Chapter 38The Carpus
Anatomy
The carpus has a dense joint capsule dorsally that blends with the overlying fascia and retinaculum. Synovium in young horses is often thickened or folded dorsally in the middle carpal joint and can interfere with visibility during arthroscopic surgery. This fold appears to smooth as horses age or as osteoarthritis develops. The antebrachial fascia blends with the retinaculum that functions to restrain extensor tendons. Retinaculum thickens and forms the medial and palmar borders of the carpal canal. The palmar retinaculum is sometimes severed in horses with carpal tenosynovitis and tendonitis (see Chapter 75). Anatomical considerations and flexor and extensor tendon injuries are discussed elsewhere (see Chapters 69 and 77). The sheathed extensor carpi radialis and common digital extensor tendons, located dorsally and dorsolaterally, respectively, limit carpal palpation and restrict access. Cul-de-sacs of distended antebrachiocarpal and middle carpal joint capsules can be palpated medial to the extensor carpi radialis tendon or between the extensor carpi radialis and common digital extensor tendons in a standing horse. Arthrocentesis and arthroscopic examination require careful placement of needles and instruments in these portals to avoid injury to tendons and sheaths. These portals can be easily felt as distinct depressions when the carpus is flexed. The sheathed lateral digital extensor tendon, located on the lateral aspect, should be avoided during arthrocentesis of the palmarolateral pouches. The sheathed extensor carpi obliquus tendon is small and passes obliquely over the antebrachiocarpal joint from lateral to medial to attach to the McII. This tendon can readily be seen medially during arthroscopic examination of the antebrachiocarpal joint. Extensor tenosynovitis must be differentiated from middle carpal and antebrachiocarpal joint effusion and hygroma. The antebrachiocarpal and middle carpal joints each have a palmarolateral and a palmaromedial outpouching through which arthrocentesis and arthroscopic evaluation can be performed. Unless greatly distended, the palmarolateral outpouchings are larger than the corresponding palmaromedial outpouchings. The palmarolateral outpouching of the antebrachiocarpal joint is in close proximity to the carpal sheath, and inadvertent penetration of the carpal sheath can occur during arthrocentesis or arthroscopic examination even when the palmarolateral outpouching is distended.
Knowledge of the communications and boundaries of the carpal joints is important in understanding the extent of disease processes and the results of diagnostic analgesia (see Chapter 10). The antebrachiocarpal joint is considered solitary, although in a single specimen in a cadaver study the joint communicated with the middle carpal and carpometacarpal joints.10 In some horses a communication appears between the antebrachiocarpal joint and the carpal sheath. The middle carpal and carpometacarpal joints always communicate (see Figure 10-8Figure 10-9Figure 10-10). Communication between the middle carpal and carpometacarpal joints and the carpal sheath is rare. The carpometacarpal joint has distinct distopalmar outpouchings located axial to the McII and the McIV that have secondary pouches interdigitating within the proximal aspect of the suspensory ligament (SL). These outpouchings explain inadvertent analgesia of the carpometacarpal and middle carpal joint while performing high palmar analgesia and possibly why lameness abates during middle carpal analgesia in horses with avulsion fractures of the proximopalmar aspect of the McIII or proximal suspensory desmitis.11
Conformation
Racehorses, especially Thoroughbreds (TBs), with offset-knee (bench-knee) and back-at-the-knee (calf-knee) conformation are predisposed to develop carpal lameness. Mild in-at-the-knee (carpus valgus) deformity is common and of little concern, but if the deformity is severe, it can predispose to carpal lameness similar to that in horses with out-at-the-knee (carpus varus) conformation (see Chapter 4).
Clinical Characteristics and Diagnosis of Carpal Lameness
Degree of lameness varies with the type and severity of carpal injury. Horses with early or mild chronic OA have mild lameness, whereas those with acute osteochondral fragments, slab fractures, or other more serious injuries have more severe lameness. Horses with infectious arthritis and comminuted carpal or other severe fractures may not bear weight at the walk. Dynamic angular deformity, carpus valgus or varus, may be seen in horses attempting to bear weight with comminuted fractures and loss of joint integrity. Lameness may be intermittent in horses with early and incomplete osteochondral fragments and may be apparent only after training or racing. Racehorses with bilaterally symmetrical lameness may not show overt lameness but have a wide, short gait bilaterally. Advancing and placing the affected limb wide while walking or trotting (pacing) is typical of carpal lameness (see Chapter 7). ![]() Horses with severe OA and natural carpal ankylosis or surgical arthrodesis swing (abduct) the limb because the carpus cannot flex. Advancement and placement of the limb in a lateral (abducted) position is not pathognomonic for carpal lameness, and horses with proximal palmar metacarpal pain or those with pain originating laterally in the digit may manifest similar signs. However, carpal tenosynovitis does not result in this typical carpal gait. Horses with carpal lameness have a shortened cranial phase of the stride. Lameness can be worse with the limb on the inside or outside of the circle depending on whether the location of pain is medial or lateral, but, in general, lameness in most horses with carpal lameness is worse with the limb on the outside of the circle.
Horses with severe OA and natural carpal ankylosis or surgical arthrodesis swing (abduct) the limb because the carpus cannot flex. Advancement and placement of the limb in a lateral (abducted) position is not pathognomonic for carpal lameness, and horses with proximal palmar metacarpal pain or those with pain originating laterally in the digit may manifest similar signs. However, carpal tenosynovitis does not result in this typical carpal gait. Horses with carpal lameness have a shortened cranial phase of the stride. Lameness can be worse with the limb on the inside or outside of the circle depending on whether the location of pain is medial or lateral, but, in general, lameness in most horses with carpal lameness is worse with the limb on the outside of the circle.
Diagnostic Analgesia
In many horses, clinical signs and characteristic gait may allow a tentative diagnosis of carpal lameness, but in most horses diagnostic analgesia should be performed. Analgesia of the middle carpal and antebrachiocarpal joints should be performed independently and sequentially. Dorsal intraarticular techniques are most common, but in horses with scurf from previous counterirritant application or dorsal wounds, the palmarolateral pouches are used. Careful selective perineural and intraarticular analgesic techniques should be performed to differentiate between proximal palmar metacarpal pain and authentic carpal pain (see Chapter 10). Intraarticular analgesic techniques are highly specific, but false-negative results may occur.12 False-positive results may also result because of abolition of carpal sheath pain or proximal palmar metacarpal region pain. Subchondral bone pain may not always be eliminated by intrasynovial deposition of local anesthetic solution, because nerve fibers may be located in bone or travel to the site by another extrasynovial route. The median and ulnar nerve block, although lacking specificity, is useful in horses with suspected carpal region pain that is not abolished by intraarticular techniques.
Imaging
Radiography
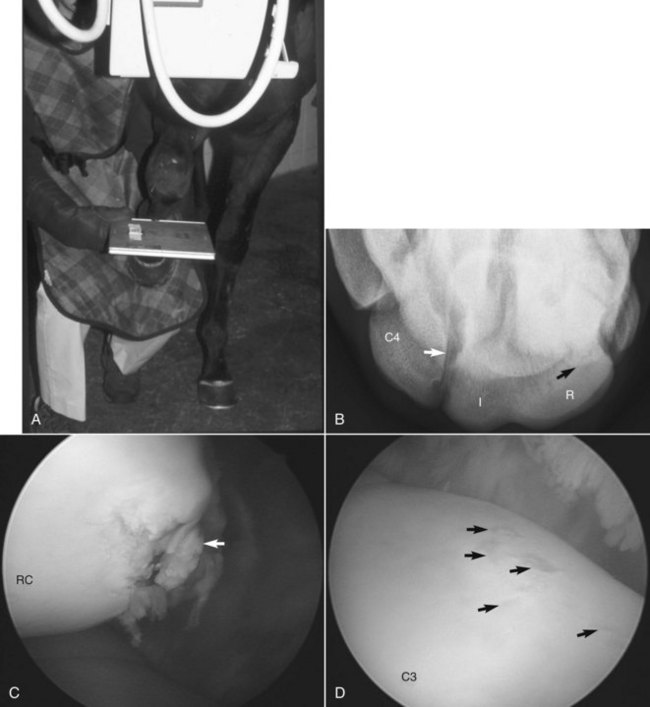
A minimum of six well-exposed and positioned radiographic images are necessary for comprehensive examination of the carpus, including the dorsopalmar (DPa), lateromedial (LM), dorsal 45° lateral-palmaromedial oblique (DL-PaMO), dorsal 45° medial-palmarolateral oblique (DM-PaLO), and flexed LM images and the dorsoproximal-dorsodistal (tangential, skyline) image of the distal row of carpal bones. The skyline image is most important for assessing subtle radiological changes of the third carpal bone, but well-positioned images are often difficult to obtain. Evaluation of the radial fossa requires flexion of the limb in the sagittal plane with the metacarpal region beneath the antebrachium (Figure 38-1). Lateral positioning of the distal part of the limb results in overlap of the radial fossa of the third carpal bone and the radial carpal bone. The skyline image underestimates the amount of increased radiopacity of the third carpal bone and magnifies normal anatomy and lesions approximately twofold.13 The skyline image is not a true proximal-to-distal view of the second, third, and fourth carpal bones, and therefore lesions located palmar to the dorsal edge of the radial carpal bone cannot be seen. The skyline image cannot be used to evaluate fracture lines located more than 8 to 10 mm from the dorsal edge of the third carpal bone or to differentiate large osteochondral fragments from frontal slab fractures of the third carpal bone. Additional images, such as the tangential image of the proximal row of carpal bones (used to identify osteochondral fragments and unusually located frontal or sagittal slab fractures), flexed oblique images (e.g., DL-PaMO view with the limb held in flexion for evaluation of the articular surfaces of the third and radial carpal bones), and weight-bearing, oblique images of different obliquity (e.g., off DPa views, used to identify sagittal slab fractures of the third carpal bone) are sometimes useful. Considerable confusion arises in description of oblique images, with the use of terms lateral and medial oblique instead of naming the images according to the direction of the x-ray beam. To most clinicians, the lateral oblique is equivalent to a DL-PaMO image, but to others it is just the opposite. Follow-up radiographic examination is recommended in 10 to 14 days if fracture is suspected but initial radiological findings are negative or equivocal.
Normal radiological anatomy of the carpus is difficult because carpal bones overlap considerably, bones shift during flexion, and normal radiolucent defects and aberrant carpal bones can be difficult to interpret. In the skyline image of the distal row, the normal articulation between the third and fourth carpal bones can be superimposed on the lateral aspect of the third carpal bone and confused with a sagittal fracture (see Figure 38-1, B). On a DM-PaLO image the normal articulation between the second and third carpal bones should not be confused with a sagittal slab fracture, but this image is essential to diagnose sagittal fracture of the third carpal bone correctly, which runs parallel to this articulation. Radiolucent defects or osseous cystlike lesions are often seen in the ulnar carpal bone and are considered incidental findings, but when they appear in other bones, they can cause lameness regardless of whether communication with a joint exists. In LM and oblique images, the first and fifth carpal bones can be confused with osteochondral fragments. Radiolucent defects in the McII and the McIV often occur in the presence of the first (see Figure 37-7) and fifth (Figure 38-2) carpal bones but are normal. In a flexed LM image the radial carpal bone moves distally relative to the intermediate carpal bone. This normal finding is quite useful in determining the exact positioning of osteochondral fragments or other lesions on the proximal or distal surfaces of the radial and intermediate carpal bones. The flexed LM image is also highly useful for evaluation of the distal dorsal articular surface and subchondral bone of the radial carpal bone. Xeroradiography has largely been discontinued, but computed radiography and digital radiography are available at most institutions and many private practices and yield images superior to those obtained by conventional radiography, but positioning and exposure must still be optimized. Subtle radiological changes can be readily seen in most digital radiographic images, as can fragments, radiolucent defects, and other changes not previously visible on conventional images (see Figure 38-1). Care must be taken not to confuse normal articulations for fractures.
Scintigraphy
Scintigraphy is especially useful to diagnose early stress-related subchondral bone injury and differentiate carpal lesions from those of the proximal metacarpal region (see Figure 19-19). A common finding in young racehorses is carpal lameness localized by clinical signs and diagnostic analgesia with negative or equivocal radiological abnormalities. Focal areas of increased radiopharmaceutical uptake (IRU) are often found unilaterally or bilaterally, most commonly in the third carpal bone (see Figure 19-16). Scintigraphy can be used to verify or refute the importance of sclerosis in the third carpal bone. Scintigraphy is useful in diagnosing unusual fractures of the palmar aspect of the third carpal bone, corner fractures or table surface collapse of the third carpal bone or other carpal bones, and lesions that are not apparent or are located in obscure areas not depicted radiologically. Focal areas of IRU occur with many carpal injuries, and although sensitivity is high, the specificity of scintigraphic images is low and differentiation of specific types of injuries is difficult. Scintigraphy is most useful in localizing the site of injury, based on which additional radiographic images are obtained, or rest is recommended, followed by repeated radiographic examination.
Diagnostic Arthroscopy
In horses with scintigraphic evidence of IRU and those with OA but without radiological confirmation of osteochondral fragmentation, arthroscopic examination usually reveals cartilage damage, the extent of which can be graded. Prognosis is inversely related to degree of cartilage damage (see Figures 23-7 and 38-1). Occult osteochondral fragments, most commonly involving the third and radial carpal bones, and intercarpal ligament tearing are found frequently in these horses (see Figure 23-4).
Specific Conditions of the Carpus
Osteoarthritis
OA is the most common carpal problem, but clear differentiation of OA from osteochondral fragmentation is difficult, because both problems are intertwined. Horses with osteochondral fragments often develop OA, and horses with early OA, and some with chronic OA, develop osteochondral fragments. Pathogenesis of OA and osteochondral fragmentation appears similar if not identical in some horses, but OA of the equine carpus has two forms. The most common form is seen in racehorses or ex-racehorses that initially develop stress-related subchondral bone injury of the middle carpal and antebrachiocarpal joints that leads to, or accompanies, overlying cartilage damage and osteochondral fragmentation (see Figure 38-1). A second form of OA develops in nonracehorses and is less common. Horses are usually middle aged or older, but occasionally it occurs in younger horses. Typical clinical and radiological evidence of OA exists, but osteochondral fragments are unusual (see Chapters 61 and 84).
OA in racehorses develops from a continuum of stress-related subchondral bone injury and cartilage damage, resulting from impact loading of the carpal bones during training and racing. This process has been studied most thoroughly in the third carpal bone but also occurs in other bones of the middle carpal and antebrachiocarpal joints. Sclerosis of the dorsal aspect of the third carpal bone is an adaptive response in racehorses.23,24 With continued loading the third carpal bone becomes densely sclerotic, and in this stage the response becomes maladaptive or nonadaptive and pathological. Subchondral changes precede those in overlying cartilage, a finding seen experimentally25 and clinically during arthroscopic examination in horses with primary stress-related subchondral bone injury (see Figure 38-1). Sclerotic subchondral bone may induce overlying cartilage damage from abnormal shear forces existing between normal and sclerotic areas.26 In most horses sclerosis leads to areas of resorption and necrosis, which then lead to osteochondral fragmentation and eventually to more advanced OA.6,23,27,28 A possible explanation for bone failure is the lack of support of overlying sclerotic subchondral bone by structurally weakened underlying trabecular bone.29 When carpal bone morphology and metabolism were studied in TB racehorses and unraced controls, racehorses were found to have a net increase in bone formation, leading to stiffer, sclerotic subchondral bone; but in addition, they had increased bone collagen synthesis and remodeling in adjacent trabecular bone that may have been structurally weakened.29 Because many of the changes in early OA in racehorses are mechanically induced, factors such as faulty conformation, intense exercise programs, and differences between racing breeds alter the rate of development and severity of OA. The pathological process continues, and some horses develop OA without osteochondral fragments, whereas others develop osteochondral fragments initially and then OA secondarily.
In many racehorses extensive OA and osteochondral fragmentation lead to retirement, but some are able to compete in other sporting events. Progressive OA can then develop later in life. In middle-aged to old nonracehorses, primary OA develops without stress-related subchondral bone injury, high-impact loading, or development of osteochondral fragmentation. This condition can be seen in Western performance horses, other sports horses, or even in horses and ponies used for pleasure riding. Often severe radiological evidence of OA is seen on initial examination when lameness is subtle (Figure 38-3). In fact, it has been proposed that the threshold of pain in riding horses with severe OA of the antebrachiocarpal joint may be higher than in those with similar conditions of the middle carpal joint, because observation of lameness by owners of these horses was a late event.30 Faulty conformation such as carpus valgus, back at the knee, or bench knee is seen in some horses, but in others neither mechanical nor training-related factors are present. OA in these horses can involve the antebrachiocarpal and middle carpal joints together or separately, but when disease involves the carpometacarpal joint, chronic and severe lameness develops (see Figure 3-2).
Clinical Signs and Diagnosis
Radiological evidence of OA in young horses is often lacking, but increased radiopacity of the third carpal bone may be seen in a skyline image (see discussion of small osteochondral fragmentation). Early radiological changes include mild enthesophyte formation, most common on the radial carpal bone, and subtle marginal osteophytes on the carpal bones and distal radius. In horses with advanced OA, marginal osteophytes and enthesophytes become numerous and large, sometimes causing obvious visible bony swelling (see Figure 38-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree