Chapter 70The Deep Digital Flexor Tendon
Deep Digital Flexor Tendonitis Associated With Recurrent Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon
Injuries of the DDFT in the carpal or metacarpal region, proximal to the DFTS, are rare except in association with chronic desmitis of the ALDDFT (see Chapter 71). Recurrent desmitis may be accompanied by pathological lesions of the DDFT.2 Because of the close proximity of the DDFT and its accessory ligament, it is difficult to assess each structure accurately by palpation, especially with chronic enlargement of the ALDDFT, which may wrap around the borders of the DDFT. Ultrasonographic examination may reveal slight enlargement of the DDFT. The dorsal border may be less well defined, and diffuse hypoechogenic regions may occur within the DDFT, extending a variable distance proximodistally. These injuries usually result in recurrent lameness.
Primary deep digital flexor tendonitis in the proximal metacarpal region is rare. A single case was recorded by Genovese and Rantanen4 in an 8-year-old Quarter Horse used for English pleasure riding. Lesions have been identified using magnetic resonance imaging in a small number of horses.5,6 Occasionally, traumatic injuries of the DDFT have been seen within the carpal sheath (see Chapter 75).
Deep Digital Flexor Tendonitis in the Carpal Sheath Secondary to Solitary Osteochondroma or a Distal Radial Physeal Exostosis
Deep Digital Flexor Tendonitis within the Digital Flexor Tendon Sheath in the Fetlock Region
Some enlargement of the DFTS is common in hindlimbs, often unassociated with lameness, but occurs less frequently in forelimbs. Sudden-onset lameness associated with distention of a DFTS in a forelimb or a hindlimb may be caused by a variety of different lesions, but deep digital flexor tendonitis always should be considered5,6 (see Chapter 74). It is rare to identify lesions of the DDFT within a DFTS that is not distended. Some horses develop deep digital flexor tendonitis after long-term chronic enlargement of the DFTS.
Lameness varies from mild to moderately severe. Distention and thickening of the DFTS may make accurate palpation of the DDFT difficult. In some horses pain can be elicited by palpation of the margins of the tendon or by firm pressure applied to its palmar (plantar) aspect. The tendon should be assessed throughout its length, proximal and distal to the fetlock. In the acute stage there may be localized heat. Passive flexion of the lower limb may induce pain. If forelimb lameness is only mild in straight lines, it may be exaggerated on the lunge on a soft surface, especially in medium and extended trot. Distal limb flexion often accentuates the lameness. Occasionally in hindlimbs lesions of the DDFT within the DFTS have been the cause of sporadic lameness. The intermittent nature of the lameness makes definitive identification of the cause a diagnostic challenge. Such a history seen in conjunction with distention of the DFTS should prompt ultrasonographic examination (Figure 70-1).16
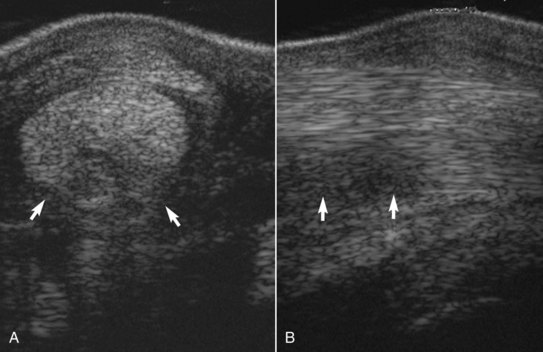
The normal DDFT changes in its shape and cross-sectional area from proximally to distally, but it is usually bilaterally symmetrical. A normal DDFT is uniform in its echogenicity, and its margins are clearly defined. At the site at which the ALDDFT merges with the DDFT there may be a relatively hypoechogenic region, especially in the hindlimbs. This is a normal variant. Hypoechoic artifacts are induced readily in the distal fetlock and pastern regions if the ultrasound transducer is not perpendicular to the tendon, and in these regions evaluating the SDFT and DDFT simultaneously is difficult. Echogenic synovial plicae (mesotendon) extend medially and laterally from the DDFT to the DFTS wall in the proximal recess of the DFTS (Figure 70-2, A). These are seen much more obviously when the tendon sheath is distended and should not be mistaken for marginal tears or adhesions. With chronic tenosynovitis, these plicae may become thickened. Distal to the fetlock is an echogenic palmar (plantar) synovial fold that should not be confused with an adhesion (see Figure 70-2, B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree