Sophy A. Jesty
Pericardial Disease
Pericarditis is an uncommon but not rare condition in the horse. Early recognition of the disease is necessary for optimal outcome. Horses with cardiac tamponade secondary to pericarditis represent a true medical emergency. In this chapter, the causes, clinical signs, diagnosis, treatment, and prognosis for horses with pericarditis are reviewed.
In horses, pericarditis has been associated with viral and bacterial infections (equine herpesvirus type 1 [EHV-1], equine herpesvirus type 2 [EHV-2], influenza virus, Streptococcus spp, Actinobacillus equuli, Pseudomonas spp, Pasteurella multocida, Staphylococcus aureus, Acinetobacter spp, Escherichia coli, Enterococcus faecalis, Corynebacterium pyogenes, Mycoplasma felis, Propionibacterium acnes, Corynebacterium pseudotuberculosis, and Clostridium spp), immune-mediated disease such as eosinophilic pericarditis, neoplasia, trauma, and contiguous spread of an inflammatory process from adjacent or nearby tissues. Many cases of pericarditis in horses, however, are considered idiopathic.
Three outbreaks of pericarditis have been reported. The most thoroughly investigated occurred in the spring of 2001 (and to a lesser extent in 2002) in association with mare reproductive loss syndrome (MRLS) in Kentucky and surrounding areas. Other manifestations of MRLS included early and late fetal losses, endophthalmitis, weak late-term foals, and Actinobacillus spp–associated encephalitis. Approximately 60 horses developed pericarditis. In all cases, echocardiography revealed fibrin adherent to the pericardium and a variable volume of fluid in the pericardial space, and many horses also had concurrent pneumonia. Repeated pericardiocentesis was necessary in virtually all affected horses; pericardial lavage was performed in fewer cases.
In about two-thirds of these cases, fluid was characterized as an aseptic fibrinous effusion, whereas sepsis was the etiology in one-third of cases. Bacteria isolated from the septic effusions by use of standard culture techniques included A equuli, Streptococcus spp, P multocida, S aureus, Acinetobacter, and Pseudomonas spp. Actinobacillus equuli was the most common isolate and may be pericardiotropic in horses; Streptococcus spp were the second most common. Use of insect cell culture growth medium to culture fastidious bacteria from stored frozen pericardial samples yielded growth of P acnes, Staphylococcus equorum, Streptococcus spp, and Pseudomonas rhodesiae. The variety of bacterial isolates obtained makes it likely that bacterial infection of the pericardial space was opportunistic and developed secondary to a separate predisposing factor. Horses with aseptic pericarditis and those with septic fibrinous pericarditis all had negative results of testing for equine viral arteritis; EHV-1, -2, and -4; equine influenza virus; Mycoplasma spp, and Histoplasma spp. Bacterial isolates from horses that died included A equuli, Streptococcus zooepidemicus, and E faecalis. Viruses and mycoplasma were not isolated. Polymerase chain reaction assay of pericardial fluid yielded positive results for EHV-2, which is ubiquitous among horses.
The clinical manifestations of MRLS were associated with a point-source exposure to eastern tent caterpillars, and it has been hypothesized that gastrointestinal damage from caterpillar setae led to embolization of normal gastrointestinal tract flora that are delivered to the fetal fluids, pericardium, and aqueous humor. In support of the hypothesis, microgranulomatous lesions were observed around the setae embedded in the submucosal lining of the gastrointestinal tract of affected horses. Interestingly, the Actinobacillus strains isolated from pericardial fluid are the same as those found in the gastrointestinal tract of healthy horses.
Clinical Signs
The rapidity of onset of clinical signs of pericarditis varies considerably, ranging from acute pericardial fluid accumulation to slower, more chronic fluid accumulation, with or without pericardial fibrosis. Clinical signs are seen when diastolic cardiac filling is impaired, leading to systemic venous congestion and decreased cardiac output. This can develop as intrapericardial pressure increases with pericardial fluid accumulation (cardiac tamponade) or when fibrosis of the pericardium restricts normal distensibility. Development of increased pericardial pressure depends on the volume of pericardial fluid, rate of accumulation, and properties of the pericardium itself. Because the right side of the heart can withstand less transmural pressure than the left side before collapsing, signs of right-sided cardiac dysfunction develop first.
Common owner complaints at initial evaluation are often nonspecific and include fever, poor appetite, lethargy, weight loss, colic, and tachypnea. Signs of cardiac or respiratory tract disease are common reasons for referral of an affected horse from another veterinarian. Clinical signs appreciated in most horses with cardiac tamponade include tachycardia, jugular and other systemic venous distension, ventral edema, weak pulses, pale or cyanotic mucous membranes, and quiet heart sounds if the volume of pericardial fluid is substantial. Clinical signs detected in many horses with cardiac tamponade include pericardial friction rubs if the effusion is fibrinous, depression, fever, tachypnea or dyspnea, and quiet lung sounds ventrally. Pericardial friction rubs are classically triphasic in that they are heard during atrial contraction, during ventricular contraction, and after early diastolic filling.
Pulsus paradoxus may also be detected in horses with cardiac tamponade and is appreciated as an exaggeration of the normal decrease in systemic blood pressure that occurs during inspiration. This decrease is a result of decreased left ventricular stroke volume during inspiration because of increased venous return and right ventricular filling at the expense of left ventricular filling, a transient reduction in the filling gradient between the pulmonary veins and the left atrium, and a decrease in the contribution of the interventricular septum to left ventricular contraction. Peripheral pulses are sometimes too weak for pulsus paradoxus to be appreciated in horses with cardiac tamponade.
Diagnosis
A hemogram may reveal changes consistent with an infection or a stress leukogram, including leukocytosis, neutrophilia (with or without a left shift), and hyperfibrinogenemia. Results of a serum biochemistry panel may be normal or may indicate dehydration, hypoproteinemia, electrolyte derangements from pericardial accumulation of fluid (third-space fluid), or changes consistent with end-organ damage from cardiac tamponade, such as azotemia and high liver enzyme activities.
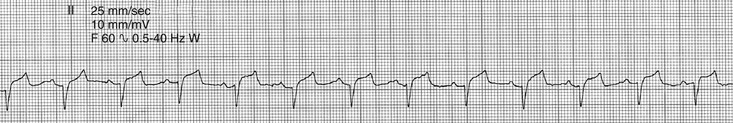
An electrocardiogram will likely reveal tachycardia and low-amplitude QRS complexes (Figure 123-1). Electrical alternans, or beat-to-beat alternation of R-wave amplitude, is a specific but not sensitive indication of cardiac tamponade. Radiography may reveal an enlarged cardiac silhouette, but cardiac margins may be difficult to assess if pleural effusion is present.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


