Chapter 25 Muscle Relaxants
Muscle relaxants may be chosen for use in veterinary patients for several reasons. Because of their muscle-relaxing effects, they are used during certain surgical procedures. Orthopedic procedures such as dislocation and fracture reductions can be performed more easily because of abolished skeletal muscle tone.1 When a balanced anesthesia technique is used that combines opioids, nitrous oxide, and low-dose inhalant agents, muscle relaxation is greatly improved if a neuromuscular blocking agent is given. This technique is especially beneficial for critically ill patients in which high doses of inhalant agents may lead to unwanted cardiovascular depression.2 During intraocular procedures or for patients with penetrating eye injuries requiring surgery, muscle relaxants may be beneficial by producing a central pupil, motionless eye, and soft globe. When used during induction and intubation, they can help prevent an increase in intraocular pressure that can occur during coughing or vomiting.2
Neuromuscular Blocking Agents
Anatomy and Physiology of the Neuromuscular Junction
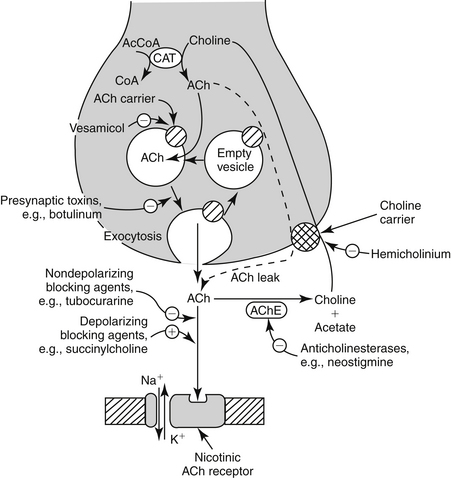
The components of the skeletal neuromuscular junction include the somatic motor nerve terminal, synaptic cleft, and the motor end plate of the muscle fiber. The cell bodies of the somatic motor neurons are located within the spinal cord. The axon divides into multiple branches, each of which innervates a single muscle fiber in mammalian species. At each neuromuscular junction, the terminal portion of the axon loses its myelin sheath and forms an arborization that lies in close proximity to the motor end plate of the muscle fiber (Figure 25-1). The site of action of neuromuscular blocking agents is at the nicotinic cholinergic receptors located at the motor end plate of the muscle fiber.
Pharmacology
Neuromuscular blocking agents exert their effects by interfering with the postsynaptic action of ACh. They can be divided into two classes, depolarizing and nondepolarizing neuromuscular blocking agents. Nondepolarizing drugs produce muscle relaxation by preventing ACh from binding to its receptors on the motor end plate. As a result of this competitive antagonism, the ion channels will not open, no shift in the resting membrane potential will occur, the motor end plate will not depolarize, and the muscle becomes flaccid. Complete neuromuscular blockade will occur when approximately 90% to 95% of the receptors are occupied.3
Individual Agents
The development of newer muscle relaxants has given the practitioner many options when selecting which agent to use. These drugs differ in their onset and duration of action, recovery time, cardiovascular effects, and route of elimination. When making the decision on which muscle relaxant to use, it is important to consider the reason for neuromuscular blockade, the desired duration of action, and the physical status of the patient. Organ dysfunction and concurrent drug administration may alter the clinical effect of muscle relaxants. Doses for depolarizing and nondepolarizing neuromuscular blocking agents for dogs and cats are listed in Table 25-1.
Table 25-1 Doses of Neuromuscular Blocking Agents for Dogs and Cats
| Drug | Dose (mg/kg IV) |
|---|---|
| Succinylcholine∗ | |
| Atracurium∗ | 0.22 |
| Cisatracurium† | 0.1 |
| Vecuronium∗ | 0.1 |
| Pancuronium∗ | 0.044-0.11 |
| Mivacurium‡ | 0.01 – 0.05 |
| Rocuronium§ | 0.18 |
| Doxacurium¶ | 0.008 |
IV, Intravenous.
∗ Plumb DC: Veterinary drug handbook, Ames, Iowa, 2005, Blackwell.
† Adams WA, Robinson KJ, Senior JM: The use of the neuromuscular blocking drug cis-atracurium in dogs, Vet Anaesth Analg 28:156, 2001.
‡ Smith LJ, Moon PF, Lukasik VM et al: Duration of action and hemodynamic properties of mivacurium chloride in dogs anesthetized with halothane, Am J Vet Res 60:1047, 1999.
§ Cason B, Baker DG, Hickey RF et al: Cardiovascular and neuromuscular effect of three steroidal neuromuscular blocking drugs in dogs, Anesth Analg 70:382, 1990.
¶ Savarese JJ, Wastila WB, Basta SJ et al: Pharmacology of BW A938U, Anesth 59(3):A274, 1987.
Depolarizing Agents
Succinylcholine
Succinylcholine is the only depolarizing neuromuscular blocking agent in clinical use today. Succinylcholine has a rapid onset of action, and its short duration of action is primarily due to rapid hydrolysis by plasma cholinesterase.4 For these reasons succinylcholine is used routinely to facilitate endotracheal intubation in human patients. Its use in small animal patients has been limited because the larynx of the dog and cat is easily visualized and does not routinely exhibit excessive laryngospasm, making neuromuscular blockade unnecessary for intubation.5
Because of the short duration of action of succinylcholine, frequent redosing or a constant-rate infusion is required if long-term neuromuscular blockade is desired. This may lead to tachyphylaxis (increased dose requirement) and change the character of the initial block (phase I block) to one similar to that produced with nondepolarizing blocking agents (phase II block), which may increase recovery time and require the use of a reversal agent (anticholinesterase therapy).6
Use of succinylcholine may be associated with significant side effects. A transient increase in serum potassium concentration occurs because of the leakage of potassium from the interior of cells. Severe, life-threatening hyperkalemia can occur after succinylcholine administration in patients with severe burns, trauma, nerve damage, neuromuscular disease, closed head injury, intraabdominal infections, and renal failure.7 Succinylcholine should also be avoided in patients in which increases in intraocular, intracranial, and intragastric pressures are undesirable. Other side effects of succinylcholine administration include myalgia and cardiac arrhythmias (e.g., sinus bradycardia, catecholamine-induced ventricular arrhythmias).7
Any agent than inhibits plasma cholinesterase (organophosphates, procaine) will prolong the duration of action of succinylcholine. Certain disease states such as liver disease, malnutrition, and chronic anemia can decrease the plasma cholinesterase level. Succinylcholine must be used cautiously, if at all, in these patients.4
Nondepolarizing Agents
Atracurium besylate
Atracurium is an intermediate-acting nondepolarizing agent with an onset of action of 3 to 5 min and a duration of action of 20 to 35 min.8 It is metabolized primarily through Hofmann elimination and ester hydrolysis.9 For this reason atracurium is the muscle relaxant of choice in patients with hepatic or renal disease. The rate of spontaneous degradation through Hofmann elimination is pH and temperature dependent. Both acidemia and hypothermia will prolong atracurium-induced neuromuscular blockade. Administration of atracurium can cause histamine release at higher doses, resulting in hypotension and tachycardia. Atracurium should be avoided in patients in which cardiovascular stability is desired. Administration of large doses slowly will attenuate these effects.10 Repeated doses or an infusion of atracurium produces a consistent degree of block and duration of action because of its noncumulative effects, making it an attractive choice for a constant-rate infusion for long-term paralysis.11,12 A metabolite of atracurium, laudanosine, can cause central nervous system (CNS) stimulation and cardiovascular depression, but this problem is rarely seen when clinical doses are used.12
Cisatracurium besylate
Cistracurium is the purified form of one of the 10 stereoisomers of atracurium. Because of this, the neuromuscular-blocking profile of cisatracurium is similar to that of atracurium. However, it is less likely to lead to histamine release. When administered to cats at up to 60 times the effective dose in 95% of cases (ED95), plasma histamine levels were unchanged.13 In human patients Hofmann elimination accounts for 77% and renal clearance accounts for 16% of total body clearance.14 A study in anesthetized dogs reported the onset of action as 3.8 minutes and duration of action as 27.2 minutes.15
Vecuronium bromide
Vecuronium is an intermediate-acting nondepolarizing agent with an onset of action of 2 minutes and duration of action of 25 minutes.8 The lack of cardiovascular or histamine-releasing effects, even at higher doses, is an advantage.12 Vecuronium is the muscle relaxant of choice for patients when hemodynamic stability is needed. Recovery from vecuronium-induced muscle relaxation depends on hepatic elimination. Animals with hepatic disease may exhibit a prolonged duration of action. Vecuronium is noncumulative and is well suited for repeated doses or constant-rate infusions.12
Pancuronium bromide
Pancuronium is a long-acting nondepolarizing agent with an onset of action of 2 to 3 minutes and duration of action of 30 to 45 minutes.8 It lacks histamine-releasing effects but does possess vagolytic and sympathomimetic effects, which can result in tachycardia, increased arterial blood pressure, and catecholamine-induced ventricular arrhythmias.16 Pancuronium is mainly eliminated by the kidney, with the remainder undergoing hepatic metabolism; therefore is should be used with caution in patients with renal or hepatic disease.17 Repeated doses or infusions of pancuronium are cumulative and can produce a delayed recovery.18
Mivacurium chloride
Mivacurium was recently developed as an alternative to succinylcholine for intubation in human patients. Its onset of action is 1 to 2 minute, with a duration of action of 15 to 20 minutes.19 Because its metabolism is by way of plasma cholinesterase, prolonged recoveries are possible in patients with hepatic disease, renal disease, or organophosphate toxicity.20 Mivacurium can cause histamine release, is noncumulative, and can be used for infusion administration.19 In human patients the onset and depth of blockade has a high interpatient variability. Preliminary work in dogs suggested that the dose should be reduced below doses used in human patients.21 In a later study, it was shown that one third of the human dose given to dogs resulted in a duration of action five times longer than that with human patients.22 The species differences may be explained, in part, by the fact that normal plasma cholinesterase levels in dogs vary from 19% to 76% of human patients.23 Also, the canine pseudocholinesterase enzyme may exhibit different affinity for the three primary isomers of mivacurium.23 Mivacurium has not been available in the United States since 2006. It is listed on the Food and Drug Administration’s Discontinued Drug Product List.
Rocuronium bromide
Like mivacurium, rocuronium was developed as an alternative to succinylcholine for intubation in human patients because of its rapid onset of action. In halothane-anesthetized dogs, rocuronium had an onset and duration of action of 1.1 ± 0.49 and 13.7 ± 0.49 minutes, respectively.24 Rocuronium lacks significant cardiovascular and histamine-releasing effects.25 It is metabolized primarily by the liver, with a small fraction eliminated by the kidney.26 In small animal anesthesia, rocuronium may be chosen if a rapid onset of action without significant hemodynamic effects is desired.
Doxacurium chloride
Doxacurium is the most potent nondepolarizing agent available for use at this time.19 It is a long-acting muscle relaxant with a slow onset of action and long duration of action in human patients. Doxacurium has minimal cardiovascular or histamine-releasing effects.27 Because metabolism is through renal elimination, a prolonged or more variable duration of action is seen in patients with renal disease.28 Doxacurium is not commonly used in veterinary medicine. Becaue of its long duration of action, doxacurium may not be suitable for routine clinical use in small animal patients, but it may be an attractive choice for researchers when long-term relaxation with minimal hemodynamic effects is desired.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree