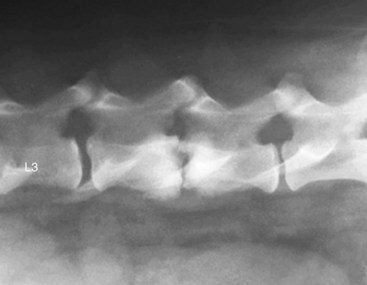
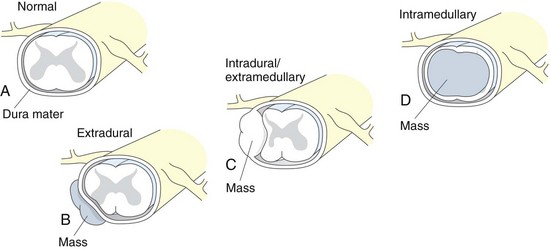
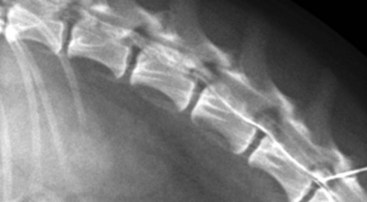
Chapter 37 As the complexity of neurosurgical cases seen by surgeons and neurologists has increased, so has the complexity of diagnostic procedures and treatments. Many of the diagnostic procedures discussed in this chapter will be performed and/or interpreted primarily by neurologists and radiologists. Neurodiagnostic procedures include, but are not limited to, radiography, contrast radiography, ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI), electrodiagnostic procedures (e.g., electromyography, nerve conduction studies), cerebrospinal fluid (CSF) examination, stereotactic brain biopsy, and nerve/muscle biopsy. Whereas a superficial understanding of more commonly performed electrodiagnostic procedures is more than sufficient for a surgeon’s purposes, the same cannot be said about advanced imaging. In particular, it is imperative for the small animal surgeon who intends to maintain a foothold in the realm of neurosurgery to have at least a working knowledge of basic MRI physics and to gain some experience in reading MR images (see Chapter 15). Contrast radiography is rapidly becoming a historic mode of imaging, with most private specialty and academic specialty hospitals preferentially using MR imaging for both brain and spinal cord disorders. The purpose of this chapter is to provide the small animal surgeon with the fundamental principles of various neurodiagnostic modalities. The modalities of CT and MRI are not discussed in this chapter; they are covered in detail in Chapter 15. Radiography and Contrast Radiography The roles of radiography and contrast radiography in modern veterinary neuroimaging have diminished tremendously coincident with ready availability of MR imaging. High-quality radiographs of the skull and vertebrae typically require sedation or general anesthesia and generally are low yield in comparison with CT and MR imaging. Despite this, certain disorders that cause bone lysis and/or production (e.g., skull tumors, diskospondylitis) will usually be apparent on survey radiographs (Fig. 37-1). Also, survey radiographs are typically taken in spinal trauma patients to evaluate for any obvious fractures or luxations (Fig. 37-2). The most common contrast radiographic procedure performed in veterinary neurology is myelography. Myelography is a procedure in which spinal radiographs are obtained following injection of a radio-opaque contrast agent into the subarachnoid space (Box 37-1). It is used to assist in the diagnosis of certain myelopathies and is indicated for cases in which survey radiographs are normal or inconclusive, despite neurologic evidence of myelopathy. It is also often helpful in estimating the location, extent, and severity of spinal lesions. The ability to easily and rapidly visualize the entire spinal cord is an advantage of myelography over other imaging procedures (e.g., CT, MRI). Myelography is generally less costly and may be more readily available than CT or MRI in certain situations (e.g., emergencies). Myelography can be performed via a cisternal or lumbar tap. Cerebrospinal fluid should be collected before contrast injection because the contrast will change the composition of the CSF and may prevent accurate analysis for at least 3 to 5 days. Lumbar myelography often results in better image quality, even for lesions in the cervical region, and is safer than cisternal myelography. Techniques and dosages for myelography are provided in Box 37-1. Despite the positive aspects of myelography, it is a somewhat invasive procedure and is associated with a low level of inherent risk. Postmyelographic seizures occur in approximately 10% to 20% of dogs undergoing the procedure; this adverse event is more likely to occur in dogs larger than 20 kg and is more likely after cisternal versus lumbar contrast injections. The likelihood of postmyelographic seizure activity increases with increasing total volume of contrast agent injected (not the dose on a ml/kg basis). In one large study, approximately 21% of myelogram patients experienced seizure activity post procedure (Barone et al, 2002). In this aforementioned study, dogs larger than 20 kg had a seizure prevalence of about 34%, whereas dogs weighing less than 20 kg had a prevalence of approximately 12%. Thirty-five percent of dogs with cisternal injections had seizures following the procedure compared with 5% with lumbar injections. Finally, this study demonstrated that each 5-ml increase in injected iohexol volume equated to a 30% increase in seizure likelihood. Dogs with and without seizure activity post myelography had mean total contrast injected volumes of 16.8 ml and 9.1 ml, respectively. Male Doberman Pinschers with caudal cervical spondylomyelopathy (i.e., “wobblers” syndrome) may be particularly predisposed to postmyelographic seizure activity. Most patients that seizure will do so only once or twice in the 24 hours following the procedure, and seizures usually cease with intravenous diazepam injection (see Box 37-1). Administering a single IV dose of levetiracetam (20 mg/kg over 5 minutes) during anesthetic recovery appears to reduce the incidence of postmyelographic seizures. Maintaining slight elevation of the patient’s head during and after the procedure (until the patient is awake) and ensuring hydration with intravenous fluids during and 24 hours after myelography are recommended to limit the occurrence and severity of postmyelographic seizures. Four basic myelographic patterns have been identified: normal, extradural, intradural/extramedullary, and intramedullary (Fig. 37-3). Normally, the contrast columns parallel each other and conform to the vertebral canal, except at the cauda equina region, where the subarachnoid space tapers. The spinal cord ends at about the L6 vertebral region in most dogs and at the first sacral vertebral region in most cats, although quite a bit of variation has been noted between breeds. Intervertebral disk extrusion/protrusion is the most common cause of an extradural myelographic pattern. Other causes of extradural patterns include vertebral fracture/luxation, congenital vertebral anomalies, hypertrophied soft tissue structures (e.g., interarcuate ligament, synovial membranes), extradural hemorrhage, vertebral neoplasia, and soft tissue neoplasia (e.g., feline lymphosarcoma). It is important to realize that the nature of an extradural compression is best appreciated when viewed tangential to the direction of the cord deviation. For example, if a disk extrusion is compressing the cord from ventral to dorsal with no lateralizing component, the myelographic pattern as viewed from a ventrodorsal view (parallel with direction of compression) could be misinterpreted as intramedullary. With intervertebral disk extrusions, which are often ventrolateral (i.e., ventral but somewhat lateralized), it is usually helpful to obtain oblique views in addition to standard dorsal and ventral views to ascertain the correct side of disk extrusion for purposes of surgical planning. The accuracy of correctly identifying the side of disk extrusion was significantly higher for oblique versus ventral views in one study, but the accuracy was higher still when information from these views was combined (Gibbons et al, 2006). An intradural/extramedullary pattern is produced when a lesion within the subarachnoid space (intradural) is not invading the parenchyma of the cord (extramedullary). As the contrast flows around the obstructive lesion, it may be outlined, appearing as a “filling defect.” Sometimes, the filling defect is incompletely outlined and resembles a golf tee, hence the term golf tee sign (Fig. 37-4). Intradural/extramedullary patterns are most often associated with neoplasia, primarily meningiomas and nerve sheath tumors. Intradural hemorrhage may rarely lead to this myelographic pattern. Intradural/extramedullary lesions may produce enough spinal cord swelling that contrast is excluded from the region of the mass. In such cases, the myelographic pattern may appear to be intramedullary; a CT is often performed through the abnormal region because contrast is better visualized on CT images. An intramedullary pattern is typically associated with spinal cord edema, expansile parenchymal masses, or intraparenchymal hemorrhage. Differential diagnoses include fibrocartilaginous emboli, neoplasia (e.g., astrocytoma, lymphosarcoma), inflammatory disorders (e.g., granulomatous meningoencephalitis [GME] in dogs, feline infectious peritonitis [FIP] in cats), and trauma (e.g., hemorrhage, edema). In addition to apparent spinal cord swelling on myelographic images, contrast leakage into the spinal cord parenchyma may be appreciated in cases of spinal cord myelomalacia (Fig. 37-5). Barone, G, Ziemer, LS, Shofer, FS, Steinberg, SA. Risk factors associated with development of seizures after use of iohexol myelography in dogs: 182 cases (1998). J Am Vet Med Assoc. 2002;220:1499. Gibbons, SE, Macias, C, De Stefani, A, McKee, WM. The value of oblique versus ventrodorsal myelographic views for lesion lateralization in canine thoracolumbar disc disease. J Small Anim Pract. 2006;47:658.
Neurodiagnostic Overview for the Small Animal Surgeon
References
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neurodiagnostic Overview for the Small Animal Surgeon