Claudio C. Natalini
Spinal Anesthesia and Analgesia
Neuraxial anesthesia and analgesia, which includes spinal and epidural anesthesia and analgesia, has been used in human and veterinary medicine as an effective technique for treating patients with acute and chronic pain as well as to provide preemptive, intraoperative, and postoperative analgesia. Epidural and spinal analgesia are induced by the injection of analgesic drugs, such as opioids, α2-adrenergic agonists, and dissociative agents, into the epidural or subarachnoid space and their resulting action on the spinal cord after diffusion into the region of the gray matter of the dorsal horn. Recently, corticosteroids also have been used in humans for their antiinflammatory action. Neuraxial blockade with local anesthetics can result in sympathetic blockade, sensory analgesia, and motor blockade. Despite these similarities between spinal and epidural analgesia, there are significant physiologic and pharmacologic differences. Spinal anesthesia involves deposition of a small mass or volume of drug around the nerve root in the subarachnoid space to induce profound, reproducible sensory analgesia, and is therefore virtually devoid of systemic pharmacologic effect. Epidural anesthesia necessitates the use of a large mass or volume of local anesthetic that is injected into the epidural space to bathe the nerve roots. This large volume may result in sufficient systemic blood levels to cause adverse effects and result in clinical complications. Because epidural injection is the most commonly used route in horses, it is the main focus of this chapter.
Anatomic Basis for Neuraxial Anesthesia and Analgesia
Painful stimuli are relayed to the spinal cord through Aδ and C fibers. First-order neurons synapse in the dorsal horn of the spinal cord with several different populations of second-order neurons. Nociception-specific neurons transmit painful stimuli exclusively, and wide dynamic range neurons transmit nonpainful signals. Second-order neurons ascend the spinal cord in multiple tracts, relaying painful stimuli to the brain. The quantitatively most important spinothalamic tract ascends the spinal cord in the ventral white matter contralateral to the site of the stimulation. Activation of these neurons results in spinal reflex responses as well as activation of ascending tracts, which transmit nociceptive information to supraspinal levels to complete the nociceptive pathway.
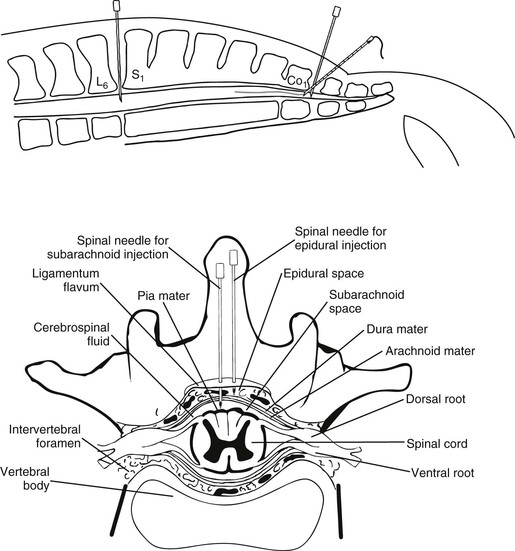
The spinal cord and meninges of horses generally terminate in the midsacral region. For a subarachnoid injection, the spinal canal can be accessed through the space between the sixth lumbar and the second sacral vertebrae at the midline depression. At this lumbosacral joint, the spinal canal is 15 to 20 cm below the skin, which limits the usefulness of this site for a single epidural injection, although it is the ideal location for a combined spinal-epidural technique (Figure 16-1).
An imaginary line joining the two hip joints crosses the midline of the sacrococcygeal joint, but because it is fused in some horses, it is rarely used as an injection site. The spinous process of the first coccygeal bone and, caudal to it, the first intercoccygeal joint, can be palpated in thinner horses. This joint, the most frequently used for caudal epidural anesthesia, is often the first moveable joint in the tail and can be seen and palpated when the tail is raised and lowered. It lies approximately 2.5 to 5 cm cranial to the origin of the tail hairs, at the level of the caudal skin folds that can be seen at each side of the tail when it is raised. Skin, variable amounts of fat, connective tissue between the dorsal vertebral spinous processes, and the interarcuate ligament (ligamentum flavum) overlie the epidural space. The aperture between the two coccygeal vertebral arches, the interarcuate space, can be relatively small in horses, compared with cattle, and can sometimes be difficult to locate with the needle.
Clinical Considerations
Intercoccygeal, or caudal epidural, injection of local anesthetics is a convenient method of inducing analgesia and local anesthesia of the tail and perineal structures in conscious standing horses. This technique has been further developed to provide long-duration analgesia and anesthesia by catheter placement in the epidural space of horses. More recently, opioid, α2-adrenergic agonists, ketamine, and other analgesic and antiinflammatory agents (corticosteroids) have been administered by caudal epidural injection, providing pain relief in both conscious standing and anesthetized recumbent horses.
Technique Description and Requirements
Epidural and spinal techniques can be performed either with a horse standing in stocks (Figure 16-2) or positioned in lateral recumbency after induction of general anesthesia. When a standing position is chosen, the epidural or spinal injection can often be performed rapidly because location of the landmarks is easy. When a horse is positioned on a surgical table in lateral recumbency, however, location of some of the landmarks necessary for the injection is not possible. The procedure can become time-consuming and may fail.

Ideally, the drug or drugs chosen should have a high safety margin and high efficacy and should lack adverse effects. Adverse effects should be reversible with an antagonistic drug. Duration of action should be compatible with the procedure to be performed. Motor and sensory blockade should be expected with the local anesthetic and in some circumstances with α2-adrenergic agonists and ketamine, whereas sensory blockade alone is obtained with drugs such as opioids.
The clinical application of spinal analgesics in horses is recommended for acute and chronic pain control of the hind limb, perineum, tail, and abdominal wall. Time to effect is influenced by the number of molecules retained in the cerebrospinal fluid and spinal tissue and by the dissociation kinetics of the drug. Thus there are differences in onset, spread, and duration that can vary with each drug. Most of the acute and chronic painful situations will involve tissue damage, and the horse will probably benefit from concurrent systemic nonsteroidal antiinflammatory drug treatment.
The use of additive drugs such as epinephrine, phenylephrine, and α2-adrenergic agonists is of some concern because these drugs can potentially reduce blood flow to the spinal cord. The combination of local anesthetics and α2-adrenergic agonists prolongs the motor and sensory effects of the local anesthetic. The mechanism for this prolongation may involve vasoconstriction and antinociception from α2-receptor stimulation.
Onset and Duration of Effect of Drugs
The onset and duration of single or combined anesthetic or analgesic drugs for spinal injections in horses is variable. Some of the combinations are suitable for long-lasting analgesia, whereas others are more appropriate for short-term procedures (Table 16-1). Duration of the motor and sensory block for local anesthetics may be increased when they are combined with a potent vasoconstrictor such as phenylephrine or epinephrine. Other drugs, such as α2-adrenergic agonists (e.g., xylazine and detomidine), also may increase motor and sensory block when combined with local anesthetics.
TABLE 16-1
Drug Regimens Used for Epidural or Spinal Anesthesia or Analgesia in Horses
| Drug | Volume (mL) | Site of Injection | Onset (Duration) (hr) | Comments |
| Epidural Anesthesia/Analgesia | ||||
| Single Drug | ||||
| Lidocaine 1%-2% | 5-8 | Co1-Co2 | 0.5 (0.75-1.5) | Repeated injections of 3 mL at 1-hr intervals |
| Lidocaine 1% | 20 | Co2 | 0.75 (3) | Causes moderate ataxia |
| Mepivacaine 2% | 5-8 | Co1-Co2 | 0.5 (1.5-3) | |
| Bupivacaine 0.2%-0.5% | 5-8 | Co1-Co2 | 0.5 (3-8) | |
| Ropivacaine 0.2%-0.5% | 5-10 | Co1-Co2 | 0.5 (3-8) | Fast onset: 10 min Less risk for ataxia |
| Xylazine 0.17 mg/kg | 10 | Co1-Co2 | 0.5 (1.0-1.5) | May cause sedation/ataxia |
| Detomidine 30 µg/kg | 10 | Co1-Co2 | 0.5 (2-4) | May cause sedation/ataxia |
| Medetomidine* 2-5 µg/kg | 10-30 | Co1-Co2 | 0.5 (4-6) | May cause mild sedation |
| Morphine 0.05-0.2 mg/kg | 10-30 | Co1-Co2 | 1-3 (3-16) | Also useful for CRI (0.5-2 mL/hr) via epidural catheter |
| Methadone 0.1 mg/kg | 20 | Co1-Co2 | 0.5-1.0 (5) | |
| Ketamine 0.5-2.0 mg/kg | 10-30 | Co1-Co2 | 0.5 (0.5-1.25) | |
| Hydromorphone 0.04 mg/kg | 10-30 | Co1-Co2 | 0.5-1.0 (4-5) | |
| Drug Combinations Useful for Balanced Regional Analgesia | ||||
| Lidocaine 2% + xylazine 0.17 mg/kg | 5-8 | Co1-Co2 | 0.5 (4-6) | |
| Lidocaine 2% + morphine 0.1-0.2 mg/kg | 5-8 | Co1-Co2 | 0.5 (4-6) | |
| Bupivacaine 0.125 % + morphine 0.1-0.2 mg/kg | 10-30 | Co1-Co2/L-S | 0.5-0.75 (8->12) | Also useful for CRI (0.5-2 mL/hr) via epidural catheter |
| Xylazine 0.17 mg/kg + morphine 0.1-0.2 mg/kg | 10-30 | Co1-Co2/L-S | 0.5-1.0 (≥12) | |
| Detomidine 30 µg/kg + morphine 0.1-0.2 mg/kg | 10 | Co1-Co2/L-S | 0.5 (24-48) 0.5 (6-8) | Mild to moderate pain |
| Lidocaine 1%-2% + morphine 0.1-0.2 mg/kg + bupivacaine 0.125% | 5 | Co1-Co2 | 0.5-1.0 (0.75-1.5) | Tuohy needle before epidural catheter placement |
| 30 (together) | L-S | 0.5-1.0 (12->24) | Epidural catheter advanced ≥5 cm cranially | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


