Chapter 11 Pericardial Disorders and Cardiac Tumors
PERICARDIAL EFFUSIONS
Physical Examination Findings
• Dogs with pericardial effusions present with clinical signs ranging from subtle to hemodynamic collapse (severe clinical tamponade).
Diagnostic Procedures
Electrocardiography
• Low voltage QRS complexes (R waves < 1 mV in all limb leads) are present in approximately half of the cases (Figure 11-2, A, B).
• Electrical alternans, a beat-to-beat variation in the contour and amplitude of the QRS and ST-T complexes (Figure 11-2, C), is strongly suggestive of a pericardial effusion. Electrical alternans is present in up to approximately 20% of dogs with pericardial effusions.
Echocardiography
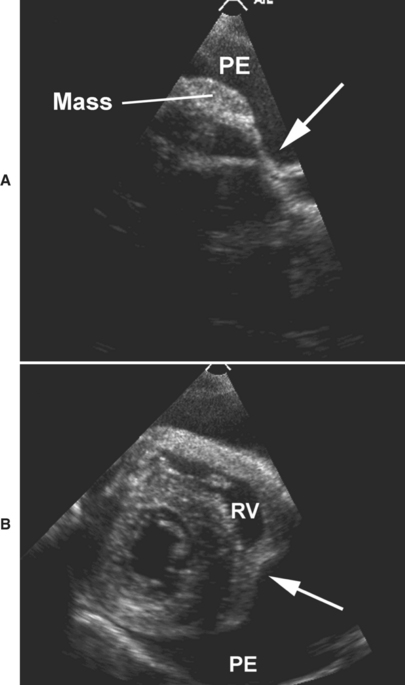
• The right atrial free wall is normally rounded throughout the cardiac cycle, reflecting the normal positive right atrial transmural pressure. Any inversion or collapse of the right atrial free wall provides indirect evidence of elevated intrapericardial pressure and transient reversal of transmural pressure (echocardiographic evidence of cardiac tamponade). Right atrial inversion occurs in late diastole and continues into ventricular systole for a variable period before normalizing (Figure 11-3, A).
• Cardiac tamponade leading to right ventricular diastolic collapse is characterized by inward motion of the right ventricular free wall (Figure 11-3, B). This may range from transient and localized concavity of the right ventricular free wall, to virtual complete right ventricular chamber obliteration throughout diastole.
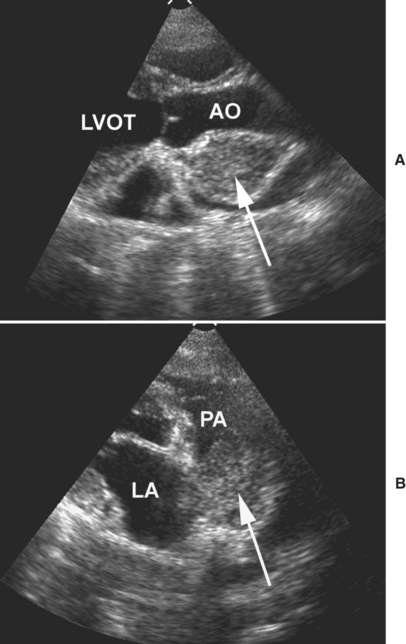
• In addition to confirming the presence of pericardial effusion and cardiac tamponade, echocardiography is the noninvasive procedure of choice to detect associated intrapericardial masses such as hemangiosarcoma and heart base tumors. Whereas histopathology is necessary to confirm and definitively identify a tumor, the echocardiographic location and characteristics of an intrapericardial or myocardial mass provides important information about the probable tumor type.
• The following echocardiographic features are consistent with a diagnosis of hemangiosarcoma:
• Hemangiosarcoma most commonly arises from the wall of the right atrium or auricle, protrudes into the pericardial space, and moves with the right auricle or atrium (Figure 11-4).
• These tumors may also protrude into the right atrial chamber, spread to involve other areas of the heart base and pericardium, and involve the right atrioventricular groove (see Figure 11-3, A).
• Hemangiosarcoma typically contains small hypoechoic spaces, giving the tumor a mottled or cavitary appearance, and the tumors are occasionally cystic (see Figure 11-4).
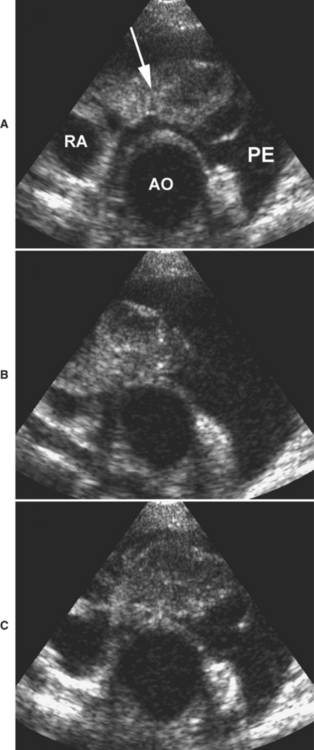
Figure 11-4 Echocardiographic images from a dog with cardiac hemangiosarcoma recorded in the short-axis view from the right parasternal location. A, A cavitary and cystic mass (arrow) is associated with the right auricle (RA). B and C, The mass moves back and forth with right auricular motion during different phases of the cardiac cycle. AO, Aorta; PE, pericardial effusion.
Initial Patient Stabilization: Pericardiocentesis
• Pericardiocentesis to remove as much pericardial fluid as possible is necessary for initial patient stabilization in any case with a pericardial effusion that is causing significant hemodynamic compromise (clinical cardiac tamponade).
• A small skin incision is made (Figure 11-6, A) and the catheter system is advanced towards the pericardium (Figure 11-6, B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree