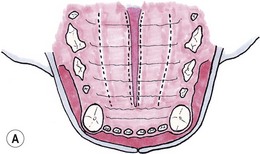
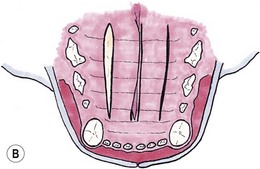
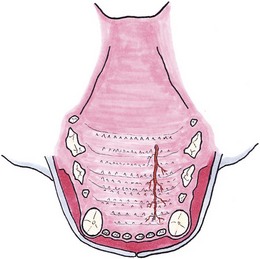
Chapter 56 The secondary palate is a bony and soft tissue structure that separates the respiratory and digestive passages of the head.1 The primary palate consists of the lips and premaxilla,2 and conditions affecting these areas are covered in Chapters 49 and 55. The nasal cavity and nasopharynx lie dorsal to the secondary palate, while the oral cavity and oropharynx lie ventral to it. The bony hard palate lies rostrally and the membranous soft palate caudally.1 The hard palate is formed by fusion of the palatine, maxillary, and incisive bones on each side.3 The soft palate extends caudally from the hard palate and this tends to be relatively short in the cat. There is a thin fold from its ventrolateral part that extends on each side to form the ventral wall of the tonsillar crypts.1 The palate has mucosa both on the nasal and oral sides. The mucosa on the oral side of the hard palate is a tough, cornified squamous epithelium. While there are no muscles of the hard palate, the muscles of the soft palate consist of paired (intrinsic) palatine muscles, and paired (extrinsic) tensor and levator veli palatine muscles. There are many palatine glands that lie within the bulk of the soft palate, which have many openings throughout the surface of the soft palate.1 The maxillary artery is the main continuation of the external carotid artery. It supplies a branch to the mandible before extending rostrally to where it branches to become the minor palatine artery, major palatine artery and infraorbital artery.3 The minor palatine arteries are the main blood supply to the soft palate, and the major palatine artery is the main blood supply to the hard palate.1 The major palatine foramen is located medial to the fourth premolar tooth and there are one or more minor palatine foraminae located caudal to this.3 The major palatine artery exits the skull through the major palatine foramen and courses rostrally along the ventral surface of the bony hard palate (Fig. 56-1). It supplies bone and soft tissues of the hard palate before reaching the midline palatine fissure where it anastomoses with the infraorbital artery.3 The minor palatine artery(ies) exit the skull through the minor palatine foramen(ae) to supply the soft palate, with contributions from the ascending pharyngeal artery and major palatine artery.3 The arteries are dwarfed by the palatine plexus of veins, which mainly lie lateral to the paired slender palatine muscles.1 Venous drainage of the hard palate is located in the submucosa covering the bony palate. Lymphatic drainage is usually via the medial retropharyngeal lymph nodes.1 Figure 56-1 The major palatine artery exits the skull through the major palatine foramen and then courses rostrally. It is the main blood supply to the hard palate. The trigeminal nerve supplies the main sensory nerves to the palate. The major palatine branch of the maxillary division of the trigeminal nerve enters the palate through the major palatine foramen to supply sensory function to the hard palate, and the minor palatine branch enters through the minor palatine foramen to supply sensory function to the soft palate.1,3 Branches of the glossopharyngeal and vagus nerves supply the muscles of the soft palate and pharynx.1 Diagnosis of congenital defects of the palate or oronasal fistulae is very easy and involves a simple physical examination. A sedation or general anesthetic may be required in animals that are difficult to examine. Animals may present with clinical signs of poor growth, nasal discharge, sneezing while eating, dyspnea, upper respiratory congestion, coughing, sneezing, or halitosis.4,5 Middle ear disease associated with congenital palatine defects has been reported in a cat.6 Neoplasia of the palate will often go unnoticed until a mass is interfering with deglutition, respiration, causes weight loss, local irritation, cessation of grooming, or ulcerates causing bleeding and/or halitosis due to superficial infection.7 Palatal masses are often not painful.7,8 Masses may be identified during routine dental procedures. Examination of the hard palate should be routine in any physical examination for amenable patients. The majority of the hard and soft palate can be examined visually under a general anesthetic with the aid of a laryngoscope or other good light source. A more complete examination of the nasopharynx may be performed using a small flexible fiberoptic endoscope. Any masses seen should have a biopsy performed for histologic examination, and associated local lymph nodes should be aspirated to check for spread of disease. If histology is consistent with a malignancy, a computed tomographic scan (CT) is often worthwhile during the staging process to aid in identifying the extent of locoregional disease and thereby assisting in determining treatment options. If previous thoracic radiographs are clear for evidence of metastases, CT may aid in earlier detection of pulmonary metastases or local or thoracic lymphadenopathy. Staging tests performed will depend on the histologic diagnosis and expected biological behaviour of the mass, and will usually include a complete blood count, biochemical panel, and urinalysis. Other tests to consider may include abdominal ultrasonography, coagulation panel, other blood tests, or nuclear scintigraphy for primary bone tumors. For a detailed discussion of oral neoplasia readers are referred to Chapters 49 and 55. Timing of surgery needs to be considered for correction of congenital clefts of the palate. While early surgery may cause interference with normal growth of the skull,9,10 surgery is often performed before skeletal maturity without subsequent clinically apparent problems.4 Animals may live with congenital defects of the palate for months prior to performing a surgical correction. Surgery should be performed sooner for animals that are not eating well or if their quality of life is otherwise significantly affected.4 If early repair is performed, the reconstructed palate of a neonate grows rapidly, causing stretching and thinning of some repairs. This can result in oronasal fistulae, which can then be repaired after patients reach eight to ten months old.2 Preoperative thoracic radiographs are performed since aspiration pneumonia is a possible complication of congenital palatine defects.6 Otoscopic examination should be performed and skull radiographs considered, even in asymptomatic animals, due to the association of middle ear disease with congenital palatine defects.6 Defects in the hard and soft palates may be congenital or acquired. Congenital defects may include clefts of the hard and/or soft palate, and hypoplasia of the soft palate.5 While congenital hard palate defects generally occur in the midline, defects in the soft palate may occur in the midline or as a unilateral (asymmetrical) or bilateral hypoplasia (Fig. 56-2).5,11 While most cleft palates are believed to be inherited recessive or irregularly dominant traits, intrauterine infections and exposure to toxins at specific times during gestation may also result in a cleft palate.12 Acquired defects occur as a result of trauma (Fig. 56-3), including surgery and/or radiation therapy, severe periodontal disease, tooth removals, resection of neoplasms, or severe chronic infections.13 Siamese and Abyssinian cats may have a higher incidence of congenital palatal defects.2,12,14 Figure 56-2 Congenital hypoplasia of the soft palate in a five-year-old cat, resulting in a ‘uvula’ (Courtesy of Prue Neath.) Reconstruction of palatal defects can be challenging and requires a detailed knowledge of the local anatomy, as well as an understanding of the various options available to the surgeon.13 This is particularly important in cases of large defects, or when radiation or previous surgeries have compromised local tissue.15 The surgeon needs to work with the anatomical limitations, difficult access, and limited tissue available for local repair. Additionally, the repair must withstand the mechanical stresses induced during mastication and deglutition.15 Consideration should be made as to whether to temporarily divert food with a feeding tube (see Chapter 12). There are a number of general principles that should be followed when considering surgery on a patient with a palate defect (Box 56-1).12 Suture materials used are usually 4/0 or 5/ 0 absorbable monofilament suture material, depending on the size of the animal, type of repair and type of tissue being sutured.13 Non-absorbable sutures have also been used. If knots are left on the epithelial surface, they will usually slough within three to four weeks regardless of the type of suture material being used.16 There have been many techniques described to manage palatal defects, including local flaps4,16–19 axial pattern flaps,15,20 distant tissue using a rostral tongue flap,21 auricular cartilage free grafts,22 temporal muscle transfer,23 free tissue (muscle) transfer with microvascular anastomosis,24 and prosthetic appliances.25,26 Due to the similarities in anatomy between dogs and cats, techniques that have previously been reported in dogs are likely to be applicable to cats although scientific reports are lacking. The more common or useful techniques for reconstruction of the hard palate include mucoperiosteal flaps, mucoperiosteal releasing incisions, local flaps from the soft palate, buccal mucosal flaps, double reposition flaps, auricular cartilage free grafts, temporal muscle transfer, and prosthetic appliances.18,19,22,23,25–29 Mucoperiosteal flaps are easy to perform (Box 56-2), being mindful of the location of the palatine artery. While a single overlapping mucoperiosteal flap may be used,18 this may interfere with bone union in the case of a cleft palate.2 Achieving a two-layer closure is preferable to allow a more anatomic closure and potentially allow bridging of the bone defect.2
Palate
Surgical anatomy
General considerations
Surgical diseases

Surgical techniques
Reconstruction of the hard palate
Mucoperiosteal flaps and releasing incisions