CHAPTER 43 The Eye
The Ophthalmic Examination
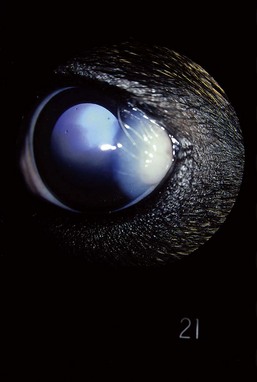
Examination of the neonate must take into account age-related variations in ocular appearance and response. Generally the eyelids open at 10 to 14 days of age, revealing a cloudy cornea that begins to clear within 24 hours. The patient should demonstrate a blink in response to a bright light when the lids open. Pupillary light reflexes are present within 24 hours of eyelid separation but remain sluggish for 3 weeks. Vision and menace responses are generally poor for the first 3 weeks and may not reach adult standards until 6 to 8 weeks of age. Reflex lacrimation begins when the eyelids open. Box 43-1 summarizes additional features of the neonatal eye.
BOX 43-1 Normal features of the immature canine and feline eye
| Eyelids | Separate at 10-14 days |
| Globe position | Kittens demonstrate subtle divergent strabismus until 3-4 weeks |
| Tear film | Reflex tearing is present when eyelids separate |
| Cornea | Mild corneal edema begins to clear within 24 hours after eyelids open; corneal thickness continues to decrease until 6 weeks of age |
| Iris | Newborn blue-gray iris shows signs of adult coloration by 1 month of age; persistent pupillary membranes are seen until 6 weeks of age in puppies and 3 weeks of age in kittens |
| Lens | Vessels of the tunica vasculosa lentis are seen until 4 weeks of age |
| Fundus | The blue-gray tapetum gradually assumes adult coloration by 4 months of age; the optic disc appears smaller because of incomplete myelination, but caliber and distribution of retinal vessels are similar to adult |
| Vision/menace reflex | Visual reflexes are poor at 3 weeks of age, gradually improving until 6-8 weeks of age, as retina continues to differentiate |
| Pupillary light reflexes | Present within 24 hours of lid separation but sluggish until the retina matures during week 4 |
| Dazzle reflex | Present when eyelids open |
The Globe and Orbit
Congenital Abnormalities
Microphthalmia
Failure of the eye to develop to normal size is referred to as microphthalmia. The small globe is often associated with a correspondingly small palpebral fissure. Depending on the constellation of accompanying defects, vision may be normal, diminished, or absent. Microphthalmia with multiple colobomas is an autosomal recessive trait linked to merling in the Australian Shepherd (Figure 43-1).
Acquired Abnormalities
Traumatic Proptosis
Complete displacement of the eye from the orbit is most commonly seen in brachycephalic dogs, but any dog or cat may present with proptosis with sufficient cranial trauma (Figure 43-2). A completely displaced eye is a true ocular emergency. Prognosis for vision is always poor because of optic nerve injury, but the intact globe may be salvaged cosmetically.
The Eyelids
Congenital Abnormalities
Eyelid Agenesis
Eyelid agenesis occurs primarily in cats as a unilateral or bilateral anomaly. The condition is characterized by absence of the eyelid margin, almost always involving the lateral one third to two thirds of the upper eyelid (Figure 43-3).

Figure 43-3 Eyelid agenesis. The superior temporal lid margin is absent in this 6-month-old Domestic Shorthair cat.
Entropion
Inversion of the eyelid margin occurs commonly in dogs but infrequently in the cat. The lower eyelid is more often affected. Accompanying clinical signs include increased tearing, squinting, corneal vascularization, and ulceration (Figure 43-4).
Young animals with entropion but without corneal disease may be treated palliatively with an ophthalmic lubricant ointment to postpone surgery until the patient matures. Delaying surgery in the Shar-Pei may not be possible because of the severity of the breed’s entropion and the risk of corneal ulceration. Temporary “tacking” is used to evert the lid margins and forestall corneal damage. The procedure is most effective when performed in the 3- to 4-week-old puppy. The older the animal is when tacking is first performed, the less likely it will be to correct the entropion without additional surgery. Local anesthetic blocks can be used in the very young animal, but masking the patient with isoflurane expedites the procedure. The first bite of a 5-0 nylon vertical mattress suture enters 2 mm from the eyelid margin and engages about 4 mm of eyelid skin and subcutaneous tissue. Avoid suturing the eyelid margin directly because postsurgical notching can irritate the cornea. The needle is then reinserted into the skin and deeper tissue overlying the orbital rim, adjusting the tension to evert the eyelid margin in a slightly overcorrected position (Figure 43-5).
Ectopic Cilia
Occasionally cilia will penetrate through the conjunctiva lining the underside of the eyelid rather than emerge from the meibomian gland opening. The classical presentation is a young dog with a nonhealing superficial ulcer in the dorsal third of the cornea. Some dogs intermittently squint and tear but never ulcerate. The upper eyelid is more commonly affected. Magnification is required to demonstrate the small dark spot at the base of the meibomian gland that represents the tip of the emerging cilia (Figure 43-6).
En bloc resection of the palpebral conjunctiva and the affected meibomian gland is curative.
The Conjunctiva
Congenital Abnormalities
Dermoid
A dermoid is a congenital mass of tissue containing skin, hair follicles, and sebaceous glands (Figure 43-7). It most commonly occurs in the temporal perilimbal conjunctiva and may also involve the adjacent eyelid and cornea.