Chapter 7 Movement
Gait
Determination, Grading, and Characterization of Lameness
2 Possibility of involvement of more than one limb and presence of compensatory (coexistent) lameness
Compensatory Lameness
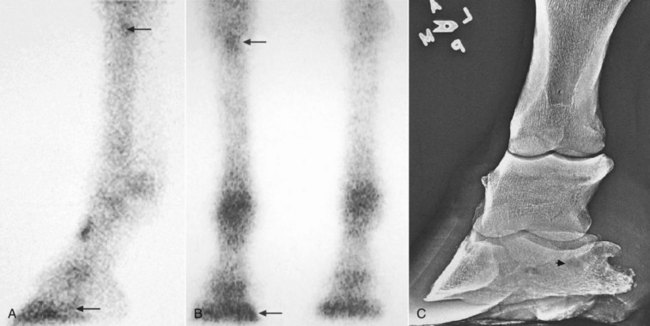
Compensatory lameness also can develop in the same limb. In horses with front foot lameness the suspensory ligament (SL) often is sore, and some horses have suspensory desmitis. In horses with lameness abolished by palmar digital analgesia, most with navicular syndrome, scintigraphic examination revealed increased radiopharmaceutical uptake (IRU) in the proximal palmar aspect of the McIII in 30% of horses, indicating possible abnormal loading of the proximal aspect of the SL (Figure 7-1).9 Complete resolution of lameness may not be achieved until high palmar analgesia is performed.