CHAPTER 6 Parasitic Diseases
Dermatoses caused by ectoparasites are common skin disorders of large animals.5 They accounted for 7.7% of the equine dermatoses seen at Cornell University for Animals (CUHA). Already-diseased skin is more vulnerable to fly or mosquito parasitism and makes the diagnosis of the underlying disease more difficult. Animal suffering through annoyance, irritability, pruritus, disfigurement, secondary infections, and myiasis is often great. Many of the ectoparasites are important in the transmission of various viral, protozoal, helminthic, fungal, and bacterial diseases. The important arachnids, insects, and helminths associated with skin disease in horses are listed in Boxes 6-1-6-3.
Box 6-1 Arachnids Associated with Skin Disease in Horses
Therapeutics
The treatment of ectoparasitism is a complex topic.5 Significant differences exist in the regional availability of, and regulations governing, parasiticidal agents. In general, most agents used to treat or prevent parasitic skin disorders of the horse are registered pesticides rather than drugs. Pesticides are under the regulation of the Environmental Protection Agency (EPA) in the United States. Other countries have similar agencies. Because of the long-lasting consequences of some chemicals, many are not available today and some can only be applied by a registered pesticide applicator. Nonrestricted pesticides must be used in accordance with their labeled directions. It is a violation of federal law in the United States to use an EPA-registered pesticide in an extra-label fashion. Commonly accepted veterinary practice is not a legitimate excuse for extra-label use. Extra-label usage includes the treatment of a nonlabeled species, a higher frequency of application than the label allows, or usage for a disorder not listed under the indications. The reader should follow all pertinent regulations in his or her country.
Topical Treatments
Topical antiparasitic therapy is primarily directed against ectoparasites that feed or live on the horse.5 In treating the dermatosis, it is critical to consider the parasite; its life cycle, epidemiology, and natural behavior; and the pathogenesis of the disease the parasite is causing. Topical therapy may be just one aspect of an overall treatment plan, or it may be the sole therapy prescribed. Proper application becomes critical when it is the sole therapy.
Historical Equine Parasiticides
In the past, chlorinated hydrocarbons, organophosphates, and carbamates were the mainstay of treatment for external parasitic disorders of the horse.5 These agents were dangerous for the animal, the environment, and the applicator. For the most part, these agents are no longer available. At this writing, only one product, coumaphos, is licensed in the United States for use on the horse and must be applied by a certified applicator.
Formamidines
These acaricidal agents act by inhibition of monoamine oxidase. They are also prostaglandin synthesis inhibitors and α-adrenergic agonists. Amitraz is available as rinse, collar, and spot application products for control of ticks and Demodex mites in the dog. Amitraz is contraindicated in horses. Horses sprayed with a 0.025% solution developed somnolence, depression, ataxia, weakness, and colonic impaction.5
Systemic Antiparasitic Agents
Systemic endectocides
These parasiticides were developed from macrocyclic lactones produced by the fermentation of various actinomycetes. This class of drugs includes avermectins (ivermectin, doramectin, abamectin, selamectin, eprinomectin) and milbemycins (milbemycin, moxidectin). At present, the product used most in equine dermatology is ivermectin. Preliminary studies suggest that all of these products may have equal efficacy when administered at the appropriate dosage. All partly act by potentiating the release and effects of GABA. GABA is a peripheral neurotransmitter in susceptible nematodes, arachnids, and insects. Avermectins and milbemycins are also agonists of glutamate-gated chloride channels. In mammals, GABA is limited to the central nervous system. Because these drugs do not cross the blood-brain barrier in most adult animals, they are relatively safe and have a wide margin between efficacy and mammalian toxicity. If the horse has some preexisting defect in the blood-brain barrier, neurotoxicity can be seen at recommended doses.6 Their use in foals less than 4-months-old is contraindicated. In general, these drugs are effective for nematodes, microfilaria, lice, and mites.
Ivermectin
Ivermectin is rapidly absorbed orally (PO) and has a plasma resident time of up to 20 days.3,5 Intramuscular administration results in longer lasting plasma levels: 8.9 ± 0.7 days versus 4.2 ± 0.4 days.4 Ninety percent of the dosage is eliminated in the feces within 4 days. The dosage used to treat all nonfollicular mites is 0.2 mg/kg at 14-day intervals.
Moxidectin
Moxidectin (Quest, Fort Dodge) is derived from fermentation products of Streptomyces cyaneogriseus subsp. noncyanogenus. It is marketed for the treatment of various intestinal parasites, including pinworms and bots. It is administered at 0.4 mg/kg PO. Its plasma resident time is approximately 18 days.5 Since it is equally as effective in treating onchocerciasis as is ivermectin, the two products probably can be used interchangeably.
Doramectin
Doramectin (Dectomax, Pfizer) is derived from fermentation of selected strains of S. avermitilis. In the United States, it is marketed for the treatment and control of various nematodes, mites, and lice in cattle and swine. In horses, when given at 0.2 mg/kg PO, plasma levels are measurable for 30 days.3
Mites
Older parasitology texts list a varying number of species for each genus of mite. In separate studies on Psoroptes and Sarcoptes mites from different species located on different continents, Zahler found that “different” species within the same genus differ phenotypically but not genotypically.5 Since different species of Psoroptes mites (P. ovis and P. cuniculi) are known to interbreed, it is likely that all species of nonfollicular mites within a given genus are related and have limited host specificity.
Psoroptic Mange
Psoroptic mange is a pruritic dermatitis and/or otitis externa of horses.1,2,5
Cause and pathogenesis
Psoroptes spp. mites are large (0.4-0.8 mm long) (Fig. 6-1) and nonburrowing and feed on tissue fluids.5 Their life cycle on the host is completed in approximately 10 days. Median life expectancy of an adult female is about 16 days. Off-host survival time is significantly influenced by local temperature and humidity. Environmental conditions in the corners of stalls, organic debris, and bedding, etc. can be very different from those in the rest of the barn with a prolonged off-host survival time. High temperatures and low humidity disfavor survival. In the typical barn, a 14- to 21-day off-host survival can be expected.1,5,8 However, P. ovis and P. cuniculi maintained under various environmental conditions survived for up to 48 and 84 days, respectively.5 The researchers suggested stable quarantine periods of 7 and 12 weeks, respectively.
Clinical features
Transmission of Psoroptes mites is by direct or indirect contact. In herds, up to 10% of contact animals may be infected.7 The incubation period varies from 2 to 8 weeks. If the horse has been infested previously and became hypersensitive during the initial exposure, the incubation period will be shorter.
Clinical signs are quite variable.5 Infested horses may be asymptomatic or may show signs of ear disease, truncal dermatitis, mane and tail disease, or combinations of these. Signs of ear disease include head shaking, ear scratching, or head shyness, and the horse may have a lop-eared appearance (Fig. 6-2). The dermatitis tends to be focused around the ears, mane (Fig. 6-3), and tail (Fig. 6-4). Pruritus is variable but can be intense. In mildly pruritic horses, the presentation will be of mane and tail seborrhea (see Chapter 11). In more pruritic horses, one sees nonfollicular papules, crusts, excoriation, and alopecia. In severe cases the entire topline may be involved.

Figure 6-2 Psoroptic mange. Lop-eared head carriage due to parasitic otitis externa.
(Courtesy W. McMullen.)
Diagnosis
The differential diagnosis includes sarcoptic mange, chorioptic mange, lice, insect-bite hypersensitivity, fly-bite dermatitis, atopic dermatitis, and food allergy. Definitive diagnosis is based on history, physical examination, skin scrapings, and otoscopic examination. Body mites, depending on the degree of infestation, may or may not be demonstrated in skin scrapings. Ear mites can be very difficult to demonstrate even with a thorough otoscopic examination (usually requires chemical restraint) and microscopic examination of material gathered from deep within the ear canal. Skin biopsy reveals varying degrees of superficial perivascular-to-interstitial dermatitis with numerous eosinophils.5 Eosinophilic microabscesses and focal areas of epidermal edema, leukocytic exocytosis, and necrosis (epidermal “nibbles”) may be found. Mites are rarely seen.
Clinical management
There are various reports on the treatment of Psoroptes otoacariasis with numerous topical parasiticides.5 After a thorough ear cleaning, the product is applied twice weekly for 3 weeks. If the horse is extremely head shy, owner compliance will be a problem and relapses can be expected. Since mites can survive outside the ear canal, simultaneous treatment of the body is recommended to prevent a relapse. Pyrethrin, pyrethroid, or lime sulfur sprays or dips can be effective when applied every 7-14 days for 3-4 weeks. Amitraz is contraindicated in horses.
Ivermectin (0.2 mg/kg PO) or moxidectin (0.4 mg/kg PO) are very effective in the treatment of psoroptic otoacariasis and/or dermatitis.5,9 A single dosage rapidly decreases mite and egg counts with parasitologic cure within 30 days of treatment. To ensure a cure, a second dose 14 days after the initial treatment is recommended. The cattle product, eprinomectin, can be applied as a pour-on at a dosage of 0.5 mg/kg once weekly for 4 treatments.8 Since ivermectin and other parasiticides do not kill eggs, the treated horse should be considered infectious for the first few weeks of treatment.
Sarcoptic Mange
Sarcoptic mange is a rare cause of pruritic dermatitis in horses.1,2,5
Cause and pathogenesis
Sarcoptes spp. mites (0.25-0.6 mm in diameter) (Fig. 6-5) tunnel through the epidermis and feed on tissue fluids and possibly epidermal cells. The life cycle on the host is completed in 2-3 weeks. The mites are quite susceptible to drying and survive only a few days off the host. Transmission is by direct and indirect contact. The incubation period varies from a few hours to several weeks, depending on the method and severity of exposure and on prior sensitization of the host.
Sarcoptes scabiei mites are found on a number of different hosts. It is currently believed that all the various mites are genotypically identical.5 Through adaptations for survival on a particular host, the mites may be phenotypically different, but these phenotypic differences do not confer strict species specificity. Cross-infestation among animals and between animals and humans are common.
Clinical features
Once common, equine sarcoptic mange is now rare throughout the world.5 In the United States, equine sarcoptic mange has been eradicated. There are no apparent age, breed, or sex predilections. The chief clinical sign is pruritus, which usually begins on the head, ears, and neck (Fig. 6-6), and spreads caudally. Nonfollicular papules, crusts, excoriations, alopecia, and lichenification are usually seen. If the mite is acquired from a fox during a hunt, the horse can develop a distal limb dermatitis mimicking many other conditions.1
Diagnosis
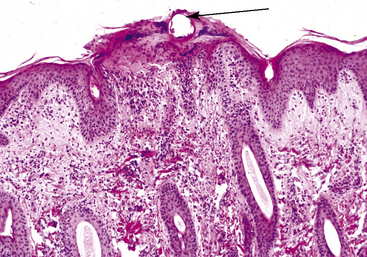
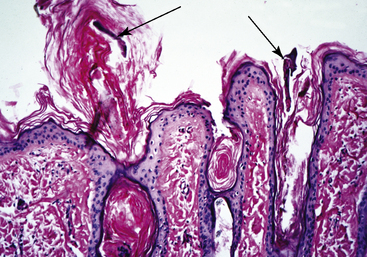
Skin biopsy reveals varying degrees of superficial perivascular-to-interstitial dermatitis with numerous eosinophils.5 Eosinophilic microabscesses and focal areas of epidermal edema, leukocytic exocytosis, and necrosis (epidermal nibbles) may be seen. Mites may be seen within parakeratotic scale-crusts and in subcorneal “tunnels,” but this is uncommon. Occasionally, deep perivascular dermatitis with lymphoid nodules may be seen.
Chorioptic Mange
Chorioptic mange (leg mange, tail mange, symbiotic scab, foot mange) is a common cause of dermatitis in horses.1,2,5
Cause and pathogenesis
Chorioptic mites (0.3-0.5 mm long) (Fig. 6-7) are surface-inhabiting parasites that feed on epidermal debris.5 The life cycle takes about 3 weeks and is completed on the host. Adult mites can survive off-host for nearly 70 days, depending on the presence of epidermal debris as a food source and the local environmental conditions. Transmission is by direct and indirect contact.
Mite populations are usually much larger during cold weather.5 Thus, clinical signs are usually seen, or are more severe, in winter. This seasonality of mite populations and clinical signs is thought to be influenced by temperature, humidity, and wetting of the host. Hot and dry conditions decrease mite survival times. The signs of disease often spontaneously regress during summer when mite numbers become very small. During this clinically inapparent stage of infestation, mites may only be demonstrated around the coronet.
Clinical features
Chorioptic mange occurs in horses in most parts of the world.* In general, there are no apparent age, breed, or sex predilections.
Chorioptes spp. infestations are most commonly seen in draft horses and other horses with feathered fetlocks, especially during winter. Clinical signs are seen on the distal hand limbs (Fig. 6-8) with the fetlocks, pasterns (Fig. 6-9), and tail being particularly affected. Pruritus may be intense or absent. Horses with widespread lesions have been seen (Fig. 6-10).
Diagnosis
The differential diagnosis includes tail rubbing (insect-bite hypersensitivity, food allergy, atopic dermatitis, lice, oxyuriasis, or stable vice) and pastern dermatitis (see Chapter 15). Definitive diagnosis is based on history, physical examination, and examination of skin samplings collected by scraping, brushing, or combing. In feathered horses, combings and brushings are more likely to be positive.11 During cool weather, Chorioptes spp. mites are usually easy to demonstrate. These mites are usually active and fast-moving. To prevent them from walking off the slide, the authors recommend using an insecticide-containing solution for the skin-scraping solution. Skin biopsy reveals variable degrees of superficial perivascular-to-interstitial dermatitis with numerous eosinophils.5 Eosinophilic epidermal microabscesses and focal epidermal necrosis, leukocytic exocytosis, and edema (epidermal nibbles) may be seen (Fig. 6-11). Mites are not usually seen.
Clinical management
Because of the mites’ feeding habits, treatment with conventional systemic endectocide regimens may or may not be effective.* Treatment with higher dosages of ivermectin (0.3 mg/kg) at higher frequencies (weekly for four treatments) can improve the response rate, but therapeutic failures will occur.
Topical treatments are labor-intensive but effective. To allow better access of agent to the mites, feathers should be clipped from draft horses. The most labor-intensive treatment involves bathing the horse with a 2% selenium sulfide shampoo.5 The shampoo is prediluted with water (1:2), and the horse is bathed three times at 5-day intervals. After a 10-min contact time, the lather is rinsed off and the horse is allowed to dry.
Over the years, various topical insecticides, applied at 7- to 14-day intervals, have proven to be effective. Effective agents include 0.25% crotoxyphos, 0.5% malathion, 0.5% methoxychlor, 0.06% coumaphos, and 2% lime sulfur.5 A 0.25% fipronil spray has been reported to be curative in one treatment.5 Horses are sprayed from the elbows and stifles down with 125 mL of product applied to each leg. To ensure cure, a second treatment in 3-4 weeks is recommended.5,12 This application constitutes an extra-label use of an EPA-registered pesticide. A 5% lime sulfur solution applied at 7-day intervals can be effective even when other treatments fail.5,10
Demodectic Mange
Demodectic mange (follicular mange, demodicosis) is a follicular dermatosis rarely seen in horses.5
Cause and pathogenesis
Demodectic mites are normal residents of the skin in all large animals.5 The mites live in hair follicles and sebaceous glands, are host-specific, and complete their entire life cycle on the host. The life cycle of most demodicids has not been carefully studied, but is assumed to be completed in 20-35 days.
Under most environmental conditions, demodicids can survive only several minutes to a few days off the host. Studies in cattle and dogs have shown that: (1) demodectic mites are acquired during the first 2-3 days of life by direct contact with the dam, (2) animals delivered by cesarean section and raised away from other animals did not harbor demodectic mites, and (3) confining normal adult animals with severely infested and diseased animals for several months did not produce disease in the normal animals.5
In addition, attempts to transmit clinical demodicosis to horses by direct contact and by applying mites to the skin were unsuccessful.5 Thus, demodectic mange is not thought to be a contagious disease.
Because demodectic mites are normal residents of the skin, it is likely that animals manifesting clinical disease resulting from this parasite are, in some manner, immunocompromised. Demodicosis in dogs is known to occur due to immunosuppression (drugs or diseases) and genetic predilection (selective immunodeficiency?).5 In large animals, many authors have suggested that clinical demodicosis probably occurs only in animals that are immunocompromised (debilitation, concurrent disease, poor nutrition, or stress). In horses, demodicosis has been reported in association with chronic treatment with systemic glucocorticoids or pituitary pars intermedia dysfunction.1,5
Clinical features
Equine demodectic mange is recognized worldwide but is very rare in occurrence and has no apparent age, breed, or sex predilections.5 The authors have rarely seen equine demodicosis and only in association with long-term glucocorticoid administration. Horses possess two species of demodicid mites: Demodex caballi (264-453 μm in length; eyelids and muzzle) and D. equi (179-236 μm in length; body) (Fig. 6-12). Clinical signs consist of usually asymptomatic hypotrichosis, alopecia, scaling, and occasionally crusting, especially over the face (Fig. 6-13), neck, shoulders (Fig. 6-14), and forelimbs. Papules and pustules may be seen.
Diagnosis
The skin biopsy reveals hair follicles distended to varying degrees with demodectic mites and keratin.5 In many cases, there is minimal inflammatory response (Fig. 6-15). Alternatively, varying degrees of perifolliculitis, folliculitis, furunculosis, and foreign body granuloma formation may be seen.
Trombiculiasis
Trombiculiasis (trombidiosis, chiggers, harvest mite, scrub itch mite, leg itch, heel bug) is a common dermatosis of horses in many parts of the world.5
Cause and pathogenesis
Trombiculid adults and nymphs are free-living and feed on invertebrate hosts or plants.5 Eggs are laid in the soil and hatch to larvae in approximately 1 week. The larvae normally feed on tissue fluids of small rodents, but are not host-specific and will attack horses and humans. Skin lesions produced by feeding larvae consist of papules and wheals. Because some animals manifest extreme pruritus, and other animals none, it is theorized that the pruritic animals may have developed a hypersensitivity reaction to larval salivary antigen(s).
Trombiculid larvae measure 0.2-0.4 mm in length and vary in color from red-to-orange-to-yellow. In North and South America, Trombicula (Eutrombicula) alfreddugesi (Fig. 6-16) and T. splendens are important trombiculids that inhabit forested and swampy areas. T. (Neotrombicula) autumnalis—the harvest mite, or heel bug, of Europe and Australia—inhabits chalky soils, grasslands, and cornfields. T. sarcina is the blacksoil itch, or leg itch, mite of Australia.

Figure 6-16 Trombicula (Eutrombicula) alfreddugesi (×100). Six-legged larva collect in a skin scraping.
Clinical features
Trombiculiasis generally occurs in the late summer and fall, when larvae are active.5 The infestation is seen primarily in pastured animals, horses in infested paddocks, or horses taken on trail rides through infested fields and woods. The larva may persist in hay or straw bailed in late summer and infest stalled horses that encounter it.13 There are no apparent age, breed, or sex predilections.
Skin lesions consist of papules and wheals at the site of larval attachment. Typical sites include the muzzle, nares, false nostril, face, ears, neck, and distal limbs (Fig. 6-17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree