Chapter 23 Arthroscopic Examination
Arthroscopic surgery is arguably the most important advance in management and one of the most important in diagnosis of equine joint disease. Arthroscopic surgery has been a mainstay in managing joint disease since the early 1980s and has mostly replaced arthrotomy. An effective equine surgeon cannot lack extensive arthroscopic surgical experience, and lameness diagnosticians must understand indications and limitations of the technique. Innovators have used the same instruments for bursoscopy and tenoscopy (see Chapter 24). For a complete description of procedures, instrumentation, and principles of arthroscopy, the reader is referred to Diagnostic and Surgical Arthroscopy in the Horse.1
Advantages and Disadvantages of Arthroscopic Surgery Compared with Arthrotomy
Advantages
Disadvantages
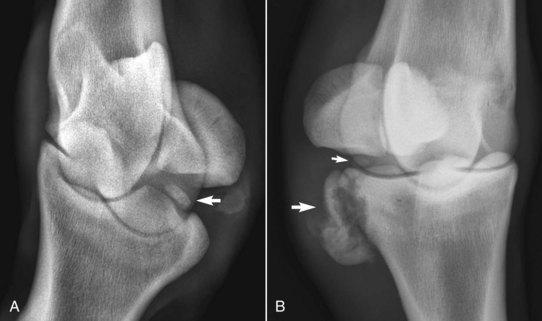
Improper Case Selection
The fragment size that can be easily removed during arthroscopic surgery is limited, and the instrument portal must be enlarged to accommodate such fragments unless ostectomy is performed. The fragment must be located in the joint or at least close to it, a decision that must be made before surgery because arthroscopic surgery is of little benefit if the fragment is not in the joint or close enough to make the approach reasonable and safe. In the metatarsophalangeal joint, large plantar process fragments from the proximal phalanx are often located extraarticularly, and although they may still be best removed using conventional surgical techniques, I have removed large fragments with arthroscopic instrumentation; surgery is facilitated by use of a motorized synovial resector (Figure 23-1). Differentiation should be made preoperatively between fragments free in a joint, which are accessible to surgical removal, and those embedded in the joint capsule and therefore not readily removed. In the stifle joint, fragments in the distal aspect of the femoropatellar joint may appear radiologically as if they are in the femorotibial joint. Rare fragments in the caudal pouches of the medial and lateral femorotibial joints can be difficult to retrieve, especially if the precise location cannot be determined radiologically before surgery. The approaches to the difficult caudal pouches of the medial and lateral femorotibial joints were recently refined.4 Highly mobile fragments in a large joint such as the femoropatellar joint can prove challenging to locate. There is still a limited role for arthrotomy in equine surgery. For example, I still prefer to use a small, medial, middle carpal arthrotomy to repair sagittal slab fractures of the third carpal bone (C3) because I believe I can more accurately place the screw in the medial aspect of the C3, between the C3 and the second carpal bone.5 Others prefer a technique using arthroscopic guidance.1