Chapter 11 Obstructive Uropathy and Nephropathy
Introduction
A. Obstructive nephropathy refers to the functional and anatomical effects of obstruction on the kidney.
B. Obstructive uropathy refers to local effects on the urinary tract at the site of obstruction as well as to effects on sites proximal to the obstruction, including the kidneys.
C. Total obstruction of one kidney eventually results in the total destruction of the renal parenchyma.
D. Partial obstruction, or complete short-term obstruction, results in decreased renal function that may be reversible if adequate urine flow can be re-established promptly.
E. Total obstruction of both kidneys is not compatible with life, and death occurs in experimental animals with complete obstruction after 3 to 5 days.
Lower Urinary Tract Obstruction
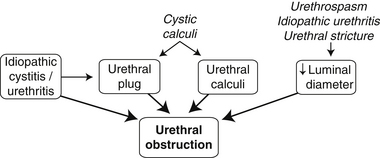
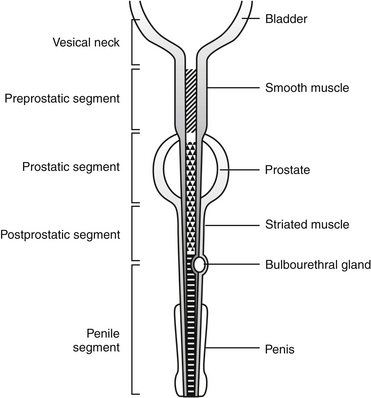
A. Obstruction within the urethra is the most common cause (Figure 11-1).
Urethral Obstruction (UO) in Male Cats
Causes and Associations
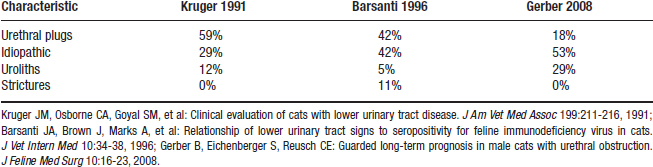
Urethral Plugs (Figure 11-3)
c. Urethral plugs have minimal intrinsic cohesive structure but often are cylinder-shaped after extrusion from the urethra.
d. Urethral plugs are fundamentally different from calculi that lodge within the urethra (i.e., urethroliths).
(1) Uroliths have an organized internal structure with much less matrix and are not easily compressed or distorted.
(3) The predominant mineral composition in most plugs is magnesium ammonium phosphate hexahydrate (i.e., struvite). This is true despite the fact that cats form calcium oxalate and struvite uroliths with nearly equal frequency.
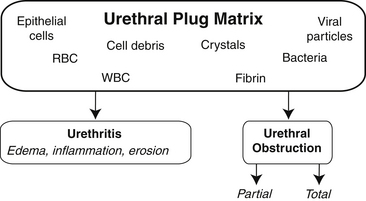
(4) Secondary components can contribute to plug formation, including inflammatory exudate (i.e., white cells, proteins), red cells, cellular debris, sloughed tissue (i.e., epithelial cells), struvite crystals, and combinations of these (Figure 11-4).
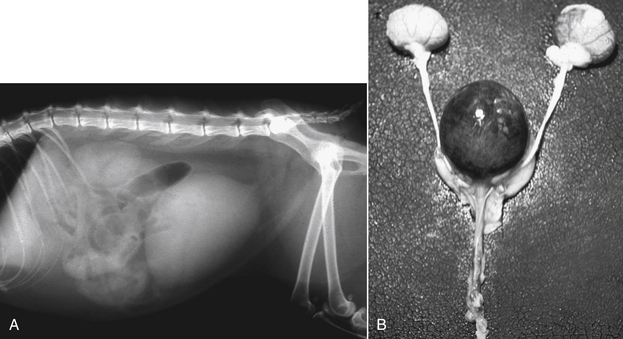
e. Most plugs are assumed to lodge within the penile urethra, but obstructions also can occur at more proximal sites (Figure 11-5).
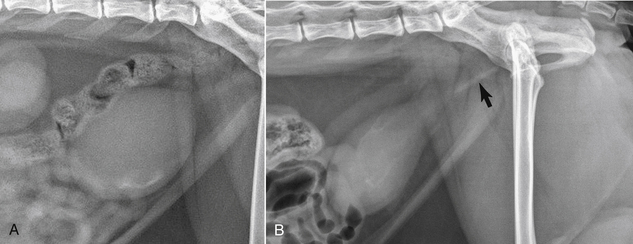
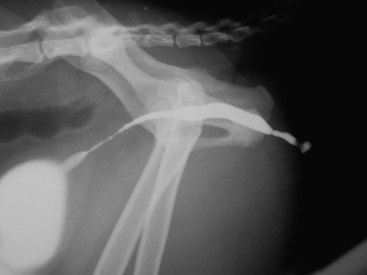
f. Definitive diagnosis of a urethral plug requires retrieval of the plug. Supportive evidence for the presence of a urethral plug can be seen on radiographs in some cats with UO (Figure 11-6).
(1) Many veterinarians assume that a urethral plug has been dislodged during hydropulsion and attempts to pass a urethral catheter when the catheter suddenly advances.
(2) This could indicate movement of a plug into the bladder or it could indicate that resistance caused by urethral spasm has been overcome.
(3) Retrieval of a plug or retropulsion of the plug into the bladder does not always result in restoration of normal urine flow (several other factors initiate or maintain the obstructing process).
g. Previously, the crystalline-matrix hypothesis proposed that plugs that then became embedded in a matrix formed secondary to precipitation of struvite crystals in the urine. According to this hypothesis, plugs created UO and urethritis.
Urethral Calculi (Figure 11-7)
Idiopathic
c. Obstruction is secondary to functional urethral spasm in addition to swelling of the urethra due to edema and hemorrhage.
(1) Refers to pathologic or neurogenic processes that cause contraction of the circular smooth or skeletal muscle of the urethra or both.
(2) Part of urethral tone maintained by the skeletal muscle (so-called rhabdosphincter) is influenced by sympathetic innervation.
d. Bacterial urinary tract infection (UTI) is very uncommon before urethral catheterization. UTI deserves more consideration in cats with recurrent UO that have undergone urinary instrumentation.
Signalment and History
A. The majority of cats with UO are relatively stable; approximately 10% are critically ill. Increased client awareness that male cats can have a life-threatening emergency associated with “urinary blockage” likely is responsible for these percentages.
D. Most affected cats in the United States are neutered males. Intact males comprise 10% of cats with UO.
G. Clinical signs depend on the completeness of the obstruction and its duration. Cats with long-standing obstruction display signs of uremia (e.g., vomiting, lethargy, dehydration) in addition to signs referable to the lower urinary tract (e.g., stranguria, pollakiuria, hematuria, pain, overflow incontinence).
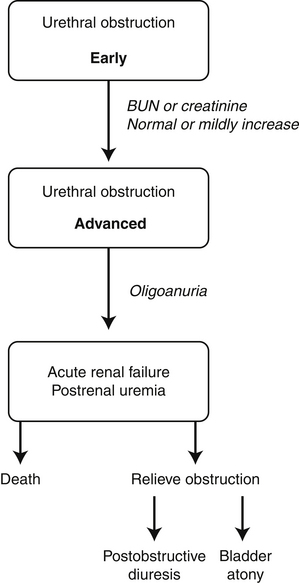
1. Cats with experimental UO do not demonstrate signs of uremia until after 24 to 48 hours of complete obstruction (Figure 11-9).
4. By 72 hours, many cats are moribund and some die. Some cats can survive periods of UO up to 98 hours, however.
Physical Examination
K. Tachypnea (median, 36 breaths per minute). As respiratory rate increases, there is less likelihood of severe hyperkalemia.
L. Rectal temperature of <95° F-96.6° F heart rate of <120 bpm was the most accurate predictor of severe hyperkalemia. A combination of hypothermia and bradycardia was 98% to 100% predictive for severe hyperkalemia (> 8.0 mEq/L).
N. Systemic blood pressure most often is normal.
1. Median systolic blood pressure was 135 mm Hg, median mean arterial pressure was 120 mm Hg, and median diastolic blood pressure was 108 mm Hg in a study of 28 affected cats (Malouin, Milligan and Drobatz, 2007).
5. Normal blood pressure at initial presentation may be misleading because of combinations of major stress, hypovolemia, and bradycardia.
6. Mean arterial pressure correlated inversely with serum potassium and directly with total serum calcium concentrations.
Diagnostics
Serum Biochemistry
4. Serum phosphorus concentration: Median, 5.0 mg/dL; range, 2.8 to 20 mg/dL; 25% were above the reference range and 6% were below the reference range. We have observed serum phosphorus concentrations between 20 and 30 mg/dL.
6. Blood gases.
a. Median venous pH was 7.29 in 198 cats (range, 7.02 to 7.45); 40% were below the reference range and 4.5% were above the reference range.
b. Median venous pCO2 was 40.2 mm Hg (range, 26.6 to 74.2 mm Hg); 13% were below the reference range and 30% were above the reference range.
e. Serum total calcium concentration in 51 cats was below the reference range in 39%, above the reference range in 0%, and within the reference range in 61%.
f. Serum ionized calcium concentration was negatively correlated with BUN, serum creatinine, serum phosphorus, and serum potassium concentrations.
g. Serum ionized calcium concentration was positively correlated with venous pH in contrast to the expected decrease in ionized calcium concentration associated with increasing pH under normal circumstances.
h. Cats with low serum total calcium concentrations had moderate to severely decreased serum ionized calcium concentrations (Drobatz, Hughes, 1997.). In one study, more cats were found to have hypocalcemia when defined by measurement of serum ionized calcium concentration (75%) than when defined by serum total calcium concentration (27%).
i. Serum parathyroid hormone (PTH) concentration was increased in 63% of cats with UO in one study, including 8 cats with low and 4 cats with normal serum ionized calcium concentrations (Drobatz, Ward, Graham, et al., 2005). Serum PTH concentration was much higher in cats with hypocalcemia as compared with those with normocalcemia. Serum 25-hydroxycholecalciferol status was not correlated to serum ionized calcium concentration.
j. Low serum ionized calcium concentration is not a consequence of deficient secretion of PTH, nor does it appear related to serum concentrations of 25-hydroxycholecalciferol. Rather, it likely is a consequence of increased serum phosphorus concentration. The potential role of decreased serum calcitriol concentration has not been studied.
Urinalysis
1. Urine specific gravity (USG) is unpredictable. USG can be >1.040 when evaluated early during UO. In more advanced cases, submaximal urine concentration can occur due to the effects of obstruction on renal tubular function.
2. Red blood cells (RBCs): Hematuria is almost always observed because of the presence of underlying idiopathic urethritis/cystitis and the effects of overdistension of the bladder wall with resultant hemorrhage.
3. White blood cells (WBCs): A mild increase can be observed, but numbers of WBCs in the sediment may be normal.
4. Epithelial cells: A mild increase can be seen; occasionally rafts of epithelial cells are observed in the urine sediment.
5. Bacteria usually are not present, but often are described as present because particulate matter in the urine sediment may resemble bacteria and be erroneously interpreted as such.
6. Crystals: Struvite crystals may be observed, especially if urine pH is alkaline. Crystals are more likely to be secondary to urine stasis or alkaline urine pH than a primary cause of obstruction.
8. pH often is neutral to alkaline due to anorexia and plasma protein exudation into urine from bleeding.
9. Glucosuria: Positive glucose oxidase dipstrip reactions are sometimes observed.
a. Detected in 74% of cats with severe UO in one study (Burrows, Bovee, 1978). Detected in 40% of cats with less severe UO (Loeb, 1971).
b. Thought to be a consequence of stress hyperglycemia. Moderate hyperglycemia occurs in many cats with UO, but frequently not above the renal threshold for glucose.
Urine Culture
Abdominal and Urinary Tract Imaging
Radiography
a. Abdominal radiographs should be obtained in all cats with UO to rule out the presence of radiopaque calculi in the bladder or urethra. It is very important to include the perineal region in the radiographs to identify urethral calculi.
b. Evaluation of the kidneys and ureters to be sure nephroliths or ureteroliths are not part of the overall process is important because upper urinary tract involvement can markedly affect the overall prognosis.
c. Free fluid resulting in a loss of abdominal detail can be seen in some cats with severely distended urinary bladders.
d. Free fluid has been observed at surgery and necropsy in some UO cats in which no tear in the bladder or urethral wall could be demonstrated. This fluid likely arises from transmural movement across an inflamed and highly permeable bladder wall (i.e., underlying idiopathic cystitis) subjected to increased hydrostatic pressure from UO.
Contrast Radiographic Studies
Treatment of Urethral Obstruction
B. The severity of clinical signs from uremia, electrocardiographic (ECG) findings, and magnitude of bladder distension dictate how quickly and in what order treatments must be performed.
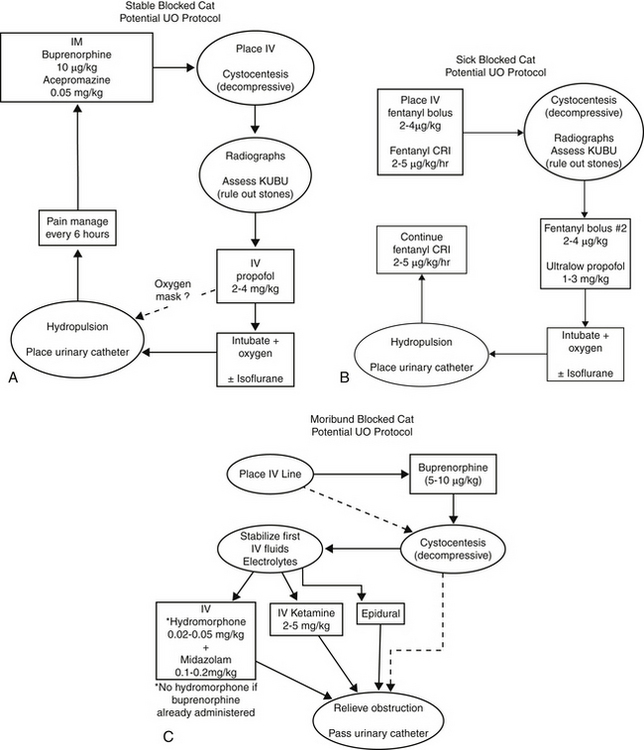
C. Cats in uremic crisis and those with very large turgid bladders are in need of prompt attention (Figure 11-11).
E. Stabilize the patient and treat the adverse effects of uremia, if present, before administering any anesthetic agents. Hypovolemia, hyperkalemia, metabolic acidosis, and hypocalcemia must be treated first.
1. Intravenous (IV) administration of fluids is needed for seriously ill cats with UO. Ten of 13 cats died after relief of advanced UO when not treated with IV fluids (Finco, Cornelius, 1977).
a. IV fluid therapy at 10 to 20 mL/kg/hr is started and the rate adjusted as the animal becomes more stable.
c. 0.9% NaCl corrects chloride deficits faster than more balanced electrolyte solutions (e.g., lactated Ringer’s solution) due to the relatively high chloride concentration (154 mEq/L) (Drobatz, 2008), but the high chloride concentration of 0.9% NaCl also makes it an acidifying solution.
d. No difference in the rate of decline in serum potassium concentration was seen in a randomized study of 68 cats with UO (22 with hyperkalemia and 31 with metabolic acidosis) treated with 0.9% NaCl compared with a more balanced polyelectrolyte solution containing 5 mEq/L of potassium as well as the base precursors acetate and gluconate (i.e., Normosol-R, Abbott Laboratories, North Chicago, Ill.).
e. More rapid correction of acidosis was accomplished within 12 hours of treatment with the more balanced polyelectrolyte solution compared with 0.9% NaCl.
f. From a practical point of view, both fluid types are acceptable for treatment of most cats with UO.
2. Management of hyperkalemia will be needed in the approximately 12% of cats that have severe hyperkalemia and may be warranted in another 12% that have moderate hyperkalemia. No specific treatment is needed for cats with mild hyperkalemia.
a. Restoration of normal renal function after relief of obstruction results in kaliuresis and a rapid decrease in serum potassium concentration.
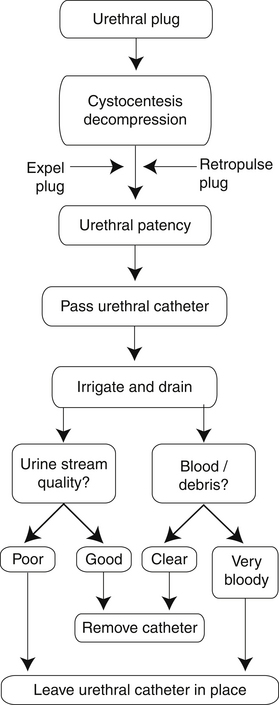
FIGURE 11-10 A decision-making algorithm for management of urethral obstruction due to a urethral plugs in male cats.
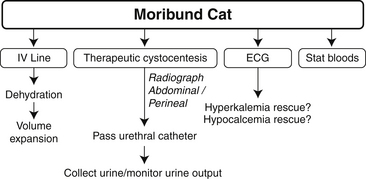
FIGURE 11-11 Overview of the approach to the moribund cat with advanced urethral obstruction. ECG, electrocardiogram.
(2) This treatment stabilizes the heart, but does nothing to change the severity of the hyperkalemia.
(3) 50 to 100 mg/kg of calcium gluconate (0.5 to 1.0 mL/kg of 10% calcium gluconate) is given over 2 to 3 minutes with continuous ECG monitoring.
c. IV dextrose is helpful for longer term control of hyperkalemia, especially if serum potassium concentration initially is >8.0 mEq/L.
d. Some clinicians also give one unit regular insulin IV to further stimulate the transcellular shift of potassium. Insulin should always be given with a bolus injection of dextrose with or without a constant rate infusion of dextrose to prevent hypoglycemia.
e. Sodium bicarbonate may be administered IV in cats with serum potassium concentration >10.0 mEq/L.
(1) 1 mEq/kg (1 mL/kg of an 8.4% sodium bicarbonate solution) is the standard dosage of sodium bicarbonate.
(2) 4 mEq/kg (4 mL/kg of an 8.4% sodium bicarbonate solution) is the maximal dosage of sodium bicarbonate.
3. Management of acidosis will be needed in approximately 6% of cats with severe acidosis and may be warranted in another 9% with moderate acidosis. No specific treatment is needed for cats with mild acidosis.
a. Restoration of normal renal function after relief of obstruction allows for rapid correction of metabolic acidosis, especially when an alkalinizing polyelectrolyte crystalloid solution (e.g., lactated Ringer’s solution, Normosol-R) is used for IV fluid therapy.
b. In cats with severe metabolic acidosis, 1 mEq/kg of sodium bicarbonate is given by IV infusion and then acid-base status is checked after 15 to 30 minutes to see if more sodium bicarbonate should be given. A partial increase in blood pH back toward normal is the goal rather than full restoration of normal blood pH.
4. Management of hypocalcemia.
b. Relief of obstruction usually results in rapid correction of serum calcium concentration as serum phosphorus concentration decreases toward normal.
c. An IV infusion of calcium gluconate is administered until the desired effect is achieved in cats that have muscular twitching or seizures.
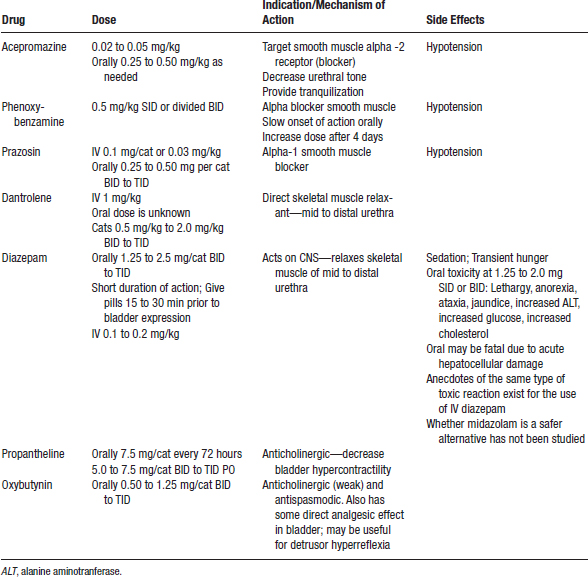
F. Sedation and analgesia for relief of obstruction due to urethral plugs, idiopathic urethritis/cystitis, or urethral stones (Table 11-2).
3. Nearly all cats benefit from preanesthetic analgesics to decrease pain and anxiety; these usually are given before decompressive cystocentesis and before anesthesia to pass a urinary catheter.
4. Urethral relaxation while the cat is sedated or under anesthesia may increase the likelihood of urethral plug dislodgment or facilitate urethral relaxation.
Decompressive (Therapeutic) Cystocentesis
1. Cystocentesis to empty the bladder should be performed as soon as possible in cats with very enlarged bladders to prevent rupture of the bladder and to allow renal excretory function to resume.
2. Cystocentesis allows for rapid reduction of urinary tract pressure and resumption of GFR compared with catheterization, which can take considerable time. Decompressive cystocentesis may stabilize the cat before anesthesia for urinary catheter placement.
3. Relief of bladder pressure before urethral catheterization also may facilitate efforts to dislodge urethral plugs, and allows collection of a superior urine sample for analysis before manipulation of the urinary tract and contamination by irrigation solutions.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree