Véronique A. Lacombe
Seizure Disorders
Seizure disorders are a diverse and common set of chronic neurologic disorders in humans and dogs. Seizures are less common in horses, compared with other species, because of a relatively high seizure threshold. A seizure is characterized by a sudden, often catastrophic event, and seizures may be referred to as fits, attacks, strokes, convulsions, or epilepsy. However, true seizures (i.e., “epileptic” seizures) are clinical manifestations of rapid, excessive, or hypersynchronous abnormal neuronal activity from the cerebral cortex that results in involuntary alterations of motor activity, consciousness, autonomic functions, or sensation. Therefore a true epileptic seizure has a specific neural origin and can occur as a single event or be recurrent.
Similar to the classification used in small animal epileptology, seizure disorders in horses can be classified by type (partial vs. generalized). Seizures that arise from a discrete area of the cerebral cortex in which a small number of neurons discharges spontaneously are classified as partial seizures and subcategorized as simple (if alertness and normal mentation are maintained) or complex (with impaired consciousness). In partial (i.e., focal) seizures, the spontaneous epileptogenic focus, which mostly arises at the periphery of the cerebrum, does not spread and primarily results in localized clinical signs. Seizures that involve the entire cerebral cortex are classified as generalized seizures and are subcategorized as follows: generalized seizures that originate from both cerebral hemispheres from the onset are referred to as primary generalized seizures, and generalized seizures that progress from simple or complex partial seizures are referred to as secondary generalized seizures. Seizures are also referred to as reactive when associated with a temporary systemic disease (e.g., electrolyte imbalances or other metabolic disorders) and normal underlying brain function. Status epilepticus has been defined as a state of more than 30 minutes of continuous seizure activity or at least two sequential seizures without full recovery of consciousness; this condition is uncommon in horses. Epilepsy (from the Greek word epilambanein, meaning to be seized or attacked) is a condition characterized by an enduring predisposition to generate recurrent (two or more) seizures, and includes a variety of disorders reflecting underlying chronic brain dysfunction. When seizures occur repetitively within a 24-hour period, the cluster of seizures is considered a single episode. Epilepsy is classified as primary (i.e., of genetic origin) and secondary or acquired (i.e., symptomatic and cryptogenic). Epilepsy is classified as symptomatic if a structural brain disorder is identified on the basis of abnormal results of neurodiagnostic testing and as cryptogenic (of unknown etiology) if recurrent seizures develop in the absence of abnormalities in neurodiagnostic test results. Intracranial disease should still be suspected, even in the face of an unremarkable workup, especially if diagnostic testing was not complete. Epilepsy from genetic predisposition, also referred to as idiopathic, is rare in horses, with the exception of Arabian foals with juvenile idiopathic epilepsy.
Etiology and Pathogenesis
Seizures do not refer to a specific disease but rather to a diverse category of disorders, which include both intracranial and extracranial diseases. Intracranial conditions, which are the most common causes of seizures, include neoplasia, head trauma, cerebral abscess, vascular events, encephalitis or meningitis, congenital abnormalities, and intoxications (e.g., lead, metaldehyde, moldy corn, and locoweed). Cholesterol granulomas have also been reported in horses with seizures. Extracranial conditions include electrolyte or metabolic disorders (e.g., hepatic encephalopathy, hyponatremia, hypocalcemia, and uremia) and septicemia. The most common causes of seizures in adult horses are brain trauma, neoplasia, and hepatic encephalopathy. The most common causes of seizures in foals are hypoxic-ischemic encephalopathy, head trauma, bacterial meningitis, and idiopathic epilepsy in Arabian foals.
Irrespective of the etiology, the pathogenesis of epileptic seizure involves abnormal hypersynchronous electrical activity of neurons, caused by an imbalance between excitatory and inhibitory neural transmitters. If this balance shifts toward excessive excitation (theory of excitatory postsynaptic potentials) or decreased inhibition, a prolonged depolarization of neuronal aggregate (referred to as paroxysmal depolarizing shift) will occur. Several mechanisms are thought to cause paroxysmal depolarizing shifts and include increased excitatory neural transmitters (glutamate), decreased inhibitory neural transmitters (γ-aminobutyric acid [GABA]), alteration in neural transmitter receptor sites, or a derangement in the internal cellular metabolism of the neuron. Notably, much research has focused on glutamate, the principal excitatory neurotransmitter in the brain, and its receptor complex, the N-methyl-d-aspartate (NMDA) receptor. A wave of depolarization reaching the presynaptic nerve terminal induces release of glutamate. Glutamate binds to NMDA receptors on the postsynaptic membrane, opening sodium and calcium channels and leading to entry of these ions into the postsynaptic neuron. This ionic movement leads to postsynaptic depolarization and generation of an excitatory postsynaptic potential. In contrast, when GABA, the major inhibitory neurotransmitter, attaches to the postsynaptic GABAA receptor, chloride channels are opened. Chloride enters the postsynaptic neuron, causing a state of hyperpolarization and an inhibitory postsynaptic potential. Failure of local surrounding inhibitory zones to prevent the spread of the initial focal epileptogenic activity allows the seizure focus to progress and spread diffusely throughout the cortex. After a critical mass of neurons has fired, uncontrolled electrical activity spreads over the cerebral cortex, possibly generating a seizure.
Clinical Signs and Diagnosis
The clinical presentation of seizure disorders reflects the area and extent of the cerebral cortex involved and is independent of the etiology. Clinical presentations can vary widely, ranging from mild alterations in consciousness to focal muscle fasciculations and recumbency with tonic-clonic struggling. Partial seizures, caused by a localized site of abnormal discharge, result in localized motor signs or sensations such as asymmetric twitching of a limb, facial twitching, excessive chewing, compulsive running, or self-mutilation. The duration of a partial (focal) seizure is variable, and a partial seizure may lead to a generalized seizure. Generalized seizures, which involve the entire cerebral cortex, result in generalized bilateral motor activity over the body, including convulsive seizures (formerly referred to grand mal), nonconvulsive seizures (formerly referred to as petit mal), or myoclonic seizures. In addition, one may observe three clinical features in a generalized seizure, including loss of control (to various degrees), the episodic (paroxysmic) nature of the attacks, and the repetitive pattern. In addition, an epileptic seizure has generally three distinct clinical periods, which include a preictal, ictal (i.e., seizure episode), and postictal period. Just before the seizure (i.e., in the aura or preictal phase), the horse may have abnormal behavior such as restlessness, signs of anxiety, and uneasiness. The postictal phase can range from mild depression to stupor and blindness and can last for hours to days. Therefore neurologic examination should be performed during the interictal period.
Diagnosing seizures in horses can be challenging. Similar to other species, epilepsy of unknown origin accounts for most recurrent seizures, and the modalities for imaging the brain in adult horses are limited. In addition, it is important to differentiate true seizures from noncerebral clinical conditions that could mimic seizures, such as tetanus, botulism, and hyperkalemic periodic paralysis, and from painful conditions, such as colic, limb fractures, and exertional myopathy. In the latter conditions, horses do not lose consciousness but remain bright and alert. Furthermore, it may be difficult to differentiate epileptic seizures from syncope and sleep disorders. For instance, cardiac arrhythmias, acquired structural heart disease (heart failure), or circulatory shock can all precipitate syncopal episodes, which could be confused with seizures. Narcolepsy and cataplexy can also be confused with seizures, although most narcoleptic horses remain standing with the head hanging close to the ground. Whenever possible, video surveillance should be used to record the events and to monitor the horse’s sleep patterns.
Because many horses are unobserved for long periods of the day and may return to normal activity after a seizure without lingering neurologic signs, seizuring might only be suspected after recognition of unexplained abrasions and lacerations to the head, eyes, or limbs. At other times, the caretaker may identify a change in the horse’s attitude or behavior, which could be a prodromal sign of an impending seizure. The caretaker should be questioned thoroughly to determine the duration and frequency of the episodes, provoking and risk factors (e.g., an inadvertent intracarotid injection, traumatic event, thunderstorms, or fireworks), febrile episodes, exposure to drugs, recent behavioral changes, and the seizure history of the dam, sire, and other siblings. If the horse is kept outdoors, any possible toxic causes should be ruled out, as well as exposure to other animals. The latter is important because rabies should always be on the list of differential diagnoses when a horse is presented with seizures.
Physical examination should rule out noncerebral conditions that mimic seizure activity and elucidate the presence of systemic extracranial disease that could trigger seizures. Evidence of nasal discharge or epistaxis may indicate a sinonasal tumor or infection that extends intracranially. Although neurologic deficits may be observed if the seizures are caused by a structural cerebral problem, the interictal neurologic examination can be normal in many instances.
A complete blood count and serum biochemistry analysis should elucidate the presence of systemic extracranial disease that could provoke seizures. The complete blood count and fibrinogen values could point toward inflammation (leukocytosis and hyperfibrinogenemia) or viral infection. A complete serum biochemistry profile (including sodium, magnesium, potassium, and calcium concentrations) should be performed to rule out metabolic abnormalities. Serum bile acids and ammonia concentrations should be determined if hepatic encephalopathy is suspected. Detection of hypoglycemia may indicate a cause for seizures in both neonates and adults, although hypoglycemia-induced seizures are rare. Renal disease and hyperlipidemia should be ruled out, as well. Severe hyponatremia has been described in foals with neurologic deficits, including seizures. Hyperkalemia is the hallmark of hyperkalemic periodic paralysis, the clinical signs of which can resemble seizure-like activity.
Cerebrospinal fluid (CSF) analysis is a valuable tool in determining the etiology of seizures caused by an active structural cerebral abnormality. High total protein concentration and cell counts are commonly seen in infectious conditions. Neutrophilia is suggestive of viral encephalitides, and serologic testing of serum and CSF is then warranted, along with culture of the CSF. Testing for equine protozoal myeloencephalitis should also be considered because seizures have been reported in horses with this disease. In general, collection of CSF in seizuring horses should be performed at the atlanto-occipital space, which is the site closest to the suspected neuroanatomic lesion, to increase the likelihood of finding cytologic abnormalities in the spinal fluid and therefore determining the etiologic agent (see Chapter 84 for more information on sampling CSF fluid). If altered CSF pressure is suspected or general anesthesia is a concern because of risk or cost, the lumbosacral space is an alternative site, provided that the lumbar puncture technique can be safely performed in the standing and sedated animal.
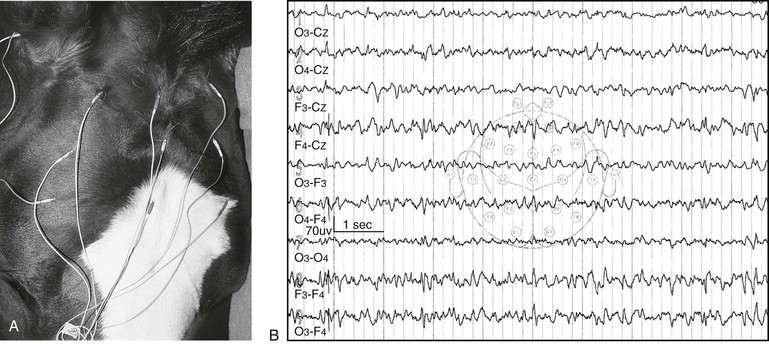
Electroencephalography (EEG) is a noninvasive neurophysiologic diagnostic technique, defined as the graphic recording of the rhythmic bioelectrical activity arising predominantly from the cerebral cortex. It has been extensively used in humans and small animals for the investigation and management of epilepsy, in particular in establishing probability of recurrence, need for treatment, and prognosis. Electroencephalography may be performed on sedated or anesthetized horses. Although investigation in horses is limited, EEG is also sensitive for diagnosis of intracranial disorders in this species. Therefore accurate interpretation of the EEG recording can provide useful information with regard to the presence of cerebral disease, although changes are not pathognomonic of a disease but rather reflect the kind of process occurring (e.g., acute vs. chronic, focal vs. diffuse, and inflammatory vs. degenerative). One should assess the background of the EEG recording for abnormal frequency and amplitude and asymmetric patterns between regions. Focal, multifocal, or generalized epileptiform activity can be recorded on the EEGs of epileptic patients, depending on the localization of the discharges and the extent of the cerebral cortex involved (Figure 87-1). In addition, epileptiform paroxysmal activity, which is defined as abnormal paroxysmal transient events, such as spikes, sharp waves, and spike-and-wave discharges, supports the diagnosis of seizures. It should be remembered that horses with extracranial diseases such as metabolic disorders may also have abnormal EEG recordings. The main limitations of this electrodiagnostic test are related to the facts that (1) only electrical activity arising from the superficial part of the cerebral cortex is recorded; (2) the establishment of normal values remains difficult because frequency and amplitudes are state dependent (i.e., the states of wakefulness, drowsiness, sleeping, and being sedated vs. anesthetized) and vary with age; (3) extensive expertise is required for a clinician to interpret the reading; and (4) the window of recording may not have been long enough to record interictal paroxysmal epileptiform discharges. Therefore the absence of epileptical activity on an EEG does not necessarily rule out seizures. Frequent and prolonged EEG monitoring, such as with a 24-hour ambulatory EEG, is routinely performed in humans, but this modality has not been used in horses.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


