Linda A. Dahlgren
Skin Grafting
Traumatic wounds are common in horses and can range from superficial abrasions requiring little or no care to those that are extremely labor intensive and expensive to manage. Veterinarians play a critical role in the treatment of equine wounds and can provide pivotal guidance to owners regarding which wounds can be managed conservatively and which require immediate, aggressive veterinary care. The effects of this decision can mean the difference between a successful return to athletic soundness and chronic lameness or euthanasia. Wound management can be extremely rewarding. One of the key tools in achieving a successful outcome is the use of appropriate skin grafting techniques. Skin grafts provide functional and cosmetic coverage, stimulate wound contraction, and speed the overall healing process. The wounds that most commonly require grafting are large wounds on the body and those on the distal portions of the limb. Degloving wounds on the distal limb segments can be especially troublesome in trying to achieve a satisfactory outcome.
Skin grafting is indicated when the wound cannot be closed surgically or exceeds the capacity to heal by contraction and epithelialization alone. Grafting a granulating wound is a cost-effective treatment. The cost of performing the procedure is often paid for in the time and money saved in bandaging and wound care. Without grafting, many wounds take an exceedingly long time to heal because of the sheer size of the wound and the fact that chronic wounds tend to become static and stop contracting. Chronic wounds require prolonged periods of bandaging and stall confinement, which can become expensive.
Types of Grafts
Skin grafts are classified as either pedicle grafts or free grafts, depending on whether a connection to the donor site is maintained. Pedicle grafts maintain at least one attachment to the donor site from which they receive their blood supply. Free grafts must establish a new vascular connection in the recipient wound bed to survive. Free grafts are used most commonly in equine practice because of the inelastic nature of equine skin and the lack of movable skin adjacent to extremity wounds. Most skin grafts applied to wounds in the horse are autografts; that is, they are grafts transferred from one site to another on the same horse.
A third useful method of categorizing skin grafts is based on the thickness of the graft. Full-thickness grafts include the epidermis and the entire dermis, are highly durable, and provide a good cosmetic outcome; however, they have traditionally been thought to have a lower rate of graft acceptance than split-thickness grafts. The latter grafts include the epidermis and a variable portion of the dermis and sacrifice durability and cosmetic outcome in favor of a higher rate of graft survival. The selection of the type of graft best suited to an individual case should be based on the size and location of the wound, desired cosmetic outcome, financial constraints of the owner, equipment available, and expertise of the practitioner.
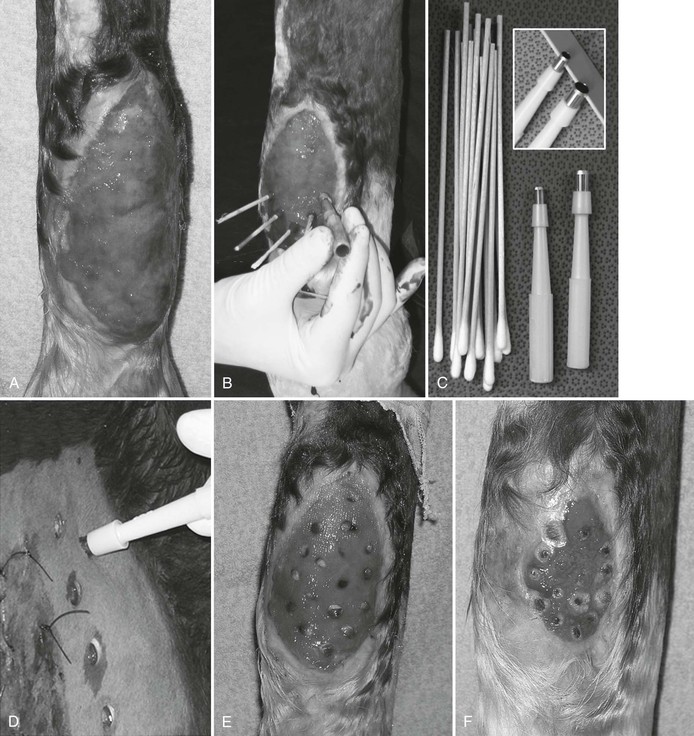
Island grafts or seed grafts are small pieces of full- or split-thickness skin that are placed into the granulating wound bed and subsequently produce a halo of epidermis around them. Common types of island grafts include punch grafts, pinch grafts, and tunnel grafts. Punch and pinch grafts are technically easy to perform in the standing horse under moderate sedation and provide a cost-effective means of wound management for a large percentage of common equine wounds. Tunnel grafts are performed less frequently but can be ideal for areas that cannot be bandaged, such as the body or where motion is a problem (e.g., the dorsal aspect of the hock).
Sheet grafts are large pieces of full- or partial-thickness skin that are harvested and applied in one large intact piece onto the granulating wound. In the horse, sheet grafts are most commonly split thickness to increase the likelihood of survival of the graft. A recent small case series, however, reported a good success rate with use of full-thickness grafts to treat wounds caused by laceration or tumor resection. In addition, it is common to fenestrate or mesh sheet grafts by creating a series of staggered cuts in the skin that allow it to be expanded to several times its original size. Not only does meshing the graft allow a much larger area of wound to be covered than the size of the graft itself, the mesh expansion provides holes that allow for drainage of serum, blood, or exudate from under the graft, preventing graft disruption. The mesh openings allow contact of topical antimicrobials with the granulation bed itself rather than just the graft surface. Regardless of the type of graft selected for a particular application, meticulous preparation of the recipient site or wound bed and attentive aftercare are critical to achieve a successful outcome.
Graft Physiology
Initially, during the adherence phase, grafts are held in place by fibrin that is exuded from the recipient site and receive temporary nutrition through passive diffusion from surrounding fluid, also known as plasmatic imbibition. Revascularization of the grafts begins 24 to 48 hours after grafting, and eventually the host vessels anastomose with vessels from the graft to supply nutrition, a process known as inosculation. In addition, revascularization of the graft is established by capillary buds from the recipient site invading the graft. By 3 to 4 days, fibroblasts have begun to invade the graft and form adhesions between the graft and recipient site, and by 9 to 10 days, grafts are firmly attached through fibrous adhesions and functional vessels crossing the graft–host interface.
Pinch grafts initially appear as dark spots within the granulation bed approximately 1 to 2 weeks after grafting as the granulation tissue overlying the grafts sloughs. By 3 to 4 weeks after punch or pinch grafting, a ring of pink epithelium can be detected around the grafts, and by 42 to 56 days, hair begins to grow from the grafts. A 60% to 75% survival rate can be expected with either punch or pinch grafting; however, it is not uncommon to have greater than 90% graft survival. One important advantage of seed grafts is that the failure of one or several individual grafts does not translate to complete graft failure. Grafting a granulating wound stimulates contraction and epithelialization of the original wound (Figure 126-1), and this makes a significant contribution to the final outcome.
Preparation of the Wound Bed
A healthy recipient bed that is free of infection and devitalized tissue and has a good vascular supply is critical to a successful outcome in any skin-grafting procedure. One rule of thumb is that if a granulating wound is healthy enough to have a margin of new epithelium, it is healthy enough for grafting. If one portion of a wound is ready for grafting and another is not, island grafts may be used to graft only a selected portion of a wound without sacrificing a successful outcome. The grafting process speeds healing by reducing the granulating surface area, which results from stimulation of wound contraction and epithelialization. Additional grafts can be added later.
In preparation for grafting, the granulating wound bed should be sharply excised to, or just below, the level of the surrounding skin with a scalpel blade or a single-edge razor blade. Excision of granulation tissue should be performed from the ventral portion of the wound to the most proximal to avoid obscured vision from hemorrhage as trimming progresses. Because granulation tissue lacks a nerve supply, trimming can be readily performed in the standing horse, often without sedation. Care should be taken to avoid the epithelial margin because this area is sensitive. Trimming the granulation bed should be performed days to several weeks before grafting, depending on the health of the granulation bed. A fully granulated wound may require a single trim 24 to 48 hours before grafting, whereas a less mature wound may require several rounds of trimming to achieve a smooth, level wound bed without crevices and pits. Wounds that have exposed bone and irregular, pitted granulation tissue that contains fibrin are not suitable for grafting (Figure 126-2). These wounds require repeated trimming at 4- to 7-day intervals until a smooth, healthy granulation bed is achieved and the bone is fully covered with granulation tissue. Trimming an older, more chronic granulating wound encourages development of a younger, vascular bed of granulation tissue consistent with a successful outcome. Chronic wounds may require 3 to 4 days to form a healthy granulation bed after trimming. Because of the marked vascularity of granulation tissue, a heavy bandage is applied after trimming to control hemorrhage. The bandage is routinely replaced after 24 hours, and a clean bandage is applied for 24 to 48 hours before grafting. Application of an antibacterial cream or ointment such as triple-antimicrobial ointment or silver sulfadiazine cream can help reduce the bacterial count on the surface of the wound. Application of ticarcillin disodium–clavulanate potassium powder to the wound surface is an effective means of controlling bacterial infection. The powder is “puffed” onto the wound to create a thin coating.

< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree