Chapter 33 The Distal Phalanx and Distal Interphalangeal Joint
 Primary Pain Associated with the Distal Interphalangeal Joint
Primary Pain Associated with the Distal Interphalangeal Joint
Diagnosis
Imaging Techniques
Radiography
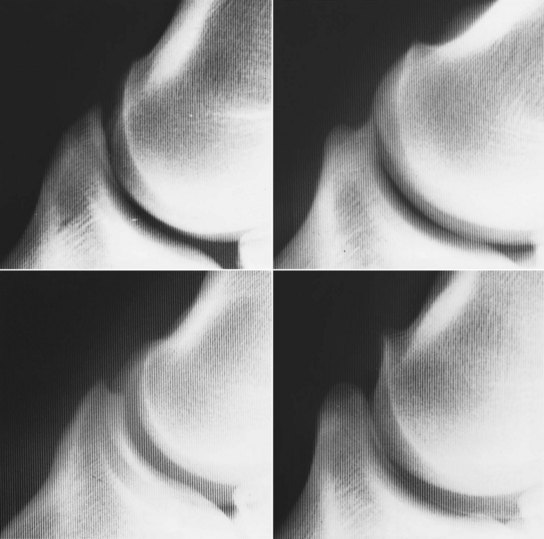
The shape of the extensor process of the distal phalanx varies considerably among horses on lateromedial images (Figure 33-1), but the shape usually is bilaterally symmetrical.10 Modeling changes of the extensor process can be present without associated lameness. Care should be taken in interpretation of the bony prominences on the distal medial and lateral aspects of the middle phalanx, which always appear larger in bigger-boned horses. Entheseous new bone at the origins of the collateral ligaments can be seen as an incidental finding. The DIP joint should be inspected carefully for recognition of small osteophytes on the distal palmar aspect of the middle phalanx and the dorsoproximal aspect of the navicular bone. Joint space congruity and the shape of the proximal articular surface of the distal phalanx should be assessed carefully. A smoothly outlined depression sometimes is seen in the middle of the proximal articular surface of the distal phalanx in clinically normal horses.
The flexed oblique radiographic images—dorsal 60° lateral-palmaromedial oblique and dorsal 60° medial-palmarolateral oblique—enhance detection of periarticular new bone (Figure 33-2) modeling of the distal aspect of the middle phalanx and entheseous new bone at the origin of the collateral ligaments of the DIP joint. Care is needed to differentiate between periarticular osteophytes and entheseous new bone at the insertion of the digital extensor tendon. Evaluation of the integrity and thickness of the subchondral bone plate of the middle and distal phalanges is important. Discontinuity of the subchondral bone plate may be the first radiological sign of the development of an osseous cystlike lesion. Increased thickness of the subchondral bone plate may occur with OA.
Diagnostic Arthroscopy
The dorsal and palmar pouches of the DIP joint may be inspected arthroscopically; however, the view of joint surfaces is limited, and complete assessment of the integrity of the articular cartilage is not possible (see Figure 23-5). Access may be enhanced after joint trauma with resultant instability of the joint. Affected horses usually develop long-term lameness problems. Lavage of the joint may be beneficial therapeutically in some horses with chronic DIP joint pain without joint instability. A limited view of the DSIL can be seen from the navicular bursa.
Magnetic Resonance Imaging
Sagittal, frontal, and transverse magnetic resonance (MR) images of the DIP joint permit excellent evaluation of the articular cartilage and subchondral bone of the joint and the dorsal and palmar pouches of the DIP joint capsule (Figure 33-3). The DSIL, DDFT, collateral sesamoidean ligaments, and the navicular bone and bursa also may be assessed. Magnetic resonance imaging (MRI) is the imaging modality of choice for horses with chronic DIP joint pain that does not respond adequately to medical treatment.
Differential Diagnosis of Primary Distal Interphalangeal Joint Pain
Synovitis
The most common cause of DIP joint pain is synovitis, which may occur unilaterally or bilaterally. Lameness is mild to moderate in degree, and palpable distention of the DIP joint capsule usually is present. Intraarticular analgesia generally resolves the lameness. Treatment should be directed to identification of any predisposing causes. Corrective trimming to restore correct foot balance and appropriate shoeing are essential for successful management. Horses with a collapsed heel usually benefit substantially from properly fitted egg bar shoes (see Figure 30-18). The timing of trimming and shoeing can be crucial: if the feet are allowed to get too long, soreness may return.
Osteoarthritis
Osteoarthritis without Radiological Abnormalities
Scintigraphy may be useful in the diagnosis of early subchondral lesions associated with OA. The definitive diagnosis of OA without radiological abnormalities is possible premortem only by MRI (Figure 33-4). Horses may have signs similar to those of primary synovitis, but the degree of lameness may be more severe, especially if the horse is exerted maximally, and the response to intraarticular medication tends to be shorter and less complete. MRI may show a reduced signal intensity within the articular cartilage of the DIP joint, in addition to irregularity in the cartilage surface, with or without concurrent abnormalities in the subchondral bone. The prognosis for sustained future soundness is guarded.
Osteoarthritis with Radiological Abnormalities
Correlation is lacking between modeling in the region of the extensor process of the distal phalanx and lameness associated with the DIP joint. Enthesophytes at the site of insertion of the common digital extensor tendon should be differentiated from osteophytes. Enthesophytes may not be associated with current lameness, but may reflect chronic instability of the joint. The presence of periarticular osteophytes on the distodorsal and palmar aspects of the middle phalanx and the proximal articular surface of the navicular bone is more likely to be associated with lameness (Figures 33-5 and 33-6). Radiological evidence of OA of the DIP joint can be seen with other causes of lameness, such as navicular disease. Horses with primary OA of the DIP joint may respond better to serial treatments with PSGAG than treatment with hyaluronan and corticosteroids.15,16 However, if concurrent severe synovitis is present, primary treatment with triamcinolone acetonide and hyaluronan, followed by intraarticular PSGAG, may yield the best results. In my experience, better results are achieved in horses that are sound after intraarticular analgesia compared with horses that show partial improvement in lameness. Prognosis usually is inversely related to the severity of the radiological abnormalities.7

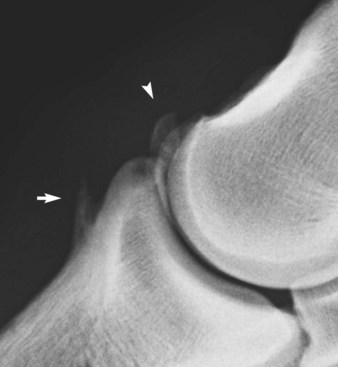
Fig. 33-6 A, Dorsolateral-palmaromedial oblique radiographic image of a flexed distal interphalangeal joint of an 8-year-old show jumper with bilateral forelimb lameness improved by intraarticular analgesia of the distal interphalangeal joints. There is modeling of the proximal articular margin of the distal phalanx (arrow), radiological evidence of osteoarthritis (compare with Figure 33-2). There is also enthesophyte formation on the dorsomedial aspect of the middle phalanx at the origin of the medial collateral ligament of the distal interphalangeal joint. No radiological abnormalities were seen in lateromedial or dorsopalmar radiographic images. B, Lateromedial radiographic image of the left front foot of a riding horse with lameness improved by intraarticular analgesia of the distal interphalangeal joint. An articular osteophyte is seen on the dorsoproximal aspect of the navicular bone (arrow), and there is a fragment on the dorsal aspect of the distal interphalangeal joint (arrowhead).
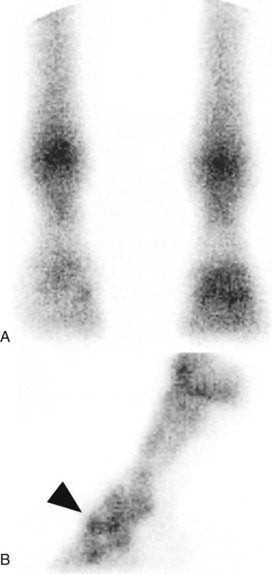
Joint Capsule Trauma
Traumatic damage to the joint capsule, with or without subchondral bone trauma, usually results in sudden-onset, severe lameness that persists despite rest. Lameness may be accentuated markedly when the horse turns. In the acute stage, no abnormalities are detected on radiographic examination. However, periarticular new bone may develop after several weeks (Figure 33-7). Nuclear scintigraphic examination may show generalized increased radiopharmaceutical uptake in the region of the DIP joint (Figure 33-8). Arthroscopic evaluation in these horses has been unrewarding. The response to intraarticular medication has been poor, and the prognosis for return to athletic function despite prolonged rest is guarded.

Fig. 33-7 Lateromedial radiographic image of the left front foot of a 3-year-old Thoroughbred filly with severe lameness that improved substantially after intraarticular analgesia of the distal interphalangeal joint. Entheseous new bone is seen on the dorsal aspect of the middle phalanx, in addition to the small fragment at the extensor process of the distal phalanx. Nuclear scintigraphic examination had revealed a similar pattern of uptake of the radiopharmaceutical to that seen in Figure 33-8.
Subchondral Bone Trauma
Subchondral bone trauma may be focal or more generalized and usually is associated with unilateral lameness, which responds poorly to intraarticular medication and short periods of rest. No detectable radiological abnormalities may be apparent in the acute stage, although Ross14 described subtle proliferative changes on the distal aspect of the middle phalanx and the proximal aspect of the distal phalanx and a variable degree of subchondral lucency in the proximal aspect of the distal phalanx. Nuclear scintigraphy may be helpful.14 Several horses have been examined with acute-onset severe and persistent lameness, which was partially improved by intraarticular analgesia of the DIP joint. MRI has revealed a focal lesion in the proximal subchondral bone plate of the distal phalanx, usually axial and toward the palmar or plantar aspect (see Figure 33-3). Response to conservative management, with or without intraarticular medication or systemic treatment with tiludronate, has been poor.
Fracture of Extensor Process of Distal Phalanx
Fractures of the extensor process of the distal phalanx are discussed in the next section.