CHAPTER 25 Pediatric Fracture Management
Fracture Assessment Score
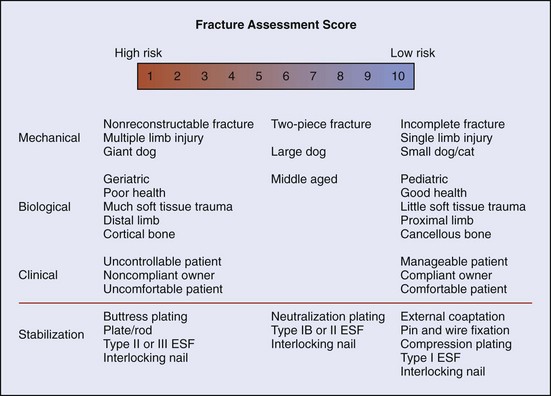
Fracture management has been described as a race between biologic healing of the fracture and mechanical failure of the stabilization used. The more mechanically or biologically favorable the fracture environment, the less robust or long lived need be the stabilization. The fracture assessment score is an objective method of considering all pertinent fracture characteristics to aid in fracture management decision making. It evaluates mechanical factors, biologic factors, and clinical (patient/client) factors and rates them on a scale of 1 to 10 (Box 25-1). Higher scores are given for factors that predict faster healing, minimal loads on implants, and decreased risk for implant failure. In general, pediatric patients tend to have higher scores for mechanical factors and biologic factors, predisposing them to more rapid healing. However, clinical factors may score lower than in adult patients. An overview of the scoring system is presented in Figure 25-1.
Physeal Fractures
Fractures of the physeal plate are not uncommon in young animals. The zone of hypertrophy in the physis is a focal weak point in the long bone. Ligaments and connective tissue are significantly stronger than the physis in pediatric patients. Thus trauma that would typically result in a sprain or luxation in adults can cause fracture or displacement involving the physis. Physeal fractures are categorized according to the method of Salter and Harris into types I through V, as described in Chapter 42 (see Figure 42-1), primarily in an attempt to prognosticate outcome.
Principles of Repair
Closed
Physeal fractures should be treated as early as possible after life-threatening injuries have been addressed. If treated early, some type I and II fractures of the tibia or distal radius can be reduced closed and treated with external coaptation (Figures 25-2 and 25-3). Treatment of humeral or femoral physeal fractures with external coaptation is not recommended (see following section on External Coaptation). If the fracture is significantly displaced or there is greater than 24- to 48-hour delay in treatment, closed reduction will be significantly more difficult or impossible, making open reduction and rigid fixation necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree