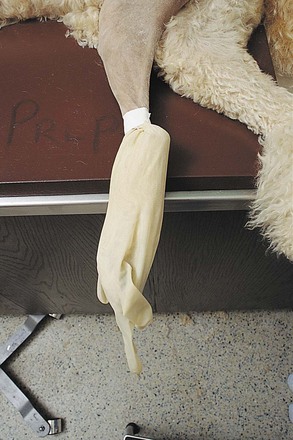
Chapter 5 The prevalence of SSI is a major concern because of the associated increased incidence of morbidity and mortality, length of hospitalization, and cost of care for postoperative patients. Although similar data are not available in veterinary medicine, it has been shown that preventing a single case of SSI caused by a methicillin-resistant Staphylococcus aureus (MRSA) can save human hospitals as much as $60,000 (Anderson et al, 2009). Preventive preoperative measures that can reduce the risk of SSI include administration of antimicrobial prophylaxis (see Chapter 9) and proper utilization of skin antiseptic agents for the surgical team (see Chapter 6) and the patient. In a comprehensive study of 225 matched pairs of human patients with and without SSI, infected patients were twice as likely to die compared with uninfected patients (Kirkland et al, 1999). Thus, it is imperative that veterinarians and their staff be proactive in preventing infection during surgery by using proper techniques and solutions to prepare the skin for surgery. In adult animals, food intake generally is restricted 6 to 12 hours before induction of anesthesia to avoid intraoperative or postoperative emesis and aspiration pneumonia. Access to water generally is not curtailed. Operations of the large intestine (see Chapter 20) often require specialized preparations (e.g., dietary restriction for 48 hours) or enteric antibiotics (e.g., oral kanamycin, neomycin, penicillin G, metronidazole), or both. Food should not be withheld from young animals for longer than 4 to 6 hours because hypoglycemia may occur. Hair should be removed as close to the time of surgery as possible, and hair removal should always occur outside the room where the surgical procedure will be performed (e.g., in the prep room). Removal of hair the night before surgery is associated with a significantly higher superficial skin infection rate than removing the hair immediately before surgery. The surgical site should be identified and hair should be liberally clipped around the proposed incision site, so that the incision can be extended within a sterile field (Fig. 5-1). The prepared area should be large enough to accommodate extension of the incision, additional incisions (if needed), and all possible drain sites. It also must be large enough that inadvertent wound contamination is avoided if the drapes move during the procedure. A general guideline is to clip at least 20 cm on each side of the incision. The hair can be removed most effectively with an electric clipper and a No. 40 clipper blade. Patients with dense hair coats may be clipped first with a coarser blade (No. 10); the higher the blade number, the shorter the remaining hair. Clippers should be held in a “pencil grip,” and initial clipping should be done with the hair growth pattern. Subsequent clipping should be against the pattern of hair growth to obtain a closer clip. Depilatory creams are less traumatic than other hair removal methods, but they induce a mild dermal lymphocytic reaction. They are most useful in irregular areas where adequate hair removal is difficult. Razors occasionally are used for hair removal (e.g., around the eye) but can cause microlacerations in skin that may increase irritation and promote infection. After hair removal is complete, loose hair is removed with a vacuum. For limb procedures in which exposure of the paw is unnecessary, the paw can be excluded from the surgical area by placing a latex glove over the distal extremity and securing it to the limb with tape (Fig. 5-2). The glove should be covered with tape or self-adherent bandaging tape (i.e., Vetrap [3M, St Paul, Minn], COHERE [Dome Enterprises, Dover, NH], Coban [Andover Healthcare Inc, Salisbury, Mass]). The foot is then “draped out” of the sterile field (see later). To enhance manipulation of limbs during surgery, a hanging-leg preparation may be done. The limb is circumferentially clipped and then is hung from an intravenous (IV) pole during prepping to allow all sides to be scrubbed. Before the animal is transported to the surgical suite, the incision site is given a general cleansing scrub, and ophthalmic antibiotic ointments or lubricants are placed on the cornea and conjunctiva. Studies suggest that using clean, rather than sterile, supplies for this initial cleansing prep does not influence the infection rate if the skin is intact (Cheng et al, 2001). Lesions, eruptions, abrasions, irritations, rashes, dermatitis, burns, denuded or traumatized areas, or other similar medical conditions that could provide a portal of entry for a pathogen should not be present. In male dogs undergoing abdominal procedures, the prepuce should be flushed with an antiseptic solution (Fig. 5-3). The skin is scrubbed with germicidal soaps to remove debris and reduce bacterial populations. The area is lathered well until all dirt and oils have been removed. This is a generous scrub that often encompasses the hair surrounding the operation site to remove unattached hairs and dander that may be disturbed during draping.
Preparation of the Operative Site
Dietary Restrictions
Treatment of Hair
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine