CHAPTER 24Selected Reproductive Surgery of the Broodmare
The notes herein are a compilation of some of the techniques that are used at the Goulburn Valley Equine Hospital and are not intended as an exhaustive, heavily referenced treatise of all available techniques. No attempt has been made to discuss all reproductive techniques or conditions requiring intervention. The procedures herein work very well for us. However, readers should be aware that different methods are employed successfully by others. We would be grateful to those who have different ideas and experiences if they would communicate them by e-mailing Dr. McKinnon at aom@iinet.net.au. Many of the techniques presented are modifications of existing techniques, newer techniques, and/or areas we feel warrant special attention. We have assumed that readers are at least familiar with both relevant anatomy and standard documented surgical correction of reproductive-related problems.
PATIENT SELECTION
In consideration of the client, patient, and general perception of our professional abilities as well as the merit of our interference, care should be exercised to select only those patients that are likely to respond favorably to surgery (Box 24-1). For example, it is pointless to perform a sophisticated, expensive surgery for vesico vaginal reflux if the mare has sustained chronic uterine damage and fibrosis that will render her infertile despite an excellent surgical outcome. Full reproductive evaluation is necessary before surgery in any candidate subjected to physical insults such as recto-vaginal lacerations and fistulas for longer than 1 year.
SEDATION AND ANESTHESIA
Most procedures are performed with the mare standing, using local infiltration or epidural anesthesia. Apart from minor procedures (Caslick’s vulvoplasty), we prefer to have mares tranquilized and restrained in appropriate stocks such as facilities for cross tying and/or tail elevation. Tranquilization and analgesia are provided most commonly with intravenous (IV) detomidine (mg) and butorphanol (mg). Longer surgeries may require the repeated IV use of low doses of xylazine (100 mg). Cost and length of tranquilization/analgesia are important considerations. Some have other physiological effects, such as increased urinary output with xylazine. Detomidine provides excellent tranquilization and analgesia; however, effects are often still apparent hours after administration. Epidural anesthesia may be extremely effective; however, variation in response and individual susceptibility and time before appropriate anesthesia is obtained occasionally make it less rewarding than tranquilization and local infiltration for some of the procedures discussed here. Techniques for epidural anesthesia have been discussed elsewhere.1 One word of warning: epidural administration of more than 7 to 9 ml of 2% local anesthetic to a 500 kg mare can be associated with loss of motor control to the hind limbs and recumbency. These mares are difficult to manage and may require support for 2 to 4 hours.
Epidural injection of xylazine for perineal analgesia has been reported to be very efficacious. A dose of 0.17 mg/kg (around 75-100 mg in an average horse) was as effective as local anesthetic agents for analgesia and had nil or minimal effects on depression of motor nerves in the lumbosacral intumescence. Another advantage was demarcation of the area of analgesia with an area of sweating (dermatome) that was consistent both temporally and topographically.2 In our experience the perineal dermatome is not always obvious. In addition it takes around 35 to 40 minutes for good analgesia to be recognized associated with xylazine epidural anesthesia. Currently we prefer to use a combination of xylazine (70 mg) and lidocaine (60 mg [3 ml]), q.s. saline to 10 ml for most horses. With this regime, loss of tail tone has occurred associated with a successful “block” within 5 to 10 minutes and surgery generally has begun by approximately 30 to 45 minutes post administration. Our most common method of epidural anesthesia is to begin with the infusion of 1 ml of local anesthetic through a 25 gauge needle subcutaneously above the first moveable coccygeal/sacral joint (usually C1 and C2). Next, a 38-mm, 18-gauge needle (bevel forward and introduced at 45 degrees) that has a small amount of fluid left to create a meniscus on the needle hub is introduced through the local bleb. Recognition of the fluid being aspirated into the needle infers correct placement, and the appropriate amount of solution is injected slowly into the epidural space whilst continually evaluating the ease of administration to ensure that the needle tip is still in place.
VESTIBULE AND VULVAL LIPS
Pneumovagina
There are 3 barriers to aspiration of air and contaminants into the cranial reproductive tract.
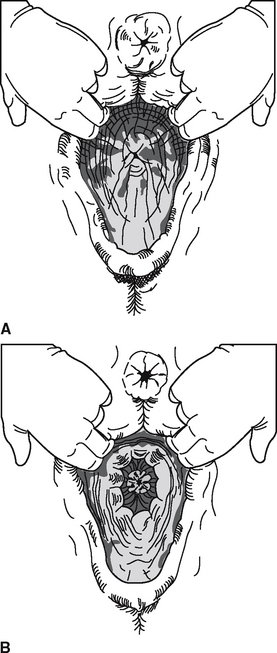
Recognition of potential candidates for pneumovagina are made from anatomical observations3 (i.e., predisposition is associated with a low pelvis, tilted vaginal lips, and a sunken anus) (Figure 24-1). If possible, mares should be examined during estrus when the reproductive tract is relaxed. Parting the vulval lips results in loss of integrity of the vestibular sphincter and an audible ingress of air to the cranial vagina. Recognition of foamy exudates from the vaginal lips may often be noted during rectal examination. In addition, ultrasonography has been used to visualize air in the uterus.4 If in doubt after clinical evaluation regarding a mare’s potential to aspirate air into the vagina, we recommend treating by surgery all mares that have been barren one or more breeding seasons, unless other causes of reduced fertility are obvious (i.e., stallion, farm management).
Caslick’s Vulvoplasty
Caslick’s vulvoplasty was first described by Dr. E. A. Caslick in 1937 and involves apposition of the vulval lips.5 Local anesthesia of vulval lips, removal of a thin portion of mucosa from the mucocutaneous junction, and apposition of the cut edges is simple, quick, and effective. Length of apposition is determined by height of pelvis relative to vulval lips. In general the join should continue to a point at least 3 to 4 cm below level of the pelvis, and approximately 3 cm should be left unopposed to allow for urination. If this is not possible, other surgical techniques (see below) may be necessary.
Variations.
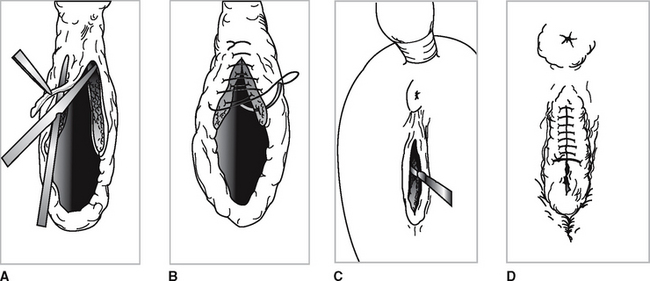
Placement of a breeding stitch (usually doubled heavy gauge suture material or umbilical tape) will save unnecessary replacement and facilitate breeding and some manual vaginal manipulations for treatment (Figure 24-2, D). Care is needed with natural service to prevent penile trauma. We routinely treat or bred (AI) mares by passage of an infusion pipette into the vagina (past the vestibular sphincter) and use rectal manipulation of the pipette through the cervix similar to, but with a little more difficulty than cattle.
Episioplasty
This procedure is used in cases with more severe anatomic abnormalities where the Caslick vulvoplasty is ineffective and in mares with extensive or repeated second-degree perineal lacerations. Technically the previous surgery is an episioplasty as well; however, we use the term to describe the more extensive procedure previously referred to as (1) a deep Caslick, (2) the Gadd technique, or (3) a perineal body reconstruction.6 The procedure is designed to restore some degree of function to the perineal body. (Figure 24-3)
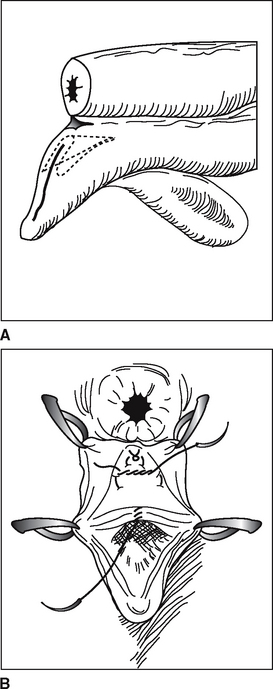
Urovagina
Pooling of urine in the vagina is a problem for a variety of reasons. In 1985 Jay Belden, then of Fossil Creek Farms, showed me his technique for urovagina. Before this time, both of us had tried other described techniques and were not particularly happy with the outcome. After approximately 34 surgeries between us using Jay’s technique, we decided the technique was efficacious and should be presented. The resultant publication is summarized below.4
The midline caudal border of the transverse vaginal fold is grasped with Allis tissue forceps and retracted caudally toward the surgeon 2 to 4 cm cranial from the caudal border of the transverse fold. A horizontal transverse incision to the submucosa is made with a No. 12 Bard Parker blade (Figure 24-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree