can result. Glandular tularemia is similar, but without an obvious route of entry. Glandular and ulceroglandular tularemia are the most common forms of the disease in humans. Hunters, trappers, and others in contact with infected animals or with arthropod vectors are the highest-risk groups, and infection is rarely fatal. Infection with low-virulence strains probably goes frequently undiagnosed.
TABLE 26-1 Clinical Syndromes Associated with Francisella tularensis Infection
| Syndrome | Description |
|---|---|
| Ulceroglandular | Mucosal or other epithelial ulcer, extension to lymph nodes |
| Glandular | Lymph node infection without apparent local ulceration |
| Oropharyngeal | Localized to oropharynx; necrotizing lesions of pharynx and upper digestive tract, gastrointestinal symptoms |
| Oculoglandular | Localized to eye; conjunctivitis, regional lymphadenopathy |
| Primary pneumonic | Lung infection following inhalation |
| Typhoidal | Fever, abdominal pain, prostration; no skin involvement, no lymphadenopathy; primary intestinal infection? dissemination from mesenteric lymph nodes? |
| All forms | Secondary pleuropneumonic involvement, meningitis, sepsis |
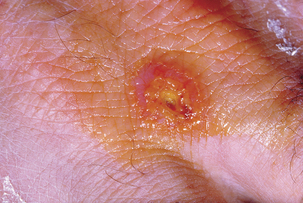
FIGURE 26-1 Ulcer caused by Francisella tularensis on the hand.
(Courtesy Public Health Image Library, PHIL #2037, Centers for Disease Control and Prevention, Atlanta, 1963, P. Brachman.)
Clinical disease in livestock is rare. Natural infection has occurred in captive nonhuman primates, including squirrel monkeys, black and red tamarins, talapoins, and a lowland gorilla, all with depression, anorexia, vomiting, diarrhea, lymphadenopathy, and petechial hemorrhage.



