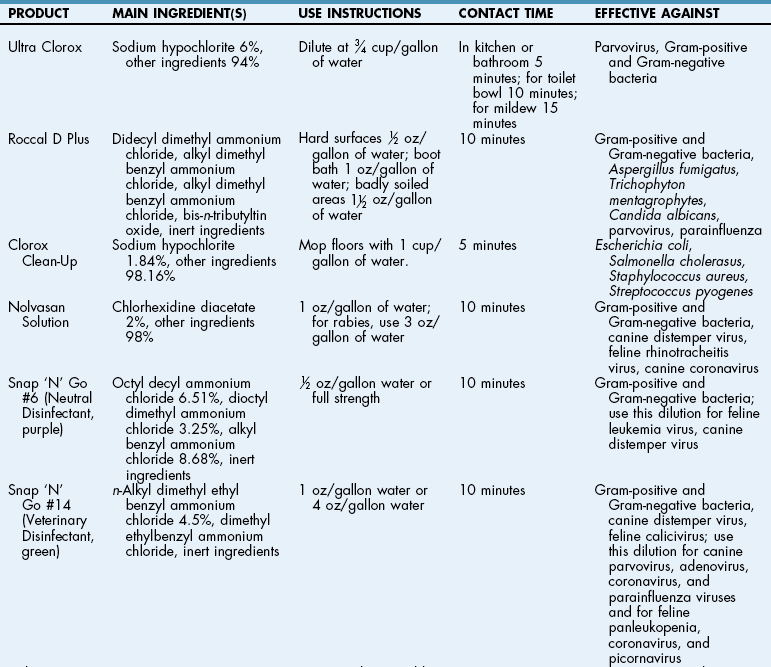
Chapter 3 A variety of physical layouts are suitable for modern operating rooms (ORs) and surgical areas, but the goals of all designs are patient safety and work efficiency. In designing an OR, careful attention must be paid to traffic patterns; the number and configuration of ORs; the space required for storage, administration, and staff; the provisions for sterile processing; and the systems used to manage airborne contaminants (Allo and Tedesco, 2005). The surgical area should be close to the anesthesia and surgical preparation areas, critical care, radiology, and central supply. However, it should be isolated from general traffic flow (e.g., examination rooms, offices, reception area, wards). In large facilities, such as universities and surgical referral centers, the anesthesia and surgical preparation area should be a separate working unit that is isolated from general hospital traffic. Because airborne contaminants can cause or aggravate infection, it is best to create traffic patterns that limit the movement of personnel and materials from outside the surgical suite. Every effort should be made to minimize traffic into and out of rooms. This restricts the movement of airborne contaminants, such as organisms carried and shed by people and objects. Entry into the OR and other clean areas should be limited to essential equipment and personnel (Allo and Tedesco, 2005). Individuals entering a clean area from a contaminated area must don proper surgical attire (see Chapter 6); the ideal location for moving from a contaminated area to a clean one (or vice versa) is through a locker room. Surgical personnel who leave a clean area and enter a contaminated area must cover their clothing before they leave and discard these items when they return to the clean area. Doors between clean and contaminated areas should be kept closed at all times. Food and drink are permitted only in contaminated areas. Movement of clean and sterile supplies and equipment should be separated as much as possible from movement of contaminated supplies and equipment by space, time, and traffic patterns. Soiled linen and trash should be kept in a contaminated area, and patients should be clipped and vacuumed in a contaminated area before transport to a clean area (e.g., the operating room). Guidelines useful for limiting movement from the outside into the operating suite are included in Box 3-1. Most particles and bacteria found in operating room air are shed from skin and hair by personnel in an OR. Although no one has established a direct relationship between the number of people in an OR and the development of postoperative infection, some studies suggest that as the number of personnel in the OR increases, so does the incidence of surgical site infection (Pryor and Messner, 1998). Whether this has to do with the people themselves or the greater amount of traffic into and around the room is not clear. Opening the doors to the OR decreases the effectiveness of the ventilation system in effectively clearing potential contaminants from the OR outward. The goal is to create realistic traffic and commerce of patients, personnel, and supplies, with careful attention to “clean” and “mixed” work areas (Allo and Tedesco, 2005). Preparation counters and surfaces should be impervious and easily cleaned and disinfected (Table 3-1). Stainless steel preparation tables with built-in sinks are ideal. Gas scavenger systems should be present at each anesthesia preparation table. General lighting is supplied by main overhead fluorescent lights, which are supplemented by a spotlight directed at each preparation table. A sink designated for cleaning anesthetic hoses, endotracheal tubes, and rebreathing bags, plus a plastic rack for draining and drying rebreathing bags and hoses, should be available. An erasable anesthesia-surgery scheduling board, easily visible to anesthesia and surgical personnel, should list the day’s procedures. The sterile instrument room is a clean area that houses all sterilized and packaged instruments and supplies. It commonly is near the nurses’ work station. Surgery personnel assemble items necessary for a particular case from supplies in this room. Items should be logically arranged on shelves (e.g., alphabetical order) and routinely checked for “outdates” (i.e., time-related expiration; see p. 6) and package integrity (i.e., event-related expiration; see p. 6). Sterile supplies should be transported into ORs in closed sterile containers. Inadequate sterilization of surgical instruments has been implicated in outbreaks of surgical site infection (see Chapter 2). For this reason, indicators documenting adequate sterilization must be included in all sterile instrument sets. As a general rule, unless a piece of equipment is mostly or exclusively used in a given OR, it should be stored elsewhere. Large pieces of equipment, such as anesthesia machines, lasers, monitoring equipment, operating microscopes, and portable surgery lights, can be stored in an equipment room. Equipment should be kept free of dust and cleaned routinely using the protocol described for OR disinfection (see p. 24). The equipment room is a valuable area because it eliminates storage of large, expensive pieces of equipment in hallways, where they could be damaged or create a hazard. Other storage spaces are designated for clean supplies and packaged reusable items and should be in a separate space from the soiled workroom. Carts and gurneys must not be stored where they obstruct corridors (Allo and Tedesco, 2005). Scrub sink areas should be centrally located for the OR suites. Antiseptic soap in an appropriate dispenser (i.e., foot-activated or motion-sensitive), scrub brushes (i.e., sterilized reusable brushes or a disposable polyurethane brush-sponge combination, unless brushless scrub solutions are used [see Chapter 6]), and fingernail cleaners (if used; see Chapter 6) should be kept within easy reach at each scrubbing station. Deep stainless steel sinks equipped with knee-, elbow-, or foot-operated or motion-sensitive water activators are ideal. Electronic sensory activated scrub sinks as shown in Figure 3-1 allow “no touch” activation. With reusable brushes, the dispensing container and clean brushes must be detached and autoclaved regularly. The scrub sink area must be located away from wrapped sterile supplies because of possible contamination by water droplets and spray from the sinks. Scrub sinks should never be used to clean equipment or instruments or to dispose of body fluids. The American Institute of Architects (AIA) guidelines recommend that newly constructed general ORs should have a minimum clear floor area of 400 square feet exclusive of fixed or wall-mounted cabinets and built-in shelves, with a minimum of 20 feet clear dimension between fixed cabinets and built-in shelves (AIA, 2001). These guidelines also state that rooms for cardiovascular, neurologic, orthopedic, and other special procedures that require additional personnel or large equipment should have a minimum clear floor area of 600 square feet and a minimum of 20 feet clear dimension exclusive of fixed or wall-mounted cabinets and built-in shelves. For renovations, the minimum clear floor area for general purpose rooms and orthopedic rooms should be 360 square feet. Cardiovascular, neurologic, and other special purpose rooms should be 400 square feet. Windows should have coved or sloped edges and should be without ledges that can collect dust. They should be well sealed and should not be allowed to be opened. Studies have shown that natural light enhances staff morale (Allo and Tedesco, 2005). The OR should be uncluttered and simple so that no areas trap dust or are difficult to clean. Floors, ceilings, walls, and other surfaces should be smooth, nonporous, and constructed of fireproof materials. Smooth surfaces can be thoroughly cleaned and disinfected (see Table 3-1), which helps to prevent trapping of biological material that could cross-contaminate. Surface materials should be able to withstand frequent washing and cleaning with strong disinfectants. Uniform ceilings are recommended for ORs. Most ceilings are made of plaster; however, moisture-resistant gypsum wallboard systems with special epoxy-based coatings may be less costly. Ceiling-mounted lights or fixtures should be sealed so that dust and contaminants cannot enter through openings, and so that there is no compromise to the ventilation system. In semi-restricted and unrestricted areas (e.g., recovery and holding areas), lay-in ceilings with clips that ensure that dust and other contaminants do not enter the room (Allo and Tedesco, 2005) may be used; however, they are not permitted in ORs. The OR environment should be kept at a constant humidity and temperature because these two factors influence the probability of surgical site infection. Most modern systems maintain adequate temperature, humidity, and pressure relationships; however, disruption of the ductwork can change internal pressure relationships, causing airborne particles to migrate into the system (Allo and Tedesco, 2005). Regularly scheduled surveillance and maintenance of the air handling system is crucial. This involves checking for moisture in walls, ceilings, and other potentially porous materials, ensuring the integrity of air ducts, and checking fan settings and filters. General lighting in the OR is supplied by main overhead fluorescent lights, which are supplemented by one or preferably two halogen spotlights. Surgery lights are designed to emit a soft white light that is of high intensity, low heat, and true color, and that provides shadow reduction without glare. Options include single, double, and triple light-head configurations in wall, ceiling, and stand mounts. Surgical lights generally are ceiling mounted. Track lighting should be avoided because dust and bacteria may become trapped in the tracks. Rotation capabilities are important; most lights rotate 360 degrees at the light-head axis, but some are even more flexible. Many lights can incorporate cameras within them. Fiberoptic headlamps worn by many surgeons are now available in comfortable, lightweight models that virtually eliminate shadowing of the surgical site (Fig. 3-2).
Surgical Facilities, Equipment, and Personnel and Care and Maintenance of the Surgical Environment
Structure and Design of the Surgical Area
Description and Function of Rooms in the Surgical Area
Anesthesia and Surgical Preparation Areas
Sterile Instrument Room
Equipment Room
Scrub Sink Area
Operating Room
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Surgical Facilities, Equipment, and Personnel and Care and Maintenance of the Surgical Environment