Chapter 24 Tenoscopy and Bursoscopy
The advantages of arthroscopy as a diagnostic and therapeutic approach to joints1 have prompted the development of applications for other synovial cavities (see Chapter 23). Tenoscopy is the term used to describe endoscopy of synovial tendon sheaths, usually using a rigid arthroscope.2 Bursoscopy is used for endoscopy of bursae.
General Principles of Tenoscopy and Bursoscopy
Surgical Principles and Techniques
The basic principles of arthroscopy are also valid in tendon sheaths and bursae (see Chapter 23). The sheath usually is distended with fluids to facilitate insertion of the cannula. However, this is not necessary for the carpal and tarsal sheaths, which are not approached through distended pouches.9,10 It is generally recommended that the portal be created with a scalpel and the cannula inserted using a blunt, conical obturator to avoid damaging the tendons. A thorough knowledge of the normal endoscopic anatomy of the sheath is paramount for several reasons. First, all the surfaces are covered by synovium and look alike, making identification of the structures difficult. Second, normal anatomical structures such as vinculae and plicae (adhesion-like formations carrying blood vessels to the tendon from the parietal sheath), endotendon (reflection of the synovial membrane, which forms a continuous band attaching the tendon to the sheath along its length), and synovial folds are apparent. These should not be damaged because they participate in the blood supply of tendons within the sheathed portion.12-14
Tenoscopy
Tenoscopy of the Digital Flexor Tendon Sheath
Surgical Technique
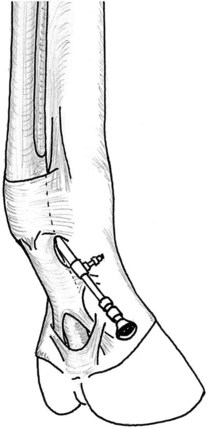
The DFTS is distended with 10 to 20 mL of physiological solution through a needle inserted in the palmar aspect of the midpastern region. Overdistention of the DFTS is avoided because it causes flexion of the digit. A 5-mm longitudinal incision is made through the skin, immediately distal to the PAL, lateral or medial to the DDFT, and 0.5 to 1 cm palmar to the neurovascular bundle, which must be carefully avoided. A stab incision is made into the DFTS, taking care to avoid damaging the DDFT, and the cannula, with a conical obturator inserted in a proximal direction, between the DDFT and dorsal sheath wall (Figure 24-1). The DFTS is lavaged through an 18-gauge needle inserted in the proximal pouch. The obturator is replaced with the endoscope, and examination is carried out from proximal to the level of the portal by rotation and gradual withdrawal. The proximal pouch is examined, followed by the abaxial aspects of the two tendons. Flexion of the fetlock joint allows insertion of the endoscope between the SDFT and DDFT without damage to the manica flexoria. The endoscope is finally rotated around the SDFT on the side of the portal to inspect the mesotendon. Examination of the opposite side is made possible by flexion of the fetlock and rotation of the arthroscope window palmarly.
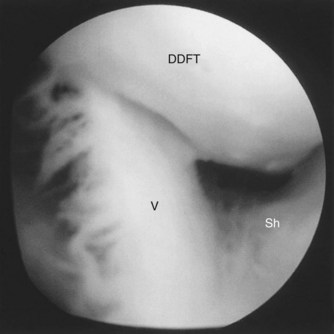
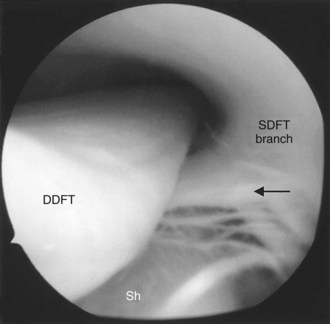
The endoscope is then pushed across the DFTS, between the DDFT and dorsal sheath wall, to avoid exiting the DFTS. The endoscope is then redirected distally. The distal part of the DFTS is examined by gradual withdrawal of the endoscope. The vinculae are visible in the proximal pastern region, between the dorsal surface of the DDFT and dorsal wall (Figure 24-2). Palmarly and farther distally, bifurcation of the SDFT branches forms a manica-like ring around the DDFT (Figure 24-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree