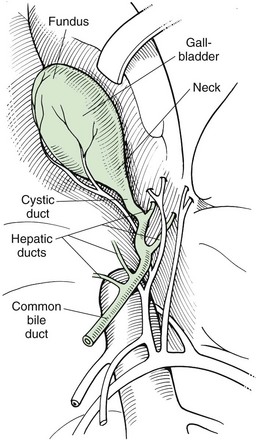
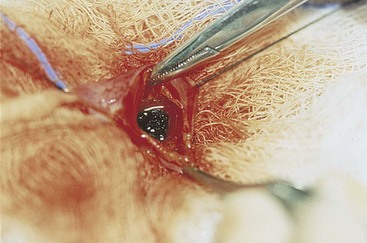
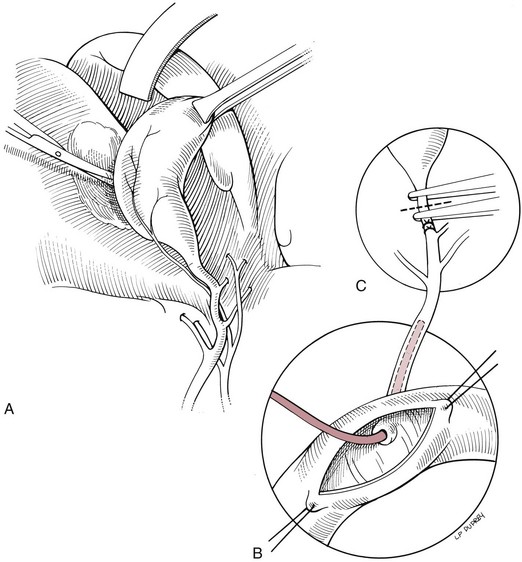
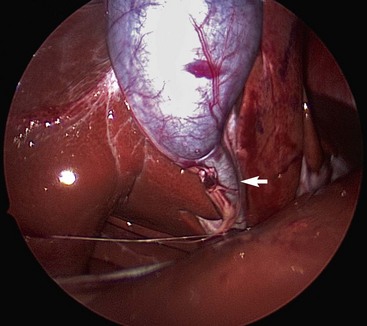
Chapter 22 General Principles and Techniques Animals with EHBO should have electrolyte and fluid abnormalities corrected before surgery. Prolonged EHBO may cause vitamin K malabsorption, resulting in deficiencies of factors VII, IX, and X. Animals with clinical evidence of bleeding or increased mucosal bleeding time should receive vitamin K1 (SC, not IV or IM) for 24 to 48 hours before surgery (Box 22-1) or fresh whole blood (see p. 36). Partial or complete biliary obstruction may allow ascending aerobic and anaerobic infection and subsequent bacteremia; therefore perioperative antibiotic therapy is indicated (see Chapter 9). The finding of hemobilia (upper gastrointestinal bleeding originating in the biliary tree) and hemocholecyst (accumulation of blood or blot clot within the gallbladder) associated with gallbladder neoplasia may not be accompanied by coagulopathy, but coagulation testing should be done (Lippo et al, 2008). Extrahepatic biliary injury may be caused by blunt or penetrating trauma. Common bile duct, gallbladder, cystic duct, or hepatic duct lacerations may cause bile peritonitis or, if the infection is “walled off,” a localized inflammatory process with adherence to surrounding organs. Necrotizing cholecystitis occurs when bacteria damage the gallbladder wall, often resulting in peritoneal spillage of bile (Fig. 22-1). This frequently leads to the development of severe, generalized septic peritonitis. Sometimes bile becomes inspissated before the gallbladder ruptures, and spillage of the relatively thick, gelatinous mass into the cranial abdomen causes a localized peritonitis. Adhesions or fistulous tracts occasionally occur around the gallbladder. See p. 632 for a discussion of the preoperative management of animals with bile peritonitis. Animals with EHBO should be differentiated from those with intrahepatic cholestasis causing partial obstruction, because the former sometimes need surgery but the latter almost never require surgical correction. The indications for exploratory surgery in animals with suspected extrahepatic biliary obstruction are not well defined. An increasing serum bilirubin level over 7 to 10 days in the apparent absence of defined hepatic disease or pancreatitis, combined with supportive radiography or ultrasonographic evidence of obstruction, is generally considered to be an indication for surgery. Dogs with EHBO due to pancreatitis almost never need surgery, although rare patients that do not respond to appropriate medical therapy may require a drainage procedure. Percutaneous ultrasound-guided decompression of the gallbladder may be considered in dogs with acute pancreatitis. Aspiration of bile may be required more than once and does not obviate the need for surgery in all cases. The main complication seen in a small number of dogs was mild, localized bile leakage from the aspiration site (Herman et al, 2005). Readers are referred to medicine texts for an in depth discussion of the treatment of pancreatitis. Nuclear scintigraphy may aid in the diagnosis of complete extrahepatic biliary obstruction (see “Diagnostic Imaging” on p. 620). Anesthetic requirements and concerns for patients with biliary disease are similar to those for patients with hepatic disease (see p. 584). An additional concern in patients with obstructive biliary disease relates to the effect of µ-agonists (e.g., hydromorphone, morphine) on smooth muscle tone. In human beings with biliary obstruction, these drugs increase both sphincter tone and pain. Mixed agonist-antagonists (e.g., butorphanol; see Table 12-3 on p. 141) may be preferable as premedicants and analgesics in these patients. Prophylactic antibiotics are recommended in patients undergoing biliary surgery because of the detrimental effects of bacterial infection on healing. Antibiotic therapy for biliary infection should be based on the results of culture and susceptibility testing of liver parenchyma or bile or both. Organisms most often isolated from biliary infection are Escherichia coli, Klebsiella spp., Enterobacter spp., Proteus spp., and Pseudomonas spp. Antibiotics excreted in active form into the bile, which are commonly used to treat biliary disease, include amoxicillin, cefazolin, and enrofloxacin (Box 22-2). The hepatic and cystic ducts, the bile duct (also known as the common bile duct), and the gallbladder constitute the extrahepatic biliary system (Fig. 22-2). Bile drains from the hepatic ducts into the bile duct and is stored and concentrated in the gallbladder. The gallbladder lies between the quadrate lobe of the liver medially and the right medial lobe laterally. It is a pear-shaped organ that, in medium-sized dogs, holds approximately 15 ml of bile. The rounded end is the fundus. Between the neck of the gallbladder (i.e., the tapering end leading into the cystic duct) and the fundus is the body, or middle portion, of the gallbladder. Radiographic findings in patients with extrahepatic biliary obstruction are generally nonspecific. Hepatomegaly and gallbladder distention may be noted. Mineral opacities in the right cranial abdominal quadrant may be indicative of cholecystic calculi (see p. 627); however, these calculi may also be incidental findings in dogs and cats. Poor serosal detail in the upper right quadrant or diffusely throughout the abdomen may be found in animals with or without gallbladder rupture. In fact, 55% of cases without rupture had decreased abdominal detail locally or diffusely (Crews et al, 2009). Ultrasound evaluation may help distinguish intrahepatic causes from extrahepatic causes of biliary obstruction. Identification of severe pancreatitis or a mass in the region of the pancreas may raise suspicion of EHBO. Ultrasound detection of diffuse peritoneal effusion had a 66.6% sensitivity and an 81.5% specificity for detecting gallbladder rupture, but sensitivity increased to 91.4% if local effusion and echogenic reaction within the gallbladder fossa were also present. Specificity, however, decreased to 44.4% (Crews et al, 2009). With experimental bile duct ligation, the gallbladder becomes distended within 24 hours, and the extrahepatic bile ducts distend within 48 to 72 hours. Intrahepatic ducts take longer to dilate (approximately a week). Remember that dilation from a previous obstructive episode may not resolve; thus it may be difficult to discern whether the present dilation is due to recent or past disease. Hepatobiliary scintigraphy has been used to determine patency of the common bile duct. With ultrasound, it may be difficult to discern whether dilation of the common bile duct in the absence of an obvious obstruction (i.e., calculus, mass) is associated with complete or partial biliary obstruction. A study evaluating the usefulness of serum biochemical values and scintigraphic studies for differentiating between animals that had complete EHBO and those that had partial obstruction found that animals that did not have intestinal radioactivity within 3 to 4 hours should have additional imaging performed (up to 24 hours) to determine whether they had complete EHBO (Head and Daniel, 2005). Those that had partial obstructions had delayed arrival of radioactivity and less radioactivity in the intestine. Re-evaluating these animals at 24 hours may lead to greater specificity. Hepatobiliary scintigraphy appears to be an insensitive test for structural hepatobiliary disease (e.g., cholangiohepatitis). Stenting of the common bile duct may be considered in cases of reversible disease processes (e.g., pancreatitis, inflammatory lesions of the biliary tract of duodenum) to allow stabilization before definitive surgical treatment, and for augmentation of bile duct repair (Mayhew et al, 2006) (see later under “Repair of Common Bile Duct Injuries”). Chronic stenting may be associated with ascending infection. After abdominal exploration, perform a longitudinal duodenotomy of the antimesenteric border of the duodenum over the major duodenal papilla. Flush the biliary tract as necessary, and treat primary disease (cholecystotomy, cholecystectomy, biliary duct repair). Pass a 5 to 10 cm segment of red rubber catheter up the common bile duct via the duodenal papilla, so that approximately one-half of the stent lies within the common bile duct and the other half resides within the duodenal lumen. Suture the stent to the submucosa of the duodenum aborad to the duodenal papilla using absorbable suture. Stents should be passed in the feces in 1 to 11 months or can be removed endoscopically if inflammation or infection is suspected (Mayhew et al, 2006). Cholecystotomy is rarely performed but may be indicated to remove some choleliths (see p. 628), or when the contents of the gallbladder are inspissated and cannot be aspirated into a syringe. In general, cholecystotomy should be avoided in favor of cholecystectomy, which has a lower morbidity/mortality rate. Pack the area surrounding the gallbladder with sterile, moistened laparotomy sponges. Place stay sutures in the gallbladder to facilitate manipulation and reduce spillage. Make an incision in the fundus of the gallbladder (Fig. 22-3). Remove the gallbladder contents and submit for culture. Lavage the gallbladder with warmed, sterile saline. Catheterize the common bile duct via the cystic duct with a 3.5 or 5 French soft catheter, and flush it to ensure patency. Close the incision with a one- or two-layer inverting suture pattern using absorbable suture (3-0 to 5-0). Short-term (temporary) biliary diversion has been described in dogs (Murphy et al, 2007). Definitive surgery was recommended when the catheter was removed to prevent biliary leakage, because maturation of the tract between the gallbladder and body wall did not occur in the aforementioned report within the 25-day period of the study. Cholecystitis that is not responsive to or that relapses after antibiotics, spontaneous rupture, and cholelithiasis that is associated with disease (many cases are asymptomatic) are best treated by cholecystectomy (see p. 628) (O’Neill et al, 2006). Cholecystectomy may also be indicated for primary neoplasia or traumatic rupture of the gallbladder. Expose the gallbladder and use Metzenbaum scissors to incise the visceral peritoneum along the junction of the gallbladder and the liver (Fig. 22-4, A). Apply gentle traction to the gallbladder and use blunt dissection to free it from the liver. Free the cystic duct to its junction with the common bile duct. Be sure to identify the common bile duct, and avoid damaging it during the procedure. If necessary, identify the common bile duct by placing a 3.5 or 5 French soft catheter into the duct via the duodenal papilla. Make a small enterotomy in the proximal duodenum, locate the duodenal papilla, and place a small red rubber tube into the common bile duct (Fig. 22-4, B). Flush the duct to ensure its patency. Clamp and double ligate the cystic duct and cystic artery (Fig. 22-4, C) with nonabsorbable suture (2-0 to 4-0). Sever the duct distal to the ligatures, and remove the gallbladder. Submit a portion of the wall, plus bile, for culture if infection is suspected. Submit the remainder of the gallbladder for histologic analysis if indicated (for cholecystitis or neoplasia). Close the duodenal incision in a simple interrupted pattern with absorbable suture (i.e., 2-0 to 4-0). Laparoscopic cholecystectomy has been performed in dogs with uncomplicated gallbladder mucoceles (Mayhew et al, 2008). Cases should be carefully chosen and should have no biochemical or diagnostic imaging evidence of biliary tract obstruction or rupture. Establish an endoscope port approximately 1 cm caudal to the umbilicus, and explore the abdomen. Triangulate three additional ports; place them under direct visualization. Place one port on the left 3 to 5 cm cranial and 5 to 8 cm lateral to the umbilicus. Place two ports on the right, 3 to 5 cm and 5 to 8 cm lateral to the umbilicus. Retract the gallbladder with a fan retractor to expose the cystic duct (Fig. 22-5). Dissect the cystic duct with curved and right-angle dissecting forceps. Ligate the cystic duct with three extracorporeally tied modified Roeder knots using 0 or 2-0 polydioxanone (PDS) and transect the duct with scissors, leaving two of the ligatures with the portion of the duct remaining in the patient. Alternatively, clip the cystic duct twice with endoscopic clip appliers, transect the cystic duct between clips with scissors, and ligate the portion of the duct remaining in the abdomen with a pre-tied loop ligature. Grasp the duct or suture tail of the portion of the cystic duct to be removed with the gallbladder. Retract the duct and gallbladder, and dissect them from the fossa using a harmonic scalpel. Place the gallbladder in a specimen retrieval bag and partially retract it through one of the operating ports. Aspirate bile until the bag and the gallbladder can be extracted. Evaluate the gallbladder fossa and ligation site for hemorrhage and leakage, respectively, and collect samples of liver for histopathologic examination, culture and susceptibility testing, and metal analysis as needed. Pack the area surrounding the common bile duct with sterile, moistened laparotomy sponges. Place traction sutures in the distended duct. Make a small incision in the duct and remove the obstruction (Fig. 22-6). Flush the duct with copious amounts of warmed, sterile saline, and pass a 3.5 to 5 French soft catheter into the gallbladder and duodenum to ensure patency. Close the incision in a simple continuous or simple interrupted pattern with absorbable suture (4-0 or 5-0). If leakage is a concern, pass a catheter into the duct through an incision in the proximal duodenum (see previously). Treat small leaks by stenting the incision with a 3.5 to 5 French soft catheter (see discussion on repairing common bile duct injuries).
Surgery of the Extrahepatic Biliary System
Preoperative Concerns
Anesthetic Considerations
Antibiotics
Surgical Anatomy
Diagnostic Imaging
Surgical Techniques
Choledochal Tube Stenting
Cholecystotomy
Laparoscopic-Assisted Cholecystostomy
Cholecystectomy
Laparoscopic Cholecystectomy
Choledochotomy
Surgery of the Extrahepatic Biliary System