Chapter 15 Pathophysiology and Therapy of Heart Failure
HEART FAILURE
Pathophysiology
• Cardiac dysfunction that leads to the clinical syndrome of heart failure can be subdivided into systolic and diastolic dysfunction. Systolic dysfunction occurs when the ability of the heart to pump blood in a forward direction is impaired. Components of systolic function include myocardial contractility, valvular competence, preload, afterload, and heart rate.
Myocardial Failure
Diastolic Dysfunction
• Diastolic dysfunction may result in heart failure. Indeed, most cases of overt heart failure have some degree of diastolic dysfunction. Adequate ventricular filling is dependent on several factors:
COMPENSATORY MECHANISMS IN CHRONIC HEART FAILURE
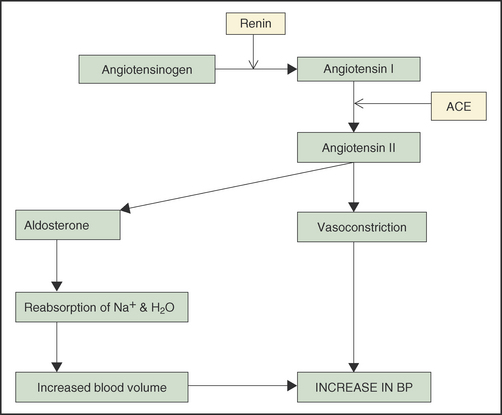
Renin-Angiotension-Aldosterone System
• The renin-angiotensin-aldosterone system (RAAS) is a complex neurohormonal compensatory system that functions to maintain relatively normal blood pressure and tissue perfusion when cardiac output is reduced. Reduced renal perfusion detected by renal baroreceptors results in release of renin (Figure 15-1). Other factors causing release of renin include decreased sodium delivery to the macula densa, and SNS stimulation of beta-1 adrenoceptors in the juxtaglomerular apparatus of the kidney. Renin initiates a cascade resulting in the formation of angiotensin II, a potent vasoconstrictor. Angiotensin II also causes activation of the SNS, increases synthesis and release of aldosterone from the zona glomerulosa of the adrenal cortex and release of antidiuretic hormone.
• Angiotensin II stimulates the release of growth factors that promote remodeling of the vessels and myocardium. Vascular remodeling (smooth muscle cell growth and hyperplasia, hypertrophy, and apoptosis; cytokine activation; myocyte and vascular wall fibrosis) results in decreased vascular responsiveness to alterations in blood flow, decreased vascular compliance, and increased afterload. Angiotensin II also causes pathologic ventricular hypertrophy, exerts cytotoxic effects resulting in myocardial necrosis and loss of myocardial contractile mass with resultant cardiac dysfunction.
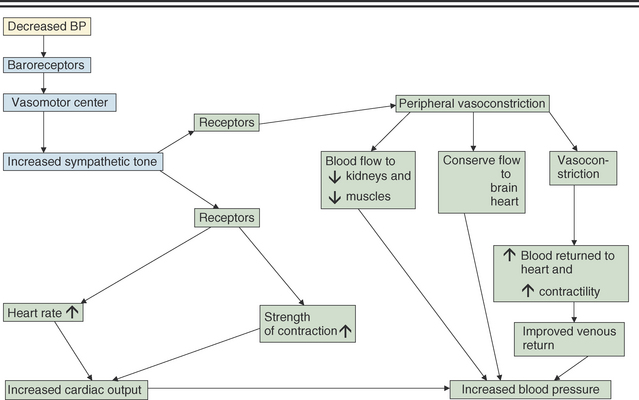
Sympathetic Nervous System Activation
Sympathetic Nervous System Activation
• The autonomic nervous system plays a crucial role in the compensation of heart failure. The activity of the SNS is increased in part by baroreflex-mediated parasympathetic withdrawal, as well as by activation by the RAAS. Early activation of the SNS helps to maintain cardiac output, blood pressure, and tissue perfusion by increasing venous return to the heart (vasoconstriction of the splanchnic vessels), vasoconstriction of other various vascular beds, and positive inotropic and chronotropic cardiac effects. Activation of the SNS early in heart failure is beneficial, but becomes maladaptive when chronically activated (Figure 15-2).
Sympathetic Desensitization:
• Chronic activation of the SNS also overloads the heart by increasing venous return (to a heart that is already volume-overloaded), by increasing myocardial oxygen consumption (by increasing heart rate and volume overloading of the heart) and by damaging the myocardium, creating a substrate for arrhythmogenesis.
Myocardial Hypertrophy
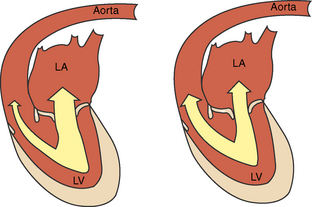
• Concentric myocardial hypertrophy (or pressure-overload hypertrophy) is characterized by thickening of the ventricular walls in response to increased systolic wall stress, and occurs as a compensatory mechanism to normalize systolic wall tension. Increased systolic wall stress stimulates the replication of sarcomeres in parallel, increasing myocardium thickness and thereby normalizing systolic wall stress (via the La Place relationship, wall tension = pressure × radius/wall thickness). The increase in thickness of the ventricular wall compensates for the increased systolic wall stress in a pressure-overloaded ventricle. If the compensatory concentric hypertrophy is inadequate and the systolic wall stress is increased, then afterload-mismatch and decompensation occur. Interestingly, when significant eccentric hypertrophy occurs in a volume-overloaded ventricle, systolic wall tension is increased secondary to the increase in ventricular diameter. Therefore, both eccentric and some degree of concentric hypertrophy are present in severely volume-overloaded ventricles.
TYPES OF HEART FAILURE
Myocardial Failure
Decreased Ventricular Compliance or Abnormal Ventricular Relaxation
CLINICAL DESCRIPTIONS OF HEART FAILURE
• Right-sided heart failure may result when the right atrium or right ventricle develops elevated filling pressures associated with valvular insufficiency, pericardial disease, outflow tract obstruction, or pulmonary hypertension. Volume and pressure overloading of the right ventricle can cause hepatic congestion accompanied by ascites, pleural effusion, and, rarely, peripheral subcutaneous edema. These diseases may also reduce the forward flow of blood into the pulmonary circulation and the left heart, resulting in reduced stroke volume, cardiac output and, possibly, signs of low-output heart failure.
DIAGNOSIS OF HEART FAILURE
History
• Coughing, tachypnea, dyspnea (respiratory distress), exercise intolerance, lethargy, and weakness are common complaints of clients with pets with symptomatic heart disease or heart failure. Additionally, pets with heart failure may have a history of inappetence, weight loss, and syncope.
• Nocturnal coughing or dyspnea typically occurs after the patient has been recumbent for some time. It is not specific for left-sided CHF.
Cardiovascular Physical Examination Findings
Murmur
Diagnostics
Electrocardiography
• Electrocardiography is used to detect cardiac rhythm disturbances, chamber enlargement, or conduction abnormalities that may be associated with cardiac disease. Electrocardiographic abnormalities are not specific for heart failure and therefore should not be used to determine the presence of heart failure. Furthermore, a normal electrocardiogram does not rule out the possibility of severe heart disease with secondary chamber enlargement.
Thoracic Radiography
• Thoracic radiography is important in the evaluation of patients with suspected heart disease or CHF. In general, with respect to heart disease and heart failure, three questions should be answered when evaluating a thoracic radiograph:




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree