CHAPTER 3 Dermatologic Therapy
Basic nutrition and the skin
Fats are an important part of the diet and are valuable as a concentrated energy source. If there is too little total fat or linoleic acid, a dry scaly skin or poor hair coat could be the result. Fatty acids have been recommended for many years as dietary supplements to improve the sheen and luster of the hair. Fatty acids as therapeutic agents are discussed in Chapter 8.
Fatty acids are valuable components of cell membranes but also have an extracellular function in the skin. They are responsible for the luster of the normal hair coat and the smoothness of the skin. Linoleic acid is particularly important because only it supplies the proper conditions for the water permeability functions of the intercellular lipid bilayer of the skin (see Chapter 1).
Topical therapy
Topical therapy has always played a large role in dermatology because of the obvious access to the affected tissue.4,17,44 Topical applications continue to be popular and useful in treating equine skin disease. Growth in topical therapy reflects multiple factors, which may include: (1) the development of more products, better delivery systems, and active ingredients; (2) the reduction in systemic absorption or effects and adverse reactions; and (3) the recognition of the adjunctive and synergistic effects in the overall management of numerous skin diseases. These factors are also the advantages that topical therapy offers to the clinician and the horse owner.
Topical products commonly used for the treatment of equine dermatoses have received little or no scientific investigation. Hence, many treatment protocols are based on anecdotal reports or have been extrapolated from other species. Companion animal products are frequently used on horses and are safe and effective.30,44
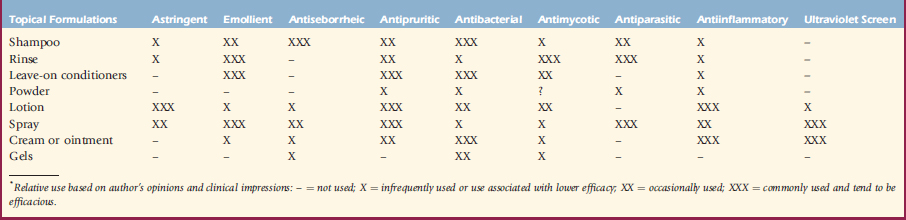
When a clinician elects to use topical therapy, several factors must be considered. Primarily is, what is the purpose or desired result of the topical therapy? Is this the sole therapy, or is it adjunctive to other nontopical therapies? What type of delivery system best facilitates obtaining the desired result? What active ingredients are used for this purpose? As previously discussed, patient and client considerations are paramount. Table 3-1 lists the most common delivery systems and formulations of active ingredients used in veterinary dermatology. The amount of use for each type of product relative to the others is based solely on the authors’ opinions and clinical impressions.
Factors That Influence Drug Effects on the Skin
Clinical efficacy and absorption are not synonymous; absorption is only one factor in efficacy. Some drugs in an insoluble form in the vehicle have only a surface effect. Once absorbed, a drug must also interact with specific receptors before an action will result. The drug’s affinity for the receptors and local factors that affect this drug-receptor interaction are also important. Absorption of drugs through the skin involves many variables. There are physicochemical factors related to the topical formulation and biologic factors. The physicochemical factors involve the interactions between the drug and the vehicle, the drug and the skin, and the vehicle and the skin. Some of these factors are determined by the concentration of the drug, the drug’s movement between the vehicle and the skin, the diffusion coefficient, and the local pH.17,26,44
Biologic factors also affect drug absorption. The body region treated may influence absorption. In horses, topical hydrocortisone penetrates faster through lower leg skin than through skin of the thorax or groin.27 Age is an important factor, with newborns experiencing greater absorption than adolescents do, who in turn experience greater absorption than adults do. Obviously, the health and condition of the skin is important because inflamed, abraded, or otherwise damaged skin often absorbs more drug. Blood flow also affects absorption. Greater blood flow favors increased systemic absorption.
Hydrotherapy
Cold applications cause capillary constriction and decreased blood flow.53 They are often used to retard swelling, prevent hematoma formation, and allay pain and itch. Warm applications cause vasodilation, increased blood flow, increased tissue oxygenation, and increased lymph flow.53
Topical Formulations
Shampoos
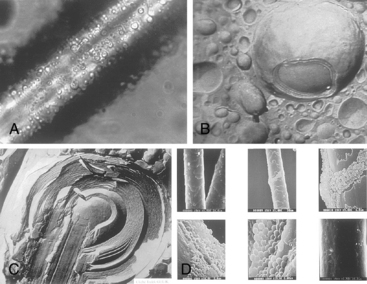
Shampoo formulations have been developed that use sustained-release microvesicle technology. In one type, the microvesicles have an outer lipid membrane and contain water (Novasomes, Vétoquinol).8,44 The lipid membrane binds to hair and skin and has a long-term moisturizing effect as the microvesicles break down (Fig. 3-1A and B). This counteracts the drying that may occur with some medications and is therapeutic for dry skin. However, the active medication is not incorporated and will still be rinsed away.
The second microvesicle technology (Spherulites, Virbac)8,44 actually incorporates different ingredients, such as salicylic acid and sulfur, chlorhexidine, ethyl lactate, benzalkonium chloride, oatmeal extract, glycerin, and urea, into multiple layers of these microvesicles. Also, these microvesicles have multiple (10-1000) layers that slowly break down (Fig. 3-1C). With the breakdown of each layer, the active ingredients and the surfactants that make up these layers are released onto the hair and skin. The microvesicles can be made with different charges on the exterior; making them positively charged causes them to bind with the negatively charged hair and skin (Fig. 3-1D). Chitosanide has been used to make the microvesicles called spherulites. Besides supplying the outer cationic surface, chitosanide is an active moisturizing agent and is hygroscopic.
Certain principles should be kept in mind when using medicated shampoos:
Medicated shampoos are often classified because of their primary activity or function.