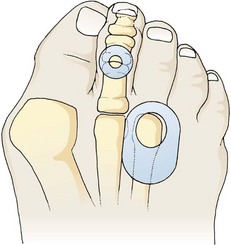
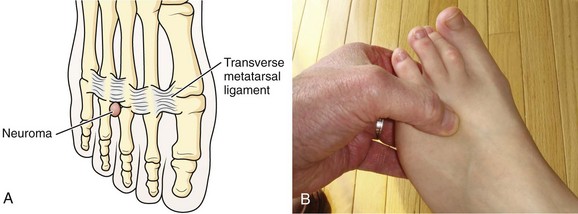
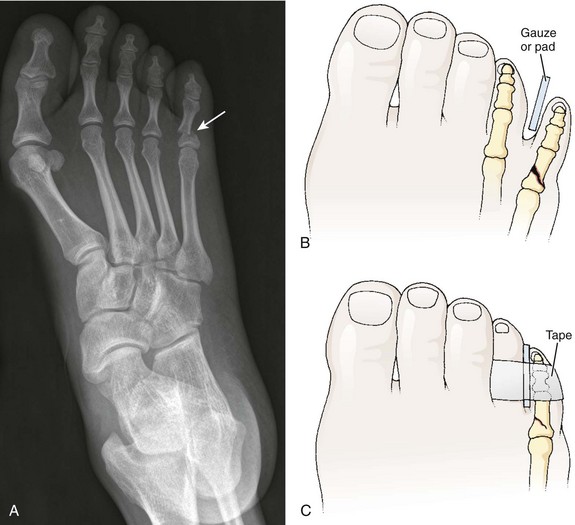
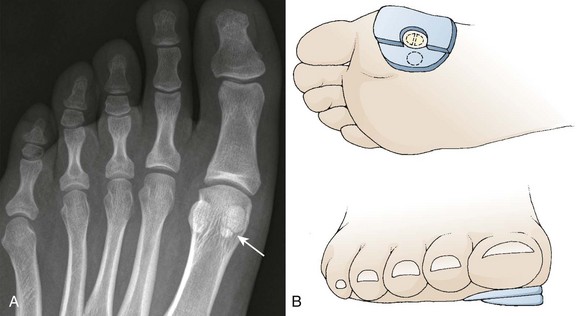
Chapter 51 Normal daily activities cannot easily be accomplished without walking, so patients with painful or infectious conditions of the feet often seek medical attention. This chapter focuses on procedures performed for common maladies of the foot. Other procedures on the foot are described elsewhere in this text, including anesthesia of the foot and ankle (see Chapters 29 and 31), management of nail bed injuries (see Chapters 35 and 37), incision and drainage of paronychia (see Chapter 37), joint fluid analysis (see Chapter 53), management of common dislocations of the foot (see Chapter 49), and splinting (see Chapter 50). Footpads redistribute pressure over an inflamed, tender area of the foot. The particular type of footpad and its placement depend on the condition being treated (Fig. 51-1). Commercially available aperture footpads are recommended for the temporary relief of warts, corns, hyperkeratoses, and bunions. Verruca virus introduced into the plantar surface of the foot may produce a painful hyperkeratotic lesion, commonly referred to as a “plantar wart,” on the sole of the foot. A simple callus may be painful and result in the formation of a “hard corn” when formed over the bony prominence of a digit. Once recognized and after other conditions are ruled out, definitive care of these lesions is rarely indicated in the ED. A bunion develops when unbalanced forces applied to the first metatarsal cause lateral displacement of the distal end of the hallux. Bunions typically form in women wearing heeled shoes with narrow toe boxes. The patient may complain of numbness over the distal, medial aspect of the first toe as a result of compression of the terminal branch of the medial dorsal cutaneous nerve. The mechanical forces that precipitate bunion formation may also cause other painful conditions, including intermetatarsal neuromas, hammertoes, ingrown toenails, corns, and calluses. Bursitis may develop over the medial bony prominence of the first metatarsophalangeal (MTP) joint. Self-adherent bunion pads placed over the first MTP joint may provide temporary relief (Fig. 51-2). In the ED, treat patients suffering from these common disorders with analgesics and footpads followed by referral for definitive care. Recommend that the patient avoid wearing the offending shoes. Consider gout when evaluating pain over the first MTP joint, particularly in the presence of other signs of inflammation (e.g., redness, swelling, warmth). Heel spur pain can be quite bothersome and chronic or recurrent. This condition is not easily remedied in the ED, and after other conditions are ruled out, minimal intervention with podiatric referral is often the best course of action. Patients typically have pain over the medial border of the plantar aspect of the calcaneus. The pain gradually worsens over a period of months. A bony prominence that begins as periostitis extends from the medial aspect of the calcaneal tuberosity into the central plantar fascia and may be seen on radiographs. Radiographs of the calcaneus that do not demonstrate a bony spur suggest plantar fasciitis (see the section “Painful Conditions of the Plantar Surface of the Foot” later in this chapter), even though many patients with plantar fasciitis have plantar calcaneal and Achilles spurs. Plantar calcaneal heel spurs are found in nearly 15% of the population, only 30% of whom have heel pain. Although many persons with heel spurs are asymptomatic, 75% of patients with heel pain have heel spurs.1 However, radiographs have little value in evaluating nontraumatic heel pain because they rarely demonstrate radiographic abnormalities that prompt additional treatment.2 Shoe supports with a heel pad or cup or a doughnut-shaped orthotic often help reduce the discomfort by redistributing weight. Few randomized, controlled trials have evaluated steroid therapy; those that have do not provide substantial evidence supporting its long-term efficacy.3,4 Treatment of the painful site is done with 10 to 20 mg of methylprednisolone injected from the medial aspect of the foot while avoiding the sensitive plantar surface. Some evidence suggests that injecting 25 mg of prednisolone acetate into the medial aspect of the heel provides partial pain relief at 1 month in comparison to lidocaine only, but no advantage can be detected at 3 months.5 A short-leg walking cast may be effective in some patients with recalcitrant heel pain.6 There is little evidence to suggest that specific interventions aimed at reducing heel pain are superior to conservative, supportive treatment alone. Although retrocalcaneal bursitis and Achilles tendinopathy, formerly referred to as Achilles tendinitis, are anatomically distinct, the clinical findings are similar. Pain at the insertion of the Achilles tendon is worsened with prolonged standing or walking and is aggravated by passive or active range of motion in both conditions. Directed palpation can distinguish one entity from the other, but both are treated similarly. Tenderness of the Achilles tendon suggests tendinopathy, whereas tenderness between the tendon and the calcaneus suggests retrocalcaneal bursitis. Achilles tendinopathy has been noted to develop spontaneously after the use of quinolone antibiotics, occasionally with rupture. The condition may occur during quinolone use or a few weeks after therapy and prompts immediate discontinuation of use of the drug if recognized. Rest, elevation, ice, NSAIDs, heel pads, and an open-backed shoe provide relief in the majority of patients. A corticosteroid injection is not usually performed, but it may provide some relief, although its superiority over conservative measures is unproved. Repeated steroid injection is associated with Achilles tendon rupture.7 Injection of platelet-rich plasma (PRP) as treatment of Achilles tendinopathy has gained some support among sports medicine physicians, but recently published studies have failed to demonstrate short- or long-term improvement in pain or function when PRP injection is compared with placebo.8,9 Osteochondrosis of the posterior calcaneal apophysis may cause pain worsened by activity in children between 7 and 10 years of age. It is thought to represent an overuse syndrome in an athletically active child with tenderness in the posterior heel region.7,10 Treat this self-limited condition with rest, ice, and heel pads. Radiographs are not indicated unless other diagnoses are suspected.11 Activity is resumed when the pain abates. Repeated microtrauma to the plantar aponeurosis causes pain on the plantar surface of the foot (Fig. 51-3A). Plantar fasciitis is typically unilateral and found in women who wear high-heeled shoes. The pain is maximally severe in the morning or after prolonged sitting and improves after walking, often referred to as “first-step pain.” Some patients with plantar fasciitis may also have a calcaneal heel spur, but the presence or absence of this radiographic finding is clinically irrelevant. Pain is elicited with palpation (see Fig. 51-3B), toe walking, or passive stretching of the plantar aponeurosis. Frequently, this annoying condition resolves spontaneously, but resolution is slow, with as long as 6 to 18 months being needed. Conservative therapy, including rest, elevation, ice, and NSAIDs, results in a satisfactory outcome after 6 to 8 weeks in 90% of patients.12 The pain improves over time in most patients with or without NSAIDs, although the addition of NSAIDs appears to increase pain relief when compared with conservative treatments alone.13 The emergency clinician can do little to treat this chronic, distressing condition. Stretching exercises each morning and evening can be suggested (see Fig. 51-3D). Night splinting to keep the foot dorsiflexed and custom orthoses made from the patient’s foot impression can be very helpful but usually require referral to podiatry for proper fitting (see Fig. 51-3C). Corticosteroid injection is used by some clinicians; its benefit remains unproved, however. A single injection may be warranted as supplemental therapy in resistant cases. Repeated injections of corticosteroids should be avoided and have been associated with rupture of the plantar fascia and fat pad atrophy.14 In a recent study, 50 units of botulinum toxic type A injected into the plantar fascia decreased pain in comparison to placebo but did not cure the disease.15 A forefoot neuroma, also known as Morton’s neuroma, is a painful condition of the plantar surface of the foot. It most commonly affects women who wear high-heeled shoes. The neuroma forms after chronic irritation to the digital sensory nerve between the metatarsals. A neuroma frequently occurs in the third interspace but may be found in the second space (Fig. 51-4A). Patients report the sensation of a lump or cord in the interspace and describe paresthesia or numbness in the third or fourth toes. Direct compression plus release of the forefoot causes pain and often a “click” (the Mulder sign) (see Fig. 51-4B). Rest, elevation, ice, and NSAIDs may result in some improvement, but surgical excision is often required.16,17 Few data support the use of corticosteroid injections. In one study, less than 50% of patients with a foot neuroma had any benefit from injected corticosteroids.16 Another study demonstrated complete or partial relief in 80% of patients injected with corticosteroids.18 Although this study demonstrated a trend toward improved outcome when injected corticosteroids were compared with footwear modifications, corticosteroid injection therapy alone was not statistically better than footwear modification at 1 year.18 A ganglion cyst is histologically similar to the synovial sheath and contains synovial fluid. The diagnosis is easy to make when the cyst is located over a tendon on the dorsum of the foot (Fig. 51-5) but may be difficult when located among the compact structures of the plantar forefoot. A ganglion cyst usually causes edema along the involved tendon sheath. The mass should roll under the examiner’s finger; a painless, immovable mass suggests a soft tissue neoplasm. Painful ganglion cysts are treated by aspiration with or without injection of a corticosteroid (see Chapter 52). After local or regional anesthesia (see Chapters 29 and 31), insert a 20-gauge needle into the cyst and withdraw yellow, thick, synovial fluid. Manually express any remaining synovial fluid after the needle is withdrawn. Corticosteroid injection is often advocated for ganglion cysts, but recurrence is common after aspiration and corticosteroid injection—as high as 57% in one study.19 Recurrence, chronic pain, neuritis, stiffness, and infection are not uncommon even after surgical excision in many studies.20 Other authors report improved functional outcome, a 9% occurrence of paresthesia, and only a 5.7% recurrence rate after excision.21 Emergency clinicians often treat toe fractures and can intervene to relieve the pain and encourage healing. As with any other fracture, pay attention to the possibility of disrupted joint cartilage, hypermobility of the fracture segments, and malposition or malunion of the fracture fragments. Fracture displacement greater than 2 mm is uncommon; reduction is rarely needed for most toe fractures.22 However, aggressive reduction is indicated for fractures of the proximal phalanx of the great toe because it represents the main propulsive segment of the forefoot (Fig. 51-6). A plaster cast alone without anatomic reduction is insufficient treatment. Displacement suggests axial rotation or abnormal biomechanical interaction between the hallux and its own interphalangeal or MTP joint. Treat closed, lesser phalangeal fractures with “immobilization” for 6 weeks. After the fracture is reduced, splint the injured toe against an adjacent noninjured toe. Place a soft corn pad or other suitable material between the toes to prevent skin maceration, and hold the toes together with adhesive tape or a self-adherent wrap such as Coban (Fig. 51-7). Demonstrate the procedure to the patient or family and dispense or prescribe enough material so that the splint can be changed every 2 to 3 days at home. Have the patient wear a less restrictive, stiff-soled shoe (Fig. 51-8). A postoperative shoe (or similar footwear) may be a comfortable alternative for the first several days. Jumping from a height can result in a fracture of the first MTP joint sesamoid bone (Fig. 51-9A). The great toe sesamoid bones lie in grooves on the bottom of the metatarsal head. Each bone lies within the tendon of its respective flexor hallucis brevis muscle belly. Localized pain on the plantar aspect of the first metatarsal head accompanies a sesamoid bone fracture. Bipartite sesamoids (tibial more frequently than fibular) are common. Comparison radiographs clarify whether the radiographic abnormality represents a fracture.
Podiatric Procedures
Common Nontraumatic Conditions of the Foot
Footpad Use
Heel Pain Syndromes
Retrocalcaneal Bursitis, Achilles Tendinopathy, and Calcaneal Apophysitis
Painful Conditions of the Plantar Surface of the Foot
Forefoot Neuroma
Ganglion Cyst of the Foot
Traumatic Conditions of the Foot
Toe Fractures and Fractures of the Sesamoid Bones
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Podiatric Procedures