Chapter 37 Ophthalmologic Diseases in Small Pet Mammals
Rabbits
Ophthalmic examination of rabbits can be performed easily.69,70 The eyes are laterally located and have a round pupil. Evaluation of a menace response is difficult, but most rabbits will react to bright light by squinting. The dorsal rectus muscle can usually be seen as a large striated band of tissue under the conjunctiva. Some rabbits do not respond to topical application of mydriatic agents because of the natural presence of atropinase. In these rabbits, the addition of 10% phenylephrine may help to obtain mydriasis. Rabbits have a merangiotic fundus. The well-myelinated optic nerve is present above the visual axis and has a deep optic cup. Retinal blood vessels are present in a linear streak medial and lateral to the optic nerve. An extensive venous plexus is present in the orbit. Tear production in rabbits can be measured by using Schirmer tear test strips. Average tear production is 5 mm/min (standard deviation, ±2.4 mm/min)1; however, very low values can be measured in some normal rabbits. Normal intraocular pressure measured by applanation tonometry is between 10 and 20 mm Hg.
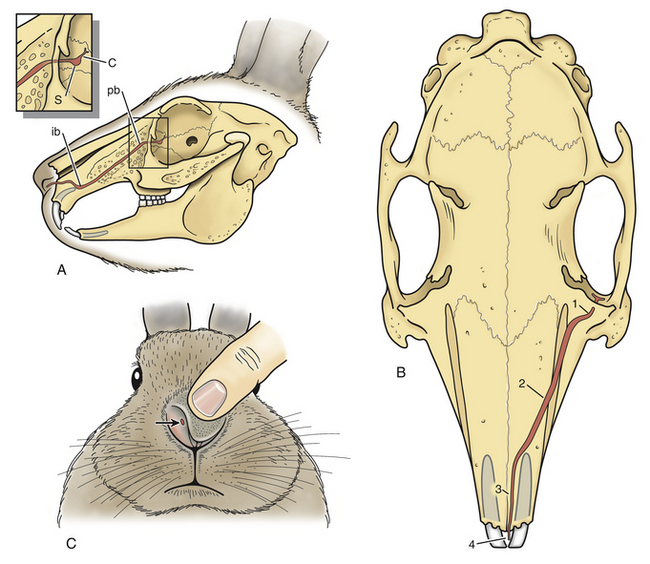
The nasolacrimal system of rabbits has a single nasolacrimal punctum. The punctum is located in the ventral eyelid 3 mm from the eyelid margin, near the medial canthus and ventral to the lacrimal caruncle (Fig. 37-1).9,38 The lacrimal sac is immediately rostral to the punctum and caudal to the nasolacrimal duct aperture. The nasolacrimal duct extends from the orbit to the nasal fossa and runs within the part of the maxilla that forms the lateral wall of the maxillary sinus.38 Approximately 5 to 6 mm within the maxilla, the duct curves sharply and decreases in diameter.9 At the level of the palatine bone, the nasolacrimal duct leaves the bony nasolacrimal canal and makes a sharp turn at the nasolacrimal duct flexure, which is located just caudal to the caudal limit of the incisor tooth roots. The nasolacrimal duct narrows at this flexure in normal rabbits. The duct then follows the ventral margin of the nasoturbinates and exits on the ventromedial aspect of the alar fold just caudal to the mucocutaneous junction of the nares.
Conjunctivitis and Epiphora
Conjunctivitis in rabbits is common. In normal rabbits with no ocular or respiratory disease, the most frequently isolated organisms from the conjunctival cul de sac include Staphylococcus, Micrococcus, and Bacillus species. Less common organisms include Bordetella, Stomatococcus, Neisseria, Pasteurella, Corynebacterium, Streptococcus, and Moraxella species.14 However, Pasteurella multocida is a cause of conjunctivitis, epiphora, nasolacrimal duct obstruction, and dacryocystitis in rabbits.27,38 A wide variety of other infectious agents also have been associated with conjunctivitis in rabbits, including Staphylococcus aureus, Pseudomonas species, Haemophilus species, Treponema paraluiscuniculi, mycoplasmas, chlamydiae, and myxoma virus.27,45,60 In New Zealand white rabbits with conjunctivitis, upper respiratory disease, and pneumonia, bacterial isolates consisted of Bordetella broncheptica, P. multocida, S. aureus, and Pseudomonas alcaligenes.50 Mucopurulent conjunctivitis and blepharitis with corneal ulceration have been associated with S. aureus infection in a rabbit.45 Treatment with topical gentamicin ophthalmic ointment and systemic gentamicin was curative. Methicillin-resistant S. aureus was isolated in a rabbit with severe bilateral conjunctivitis. (K. Quesenberry, personal communication). Other causes of conjunctivitis in rabbits include foreign bodies, entropion, distichia, trichiasis, and high ammonia or dust content in the environment. Dental disease, including root elongation and dental abscesses, is also associated with conjunctivitis.
Unilateral or bilateral epiphora can be present in rabbits without conjunctivitis. The discharge often has a white, gritty appearance and may be intermittent and resistant to treatment with topical antibiotics. Root elongation of the maxillary incisors is a common underlying cause.27 The elongated roots can cause an obstruction of the nasolacrimal duct at its flexure just caudal to the roots of the incisors. Radiographs of the skull are needed to assess the incisors; excess curvature of the incisor roots is abnormal. In one report describing two affected rabbits and 13 normal rabbits, radiographs revealed a cystic dilation of the nasolacrimal duct immediately caudal to the duct flexure, and the incisors were more arched than in normal rabbits.38 Irrigation of the nasolacrimal duct in affected rabbits yielded opaque, white, gritty fluid which, on cytologic examination, showed numerous macrophages, lipid-laden mesothelial cells, lipid droplets, and small numbers of bacteria and erythrocytes. Occlusion of the ducts was presumed to be attributed to fat droplets. Bacteriologic culture of fluids used to irrigate the nasolacrimal ducts of both normal and affected rabbits yielded similar bacterial isolates; therefore microorganisms may not be important in the pathogenesis of epiphora in rabbits. The most common bacterial isolates were S. aureus, coagulase-negative Staphylococcus species, Moraxella and Neisseria species, Oligella urethralis, and Streptococcus viridans. In a study of 28 cases of dacryocystitis in rabbits, 89% of cases were unilateral. The cause was determined to be dental malocclusion in 50%, no apparent cause in 35%, rhinitis in 7%, both rhinitis and dental malocclusion in 4%, and panophthalmitis in 4%. Most animals (98%) were treated with topical antibiotics, with a mean duration of 5.8 weeks.21
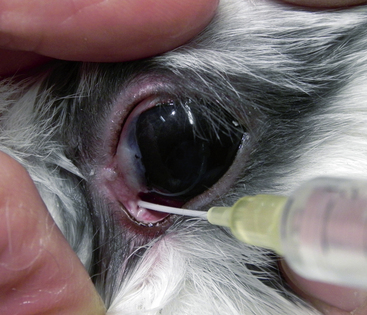
Treatment of epiphora in rabbits can be frustrating. Irrigation of the nasolacrimal duct is important to restore the patency of the nasolacrimal system. After instilling a topical ophthalmic anesthetic, use a 23-gauge lacrimal cannula or a 22- to 24-gauge Teflon intravenous catheter to flush the duct (Fig. 37-2). Recurrence of the obstruction is common, and duct irrigation may need to be repeated every 2 to 3 days or weekly until a few consecutive clear irrigations are obtained. If topical antibiotic therapy is used, a broad-spectrum medication such as triple antibiotic solution is recommended. Topical nonsteroidal, anti-inflammatory ophthalmic medications, such as 0.03% flurbiprofen or 0.1% diclofenac, may help minimize irritation caused by the procedure. In rabbits with chronic or severe infections, concurrent topical ophthalmic and systemic antibiotic therapy may be needed. Suggested combinations include systemic enrofloxacin (Baytril, Bayer Corporation, Shawnee Mission, KS) or marbofloxacin (Zeniquin, Pfizer Animal Health, Exton, PA) and topical ciprofloxacin or gentamicin ophthalmic solution. In rabbits with evidence of underlying incisor root elongation, removing the incisors can be considered in severe cases.
Cornea
Corneal dystrophy is the accumulation of cholesterol or lipid crystals in the cornea.4 This may develop spontaneously, as has been reported in American Dutch belted rabbits,47 or be due to high dietary cholesterol. It also occurs in breeds that are predisposed to hypercholesterolemia, such as the Watanabe rabbit with heritable hyperlipidemia.22,35 In Watanabe rabbits, yellowish-white granules can develop along the corneal-scleral junction and in the iris. In rabbits without systemic lipid abnormalities, spontaneous corneal dystrophy is usually bilateral and symmetric and does not progress to visual impairment. In any rabbit with corneal dystrophy, carefully evaluate the fat content of the diet.
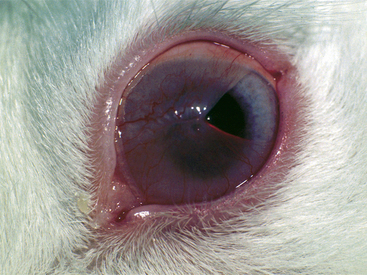
Progressive occlusion of the cornea with a conjunctiva-like membrane is occasionally seen in rabbits.3,18,57,59 Membranous corneal occlusion, or pseudopterygium, is a pain-free condition that may affect one or both eyes (Fig. 37-3). Ophthalmic examination reveals a circular membrane that originates at the limbus (the junction of the cornea and sclera) and gradually advances over the cornea. In severe cases, only a small central opening is present, allowing visibility of an otherwise normal globe. The membrane does not adhere to the cornea. The cause of this condition is unknown, although trauma has been suggested. Progressive membranous occlusion in rabbits has been compared with pterygium in humans. However, in humans the membrane is triangular and adherent to the cornea, whereas in rabbits it is nonadherent and circumferential from the limbus. Treatment with topical antibiotic or antibiotic-steroid medications has no effect. The membrane can be resected surgically and treated with topical antibiotics postoperatively; this usually results in quick recurrence of the membrane. However, if the membrane is resected a few millimeters beyond the limbus and the eye is then treated with a topical antibiotic-steroid combination, recurrence may be prevented. Good results have also been obtained with surgical resection and the use of topical cyclosporine with or without corticosteroids.57 Another described surgical technique is to incise the membrane into four to six quadrants and suture each quadrant of the membrane to the inside of the eyelid.3,59 With this technique, recurrence may be prevented for at least 1 year.
Uveitis and Diseases of the Lens
Encephalitozoon cuniculi may cause granulomatous encephalitis and renal lesions in rabbits. Many rabbits infected withE. cuniculi are asymptomatic, but neurologic signs can include convulsions, tremors, torticollis, paresis, and coma. Encephalitozoon cuniculi infection has also been associated with phacoclastic uveitis.20,23,63 Most affected rabbits are young (less than 2 years of age), and dwarf rabbits appear predisposed to this disease. Clinically, a white mass is often seen protruding into the anterior chamber (Fig. 37-4). Careful examination of the anterior segment of the eye with slit-lamp biomicroscopy may reveal a break in the anterior lens capsule. The break is frequently hidden by inflammatory material and it may appear as if only the iris is involved in the inflammatory process. A focal cataract is often present in the area of the anterior lens capsule break. Signs of a severe pyogranulomatous anterior uveitis are usually present, such as conjunctival hyperemia, a swollen hyperemic iris, miosis, aqueous flare, and low intraocular pressure. The posterior segment of the eye is initially normal; however, if left untreated, severe uveitis and cataract formation can lead to blindness and possible phthisis bulbi or glaucoma. An abscess in the iris caused by P. multocida initially may resemble phacoclastic uveitis. Measurement of serum antibody titers for E. cuniculi and P. multocida may aid in the differential diagnosis. The treatment of choice is surgical removal of the lens by phacofragmentation. Because of the rabbit’s ability to regenerate a lens after this procedure, insertion of an artificial lens after phacofragmentation is not recommended. Systemic treatment of E. cuniculi with albendazole (30 mg/kg PO q24h for 30 days, then 15 mg/kg PO q24h for an additional 30 days) has been reported.63 Fenbendazole (20 mg/kg q24h for 28 days) has proved effective in both preventing experimental E. cuniculi infection in rabbits and treating naturally infected seropositive rabbits.64 If the lens is not removed surgically, control of the uveitis with topical steroidal (such as 1% prednisolone acetate) and nonsteroidal anti-inflammatory medications as well as systemic fenbendazole or albendazole is necessary. Enucleation may be indicated if the uveitis cannot be controlled medically and a chronically painful eye is present.23,74
Spontaneous cataract formation is rare in rabbits. One report describes a low incidence of juvenile cataracts in laboratory New Zealand white rabbits.49 Keratitis caused by Shope fibroma virus has been reported in one rabbit.32 Cataracts developed 3 months after the keratitis, which may have been hereditary in origin and unrelated to the virus. Cataract and subsequent glaucoma can develop subsequent to ocular trauma, such as cat-scratch injury.
Intraocular sarcomas have been described in two adult rabbits; one had a nonvisual eye associated with chronic inflammation and the second had chronic uveitis, cataract formation, and glaucoma.42 In both rabbits, intraocular spindle cell neoplasms closely associated with lens and lens capsular fragments were described. The histologic features of the tumors closely resembled posttraumatic ocular sarcomas in cats; chronic inflammation and trauma were considered as probable causes.
Glaucoma
Congenital glaucoma is inherited as an autosomal recessive trait in rabbits. In those with this condition, the intraocular pressure is high as early as 3 months of age.10 With increasing age, progressive buphthalmos with a markedly enlarged cornea, structural abnormalities of the iridocorneal angle, atrophy of the ciliary processes, and excavation of the optic nerve develop. Topical glaucoma medications used in dogs, such as 0.5% timolol maleate and 2% dorzolamide, may also be used in rabbits. Because response to therapy is unpredictable in rabbits, carefully monitor the intraocular pressure during treatment. Enucleation, insertion of an intrascleral prosthesis, and laser cycloablation with a diode laser have also been used to manage glaucoma in pigmented pet rabbits. However, laser cycloablation cannot be used in albino rabbits. If left untreated in chronic cases, pressure-induced atrophy of the ciliary body may lead the intraocular pressure to return to normal.
Orbit
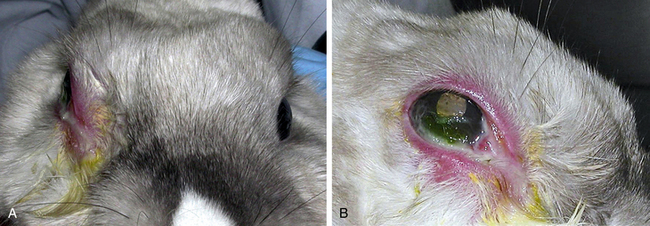
Retrobulbar disease processes are occasionally seen in rabbits. Clinical signs include progressive exophthalmos, protrusion of the third eyelid, and inability to retropulse the globe. Exposure keratitis may be present if the ability of the eyelids to close properly has been affected (Fig. 37-5). Abscesses are the common cause of retrobulbar disease in rabbits; dental disease with tooth root abscessation is often a predisposing factor (see Chapter 32). Infection is caused by both aerobic and anaerobic bacterial species. A thorough dental examination and skull radiographs are indicated in any rabbit with a suspected retrobulbar mass (see Chapter 35). If available, a computed tomography (CT) scan is especially helpful in diagnosis Taenia serialis coenurus formation caused exophthalmos in a pet rabbit. Surgical removal was curative.51 Retrobulbar neoplasia is uncommon in rabbits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree