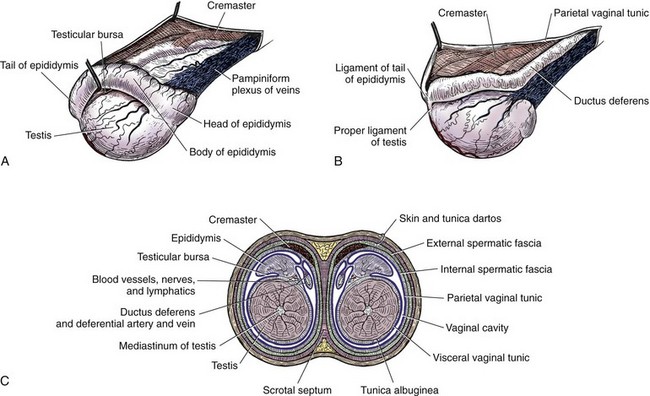
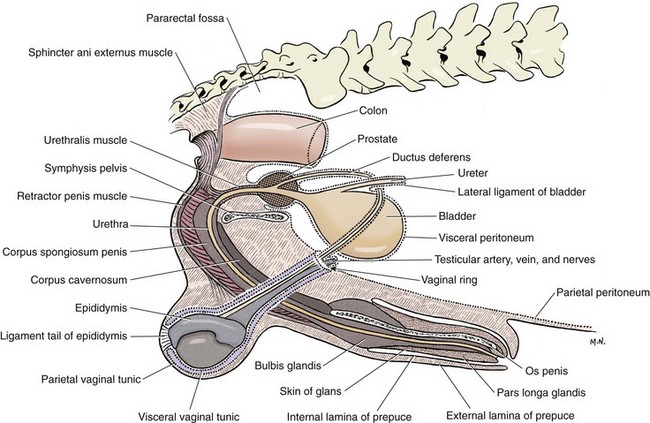
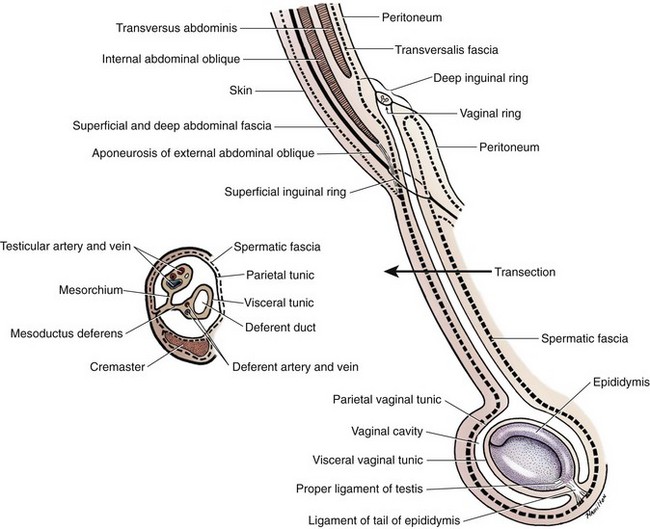
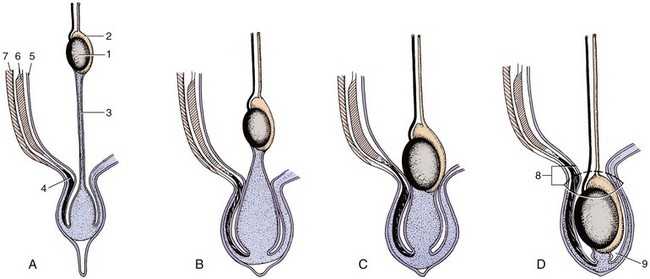
Chapter 111 The testes, or male gonads, are oval in shape and directed dorsocaudally. Each testis with its respective epididymis and distal spermatic cord is located within the scrotum. The left testis is farther caudal than the right testis; this orientation decreases pressure on each testis and allows the testes to glide easily on each other.24 The epididymis is a tightly coiled tube that connects the efferent ducts from the testicle to the vas deferens. It is adherent to the dorsolateral surface of the testis, with its head cranial and tail caudal. The epididymal tail is attached to the testis by the proper ligament of the testis. The ligament of the tail of the epididymis attaches the testis and epididymis to the vaginal tunic and spermatic fascia. The tail of the epididymis continues craniodorsally up into the spermatic cord as the ductus deferens (vas deferens). The ductus deferens enters the abdominal cavity through the inguinal canal, crosses ventral to the ureter at the lateral ligament of the bladder, and penetrates the dorsal prostate to insert into the prostatic urethra (Figures 111-1 and 111-2).24 The spermatic cord contains the ductus deferens and its associated artery and vein, testicular artery, pampiniform plexus, lymphatic vessels, and nerves.24 It is covered by spermatic fascia, which is formed by transversalis, superficial abdominal, and deep abdominal fascia. The cremaster muscle is formed from the internal abdominal oblique and occasionally the transversus abdominus. It inserts on the spermatic fascia and travels along the external surface of the parietal vaginal tunic. The cremaster muscle raises and lowers the testicles, depending on ambient temperature, so that testicular temperature remains slightly below body temperature to enhance spermatogenesis.24 The testicular and ductus deferens arteries supply the testis and epididymis, respectively. The right and left testicular arteries arise from the ventral surface of the aorta at the level of the fourth lumbar vertebra. The ductus deferens artery is a branch of the prostatic artery, which arises from the visceral branch of the internal iliac artery. Within the spermatic cord, the testicular vein forms an extensive network called the pampiniform plexus. This plexus wraps around the artery and provides a mechanism for countercurrent heat exchange to assist testicular thermoregulation. The right testicular vein drains into the caudal vena cava, and the left testicular vein drains into the left renal vein.24 Accompanying the testicular arteries are the nerves of the testicular (internal spermatic) plexus. These nerves are derived from the fourth, fifth, and sixth lumbar ganglia of the sympathetic trunk, which is a division of the autonomic nervous system. Testicular and epididymal lymphatics drain into the lumbar lymph nodes.24 The scrotum is located approximately two thirds of the distance from the anus to the preputial opening in the inguinal region in dogs and ventral to the anus in cats. Whereas the scrotum in dogs is thin, pigmented, and covered with finely scattered hairs, the scrotum in cats is densely haired.24 It is composed of three layers: the skin, tunica dartos, and scrotal fascia. The tunica dartos is a poorly developed layer of smooth muscle mixed with collagenous and elastic fibers that lies deep to the skin. The testes are able to be drawn closer to the body when the tunica dartos contracts.24 The scrotum is divided into two cavities by a median septum composed of fascia and tunica dartos. Each cavity of the scrotum contains a testis, epididymis, and distal portion of the spermatic cord with its associated spermatic fascia, vaginal tunic, and cremaster muscle. Within each scrotal sac is an evaginated pouch of peritoneum called the vaginal process, which is covered by the external and internal spermatic fascia. Deep to the spermatic fascia are the outer, or parietal, and inner, or visceral, tunics. Between these tunics is a cavity that is continuous with the peritoneal cavity at the external inguinal ring. Deep to the visceral vaginal tunic is the dense shiny white capsule of the testis called the tunica albuginea (Figure 111-3).24 The external pudendal artery is the principal blood vessel to the scrotum. The scrotal arteries traverse along the cranioventral surface of the testis superficial to the common vaginal tunic. The scrotal veins correspond to the arterial supplies. The superficial perineal nerve, which is a branch of the pudendal from sacral nerves 1, 2, and 3, supplies the entire scrotum. The tunica dartos is innervated by the postganglionic sympathetic trunk from the superficial perineal nerve, not from the pelvic plexus. Scrotal lymphatics drain to the superficial inguinal lymph node.24 The internal structure of the testis is formed by the convoluted seminiferous tubules, which are composed of three different cell types (spermatogenic cells, Sertoli cells, and Leydig cells) along with connective tissue as its supportive network.100 Within the basal compartment of the seminiferous tubules are the stem cells (spermatogonia). Mitotic division of spermatogonia eventually produces primary spermatocytes with 2n chromosome numbers. These cells undergo meiotic division to form spermatids. Throughout the process of spermatogenesis, spermatids mature and undergo nuclear and cytoplasmic changes and transform from nonmotile cells to motile cells with flagella (tails). They then migrate into the lumen of the seminiferous tubules (spermiation).78 Sertoli cells (sustentacular cells) support the development and maturation of spermatozoa and control the release of spermatozoa into the lumen of the tubules. The basal junction (tight junction) of the seminiferous tubules with adjacent Sertoli cells forms the blood–testis barrier. This barrier controls the environment within the tubules and prevents spermatozoa from entering the interstitium.78 Sertoli cells are stimulated by follicle-stimulating hormone from the anterior pituitary gland. Follicle-stimulating hormone has a negative feedback loop with inhibin. Interstitial cells (Leydig cells) reside within the spaces between the seminiferous tubules and are responsible for producing testosterone.100 Production of testosterone from Leydig cells depends on a negative feedback system with luteinizing hormone and interstitial cell stimulating hormone from the anterior pituitary gland.100 Spermatozoa cells pass from the seminiferous tubules of the testis via the efferent ducts of the rete testis to the epididymis, which stores the spermatozoa until they are released.100 During ejaculation, spermatozoa travel from the epididymis through the ductus deferens (vas deferens) to the prostatic urethra.100 In dogs, the accessory sex gland is the prostate; in cats, the accessory sex glands are the prostate and bulbourethral glands. The prostate secretes thin, milky, alkaline seminal fluid that aids survival of spermatozoa within the acidic female reproductive tract. The bulbourethral glands of male cats secrete a thick mucous substance that also becomes part of the seminal fluid.100 During embryonic development, the testes are intraabdominal but outside the peritoneum. They have a fibrous connection to the scrotum known as the gubernaculum testis. As development progresses, the gubernaculum pulls the testes through the inguinal canal into the scrotum, creating the double-walled tube of peritoneum known as the visceral and parietal vaginal tunics (Figure 111-4).78 Scrotal temperature is less than body temperature to prevent degeneration of seminiferous tubules.44 Several factors are involved in testicular thermoregulation. The scrotal skin is thin, has few hair follicles and little or no subcutaneous fat, and is richly supplied with sweat glands. The external cremaster muscle and tunica dartos muscles allow the testes to be moved away from or closer to the body, depending on external temperature. Warm arterial blood is cooled as it passes next to venous blood within the pampiniform plexus. Seminiferous tubule temperature needs to be 2° to 3° C lower than the body temperature for viable production of spermatozoa.100 Anorchism is the absence of both testicles; monorchism is the absence of one testicle. These are rare conditions in small animals. Richardson and Mullen82 reported a 4% (two in 50) incidence of anorchism in cats, and Millis et al.62 reported a 0.1% incidence (2 in 1345) of monorchism in felines. These conditions are suspected when history rules out previous orchiectomy and physical examination and diagnostics rule out a cryptorchid testicle (see below). Definitive diagnosis is obtained by careful ultrasonographic evaluation, computed tomography, magnetic resonance imaging, or exploratory abdominal surgery. Testosterone concentrations can be used to differentiate a bilateral cryptorchid patient from a bilateral anorchid or castrated patient. After administration of human chorionic gonadotrophin or gonadotropin releasing hormone, testosterone concentrations are measured by radioimmunoassay. Males with a functional testicle will have a functional rapid increase in plasma testosterone levels.21 Cryptorchidism is a condition in which one or both testicles do not descend into the scrotum. The testis originates on the caudal ridge of the kidney in the abdominal cavity of the fetus, passes through the inguinal canal, and descends into the scrotal cavity.84 Testicular descent into the scrotum depends on the growth and action of the gubernaculum. Abnormalities of the gubernaculum, such as absolute or relative failure of outgrowth, aberrant growth, and excessive growth, result in abnormal testicular location. Specific causes of gubernacular abnormalities are incompletely understood.103 Based on studies of Beagles and mixed-breed dogs, the testicles are completely descended by 30 to 40 days after birth.2,55 Although statistical data are lacking, anecdotally testicular descent is prolonged in some canine breeds. Therefore, definitive diagnosis of cryptorchidism may not be made until 6 months after birth.19,81,84 Cryptorchidism is described by location (abdominal, inguinal, prescrotal), side (right, left), and number of testicles affected (unilateral, bilateral).19 Unilateral cryptorchidism is not the same as monorchidism, which is the absence of a testicle. In dogs and cats, unilateral cryptorchidism is more common than bilateral cryptorchidism.19,53,62,82 Several studies report a higher incidence of right cryptorchidism in dogs,14,79,106 but many studies also report an equal distribution of right and left cryptorchidism in dogs and cats.53,62,82,106 The incidence of canine and feline cryptorchidism in the literature is varied. Reported canine incidences are 1.2%, 2.6%, 6.8%, 9.7%, and 12.9%.* Chihuahuas, miniature Schnauzers, Pomeranians, poodles (miniature, toy, and standard), Shetland sheepdogs, Siberian huskies, and Yorkshire terriers have increased prevalences.14,71 In cats, the reported incidences of cryptorchidism are 1.3%, 1.7%, and 3.8%, with an increased prevalence in Persians.62,82,106 Cryptorchidism is strongly suspected as being heritable in dogs and cats.34 A polygenic mode of inheritance is suspected in both species,14,83 and a single sex-linked autosomal recessive gene may be involved in dogs.10,81 Thus, surgical descensus and orchipexy are not recommended. Bilateral cryptorchid patients are sterile because of thermal suppression of spermatogenesis; however, testosterone is still present and allows normal development of secondary sex characteristics, such as feline penile barbs.53,82,84 Unilateral cryptorchid patients are fertile but at a decreased level compared with normal animals. These patients have decreased testosterone concentrations and libidos. They also have reduced ejaculatory function characterized by decreased semen volume, spermatozoa, and sperm motility and higher numbers of abnormal and immature sperm compared with dogs without this condition.53 In addition, a cryptorchid testis can decrease the function of an appropriately descended testicle, preventing compensatory hypertrophy.54 In a study of six unilateral cryptorchid dogs, the cryptorchid testicle was surgically removed; within 24 weeks, the remaining testicle had near normal spermatozoa production.54 Additional secondary complications associated with cryptorchidism include neoplastic transformation or testicular torsion in dogs (see below), continual urine spraying in cats, and concurrent congenital anomalies in dogs and cats. Reported incidences of neoplastic transformation of canine cryptorchid testicles are 9.2%, 10.9%, and 13.6%.33,34,71 It is unknown if feline cryptorchid testicles are prone to developing neoplasia or torsion.62 Increased rates of concurrent hip dysplasia, patellar luxation, defects of the penis and prepuce, and umbilical hernia have been noted in cryptorchid dogs.71 Patellar luxation, a shortened or kinked tail, tetralogy of Fallot, tarsal deformities, microphthalmia, and upper eyelid agenesis have been reported concurrently with felines affected with cryptorchidism.62,82 In a study by Richardson and Mullen,82 all cats with cryptorchidism continued to have odoriferous urine and displayed behavior of intact male cats. Locating ectopic testes can be difficult. In response to fear, stress, or cold, immature testicles can be retracted from the scrotum by cremaster muscle contraction.84 Palpation to locate the undescended testicle was accurate in only 48% of affected cats, and 30% had incorrect initial surgical approaches.82 Inaccurate localization can lead to unnecessary surgical exploration, patient morbidity, and complications. If one testis is descended, it can be pushed dorsally and cranially within the prescrotal region to help determine if it is the right or left testis. Careful palpation of the affected side’s prescrotal area and inguinal canal region is then performed. Prescrotal testicles or those in an inguinal location caudal to the fat pad are usually palpable.82 Small atrophic testicles must be carefully distinguished from inguinal fat or lymph nodes.6 Abdominal testicles are difficult to palpate unless they are enlarged from a pathologic process. A patient with bilateral cryptorchidism cannot be assumed to have both testicles in the same position.82 A thorough physical examination needs to be conducted to rule out clinical signs associated with testicular neoplasia or testicular torsion. A complete blood count (CBC), chemistry panel, and urinalysis are indicated for middle-aged and older patients and in patients suspected to have concurrent neoplasia or torsion. For nonpalpable testicles, diagnostics may include testosterone stimulation tests (to confirm a bilateral cryptorchid patient versus an anorchid), abdominal radiographs and ultrasonography, exploratory abdominal surgery, or abdominal exploratory laparoscopy. Abdominal radiographs may reveal an abnormal soft tissue mass within the abdomen or in the inguinal region. Ultrasonography of the prescrotal region, inguinal region, or abdomen may also be used to find a testicle. Normal testicles are hypoechoic to surrounding fat, with a homogenous medium echotexture. The mediastinum testis is a hyperechogenic central linear structure on the midsagittal plane and a central focal echo on a midtransverse scan plane.35,58 Submission of the testicle for histopathology is recommended after orchiectomy. The incidence of epididymitis and orchitis in dogs is unknown but is considered to be relatively uncommon. Primary causes of orchitis and epididymitis include infectious causes such as bacterial (Brucella canis, Klebsiella spp.), viral (canine distemper), fungal (Rhodotorula glutinis), or rickettsial (Rocky Mountain spotted fever) infection.28,44,51,67 Secondary causes include trauma to the testicle or epididymis, which can result in secondary inflammation or infection, and ascending infection from the prostate or urinary tract.44 Primary orchitis and epididymitis must be carefully differentiated from testicular neoplasia and torsion, which have similar clinical signs. Signs include swelling, pain, lethargy, inappetence, vomiting, pyrexia, and a stiff walking gait. History, clinical findings, blood work indices, testicular ultrasonography, fine-needle aspirate, testicular biopsy, and orchiectomy can be used to help determine the cause.5,67 If epididymitis or orchitis is confirmed in a patient intended for breeding, treatment is aimed at the underlying cause. Otherwise, orchiectomy is performed. Histopathology and culture evaluation of the excised testicle are indicated. Testicular torsion is a rare condition in small animals.65 Torsion of a testicle is more often associated with an intra-abdominal testicle, possibly because it is more mobile; however, inguinal and scrotal testicular torsions have been reported.70 Testicular torsion can be seen concurrently with testicular neoplasia.65,70 Patients affected with testicular torsion can present with vague clinical signs (e.g., anorexia, vomiting, lethargy) or signs typical of an acute abdomen, such as mild to marked abdominal discomfort and shock. Differential diagnosis for acute abdominal pain with no history of trauma may include pathology of the gastrointestinal tract (gastric dilatation and volvulus, intussusception, foreign body obstruction, pancreatitis, incarcerated intestines), urinary tract (acute pyelonephritis, urethral or ureteral obstruction), peritoneum (chemical or septic peritonitis), spleen (torsion), or prostate (abscess).35,56 Testicular torsion is an emergency situation; without prompt diagnosis and surgery, death can ensue. Diagnostics include abdominal radiography, abdominal ultrasonography, and abdominal exploratory surgery. A palpable intra-abdominal mass may also be found during physical examination.6,22,65 On ultrasound evaluation, the testicle may appear enlarged and globoid, and the mediastinum testis may be difficult to recognize. Decreased testicular echogenicity is the most common finding, but hyperechogenicity can also occur. With complete testicular torsion, blood flow within the spermatic cord is absent on color Doppler.35 Decreased blood flow can be seen with an incompletely twisted testicle; increased blood flow may occur after spontaneous detorsion and can appear similar to epididymitis and orchitis.5,35 The prognosis for testicular torsion is good with timely diagnosis and surgical removal of the affected testicle.65,70 The incidence of canine testicular neoplasia is 1.3% to 16.2%.17,80 The mean age of affected dogs is 10.2 years (range, 3 to 19 years).50 Common primary testicular neoplasms include interstitial cell (Leydig) tumors, Sertoli (sustentacular) cell tumors, and seminomas. Overall, these tumors are represented in near equal frequency, but some studies cite interstitial tumors as being more common.17,33,50 More than one tumor may be present at a time; Dow17 cites a 41.5% (39 in 94) occurrence of more than one tumor type at the time of diagnosis.71,79 Feline testicular tumors are rare, and it is unknown if feline cryptorchid testicles are prone to developing neoplasia.105 In dogs, the risk of testicular neoplasia is increased 4.7-fold when inguinal hernias are present.33 The reported incidence of neoplastic transformation of canine cryptorchid testicles is 9.2% to 13.6%.33,34,71 Seminomas and Sertoli cell tumors are twice as common in inguinal cryptorchid testicles than abdominal ones.79,80 Of dogs with Sertoli cell tumors, 16% to 39% may have feminization syndrome. Clinical signs include bilaterally symmetric alopecia, especially of the ventral abdomen and perineum; squamous metaplasia of the prostate, resulting in enlargement and potentially cyst or abscess formation; a pendulous prepuce; penile atrophy; gynecomastia, galactorrhea; and attraction for other male dogs.16,17,63,64,74,80 Hematologic changes include anemia, leukopenia, and thrombocytopenia. Myelotoxicosis can be fatal and is associated with a guarded prognosis, even with castration.16,20,63,93,97 Clinical signs of feminization are generally reversible with orchiectomy unless metastasis is present.59 Sites of metastasis include internal medial iliac, sublumbar, and inguinal lymph nodes; lungs; kidneys; spleen; pancreas; and liver.7,16,17,59 The rate of metastasis is 2.17% to 10%.7,17,50,59,64 The overall rate of metastasis for seminomas is 6.38% to 11%.17,50,66 Sites of metastasis include internal iliac lymph nodes, para-aortic nodes, epididymis, tunica albuginea, and lungs. Prognosis is often curative with surgery and no metastasis.17 Interstitial cell tumors have been associated with increased testosterone production. In a study by Lipowitz et al.,50 concurrent perineal hernias, perianal adenomas, and perianal gland adenocarcinomas were noted in 15%, 37.3%, and 9%, respectively, of dogs with interstitial cell tumors.44 In extremely rare instances, interstitial cell tumors metastasize to sites such as the internal iliac lymph nodes and lung. If metastases are not present, the prognosis is excellent with orchiectomy.17,44,66 Secondary metastatic testicular neoplasia is rare. Two case reports describe metastatic testicular adenocarcinoma with the primary tumor located in the gastrointestinal tract.23,69 If a diagnosis of testicular adenocarcinoma is made, close examination of the gastrointestinal tract is recommended.23 Clinical signs of testicular neoplasms may include discomfort, feminization, and drainage. Dogs may also have signs associated with prostatic disease. On testicular palpation, increased firmness, enlargement, a disparity in testicular size, or a mass (Figure 111-5) may be noted. Many clinical signs are related to paraneoplastic syndrome from hormones produced by the testicular tumor. Sertoli cell and, rarely, seminoma and interstitial cell tumors can produce estrogen.92 Sertoli cell tumors have also been associated with hyperprogesteronemia,60 and interstitial tumors can produce excessive testosterone.25,63 Feminization is most frequently seen with Sertoli cell tumors but has also been reported with interstitial cell tumors and seminomas.63,97 Traditionally, signs of feminization have been attributed to increased estrogen production. In dogs with Sertoli cell tumors, peripheral concentrations of inhibin are increased, and luteinizing hormone, follicle-stimulating hormone, and testosterone are decreased; estradiol-17β, however, remains relatively constant.30 Feminization associated with Sertoli cell tumors is therefore thought to occur because of a significant increase in the ratio of estradiol to testosterone rather than an increase in peripheral estradiol-17β.74 Differential diagnoses include scrotal hernia, orchitis, epididymitis, testicular torsion, spermatocele, varicocele, hydrocele, hematoma, abscess, and sperm granuloma.45 Both testicles must be carefully palpated because the incidence of bilateral involvement is 43% with interstitial cell tumors, 18% with seminomas, and 11% with Sertoli cell tumors.17 Patients should be carefully evaluated for concurrent prostatic disease; thus, digital rectal examination is needed.16,50,79 For valuable breeding animals, ultrasonographic evaluation is useful to localize tumors but not very specific for differentiation. A hydrocele (fluid accumulation around the testicle) may be noted with testicular tumors.58 Ultrasound-guided biopsy may be beneficial in determining the cause.45 Staging diagnostics may include CBC, complete serum chemistry panel, urinalysis, three-view thoracic radiographs, two-view abdominal radiographs, and abdominal ultrasonography. An activated clotting time or buccal mucosa bleeding time should be performed in patients presenting with myelosuppression.16 Serum levels of testosterone, estrogen, and progesterone can also be measured.16 Bilateral orchiectomy is recommended and may be curative. During surgery for an undescended testicle, an attempt should be made to biopsy or remove any enlarged lymph nodes for clinical staging.16 Anemic animals may require transfusion before surgery. Chemotherapy may be attempted for metastatic disease.16 Overall, dogs with testicular neoplasia have an excellent prognosis after orchiectomy if there is no evidence of myelosuppression or metastasis.16,105
Testes and Scrotum
Anatomy
Scrotum
Physiology and Histology
Scrotum
Disorders
Anorchism and Monorchism
Cryptorchidism
Orchitis and Epididymitis
Testicular Torsion
Testicular Neoplasia
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Testes and Scrotum
Only gold members can continue reading. Log In or Register to continue