Taralyn M. McCarrel
Superficial Digital Flexor Tendon Injury
The superficial digital flexor tendon (SDFT) is at great risk for injury in the horse, and it is therefore not surprising that clinically relevant disease involving this structure is common in both racehorse and sport horse populations. Reasons for increased susceptibility to injury and sepsis are numerous and include the tendon’s superficial location, close association with synovial structures susceptible to penetrating injury, and inferior reparative response, plus the fact that the SDFT functions at its biomechanical limit in high-level performance horses. The following chapter will introduce the reader to the diagnosis and management of several different types of injury involving the SDFT and associated structures.
Anatomy and Function
The superficial digital flexor originates from the proximal aspect of the caudal surface of the humerus and inserts on the first and second phalanges. In addition, the accessory ligament of the SDFT (ALSDFT) originates at the level of the musculotendinous junction and has a fanlike insertion on the distal radius in close association with the carpal canal. The hind limb superficial digital flexor originates from the proximal aspect of the caudal surface of the femur and inserts on the phalanges, similar to the arrangement in the forelimb. The hind limb SDFT overlies the calcaneus, where it sends off medial and lateral attachments to this structure. The calcaneal bursa provides a gliding surface between the SDFT and the calcaneal tuber. The forelimb and hind limb SDFT are enveloped by the digital flexor tendon sheath (DFTS) from the distal half of the cannon bone to the pastern (Figure 190-1). The manica flexoria (MF) is an extension of the SDFT that encircles the deep digital flexor tendon (DDFT) within the DFTS.
The superficial digital flexor muscle is composed of very little muscular tissue and thus has minimal role in flexion of the distal limb. Instead, the SDFT’s primary functions are stabilization and energy storage. Along with the suspensory ligament, the SDFT has a major role in supporting the fetlock joint. Furthermore, the muscle fibers are able to adapt to small vibrations that develop during locomotion, yielding a degree of shock absorption. Finally, the SDFT stores elastic energy when it is stretched during the stance phase of locomotion, and release of this energy allows the horse to propel its large mass with great efficiency.
Tendon Repair
Normal tendon is composed primarily of type I collagen arranged linearly in a hierarchical structure. Tenocytes, specialized tendon cells, produce the extracellular matrix, including collagen and noncollagenous molecules that assist in collagen fiber alignment. Blood supply is greatest at the periphery of the tendon, with relatively little vasculature supplying the tendon core.
Tendon repair proceeds through the classic stages of wound healing: inflammation, repair, and remodeling. The inflammatory phase begins at the onset of injury and lasts from a few days to weeks, depending on severity of the injury and antiinflammatory therapy instituted. The release of proteolytic enzymes results in expansion of the lesion, both in length and cross-sectional area, for several days. The repair phase overlaps with the inflammatory phase and is characterized by increased vascularity, cellularity, and production of disorganized small collagens. The remodeling phase is the longest of the tendon healing phases, lasting as long as 18 months. Remodeling overlaps with the repair phase and is characterized by increasing collagen organization and a greater proportion of collagen I. However, the resulting scar tissue is biomechanically inferior. Overall, the scarred area is stronger than normal tendon, but it is less elastic. The transition area between the inelastic repair tissue and the normal tendon is most susceptible to reinjury. A recent report suggested that the most crucial time for therapeutic intervention in the tendon healing process is the period from 12 to 16 weeks after injury.
Tendinopathy
Overstrain injuries of the SDFT are common in racehorses and top-level event horses. Although the clinical signs often manifest acutely, research into the pathophysiology of overstrain injury suggests that chronic degeneration leads to ultimate failure of the tendon. Despite considerable research effort and numerous proposed theories, the definitive cause or causes of SDFT tendinopathy remain elusive. Several risk factors have been identified for Thoroughbred racehorses, including fast work on hard surfaces, increased age at first race start, having a previous SDFT injury, fatigue, and heel elevation.
Diagnosis
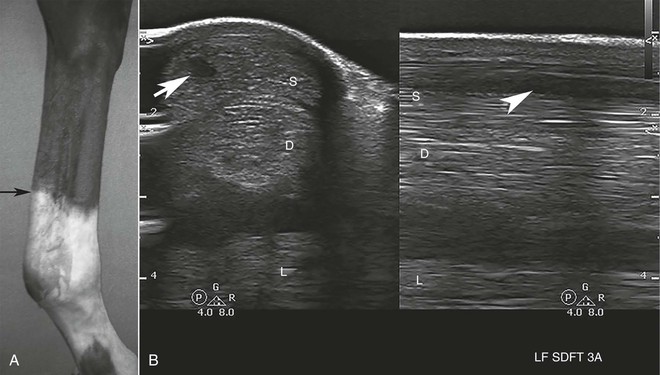
The horse with acute manifestation of classic midmetacarpal SDFT tendinopathy will have variable lameness, depending on lesion severity, and overt lameness may disappear rapidly. The horse should be observed for local swelling characteristic of a “bowed” tendon (Figure 190-2, A). The palmar structures of the metacarpus should be palpated both during weight bearing and with the limb unloaded. Horses with an active injury often resent palpation of the affected region, which may feel soft compared with normal tendon. More chronic lesions may be nonpainful and firm on palpation. A complete lameness examination is warranted because SDFT tendinopathy is often bilateral or may be a secondary overstrain injury arising secondary to lameness of a different cause in another limb. Diagnostic analgesia may be performed if confounding lameness exists, but information from the history, clinical signs, and ultrasound examination is often sufficient for diagnosis of tendinopathy.
Ultrasonography is the primary imaging modality for diagnosis and monitoring of tendon lesions. The palmar or plantar aspect of the distal part of the limb should be clipped, cleaned if necessary, and imaged with a 7.5- to 14-MHz linear probe with a standoff pad. The typical findings of acute tendinopathy include a hypoechoic core lesion with loss of linear fiber pattern, increased cross-sectional area of the tendon, and change in shape of the tendon (Figure 190-2, B). Lesions along the margins of the tendon are also possible. A tendon that is healing appropriately will have an increase in lesion echogenicity, improvement in linear fiber pattern, and decrease in tendon cross-sectional area. The timing of the first ultrasound evaluation and impact of lesion expansion on the ultrasonographic appearance of acute tendon lesions must always be considered. Initially, core lesions may not be evident but will appear several days later. Ultrasound examinations performed within the first week after injury should be repeated in 2 to 4 weeks to allow full assessment of lesion size and severity.
Standardbreds may have SDFT tendinopathy as a part of the “curb” complex of plantar hock soft tissue injury. An atypical form of proximal SDFT tendinopathy was recently described. The lesions were detected in older horses performing lower-level work; horses had an acute onset of lameness, with prolonged lameness thereafter. Horses reacted positively to carpal flexion, and lameness was abated following ulnar nerve block. Diagnosis was confirmed by ultrasonography of the SDFT at the level of the carpal canal, and effusion within the carpal sheath was evident. Prognosis for return to previous use was poor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree