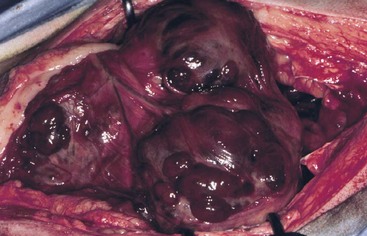
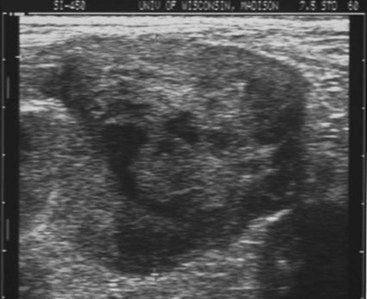
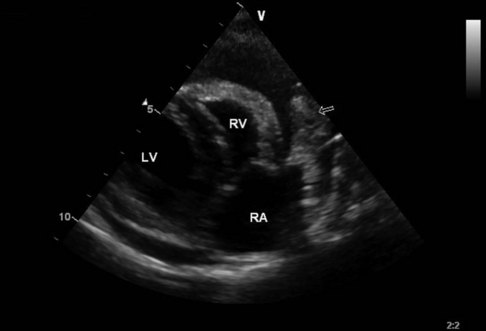
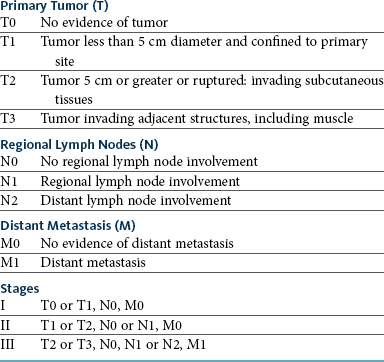
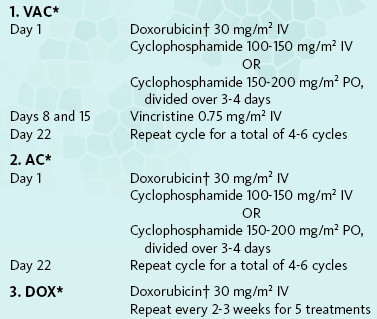
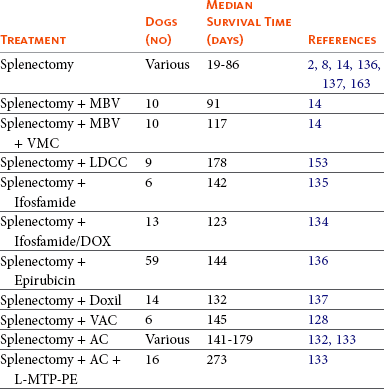
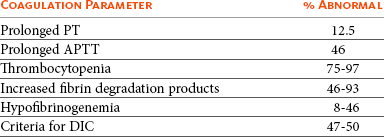
33 Hemangiosarcoma (HSA), also known as malignant hemangioendothelioma or angiosarcoma, is a malignant neoplasm of vascular endothelial origin. HSA occurs more frequently in dogs than in any other species.1,2 It represents about 5% of all noncutaneous primary malignant neoplasms and 12% to 21% of all mesenchymal neoplasms in the dog.3–5 HSA accounts for 2.3% to 3.6% of skin tumors in dogs1,6 and 45% to 51% of splenic malignancies.2,7,8 It is less common in the cat, occurring in approximately 0.5% of cats examined at necropsy in one study and accounting for 2% of all neoplasms in another.9,10 HSA is seen mostly in middle-aged to older animals, although there are reports in dogs less than 3 years of age.7,10–14 German shepherds, golden retrievers, and Labrador retrievers are overrepresented in many case series.7,11,14–16 There may be a slight male predisposition in dogs.11,12,14,15,17 Although the etiology is unknown, reports in humans have been related to exposure to thorium dioxide, arsenicals, vinyl chloride, and androgens.18 It is reported as a rare late sequela to breast-conserving irradiation in humans with breast cancer.19 The human vascular neoplasm Kaposi’s sarcoma is causally associated with human herpesvirus 8, and although some studies have demonstrated herpesviral elements in human angiosarcoma as well, the majority have not.20–23 There is a documented increase in HSA development in dogs exposed to ionizing radiation prenatally or postnatally.24 Cutaneous HSAs are found more frequently in dogs with minimal pigmentation and thin hair coats25 and have been associated with ultraviolet light exposure in laboratory dogs.26 There is increasing evidence that dysregulation of molecular pathways governing angiogenesis may be important in the pathogenesis of HSA. Studies in humans and dogs have demonstrated abundant expression of angiogenic growth factors such as vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and angiopoietins-1 and -2 (Ang-1 and -2) in HSA cells and tissues and concomitant expression of the cellular receptors for VEGF, bFGF, and Ang-1.27–36 This suggests the potential for autocrine stimulation of one or more of these receptors leading to dysregulated proliferation and survival. Indeed, enforced overexpression of VEGF is sufficient to transform immortalized murine endothelial cells into HSA,37 and in vivo overexpression of VEGF has led to vascular tumor formation in mice.38 Mutations in tumor suppressor genes such as p53,39,40 Ras,41–43 and Tsc244 have likewise been implicated in the pathogenesis of HSA, based on murine or human studies. Recent studies suggest that p53 and Ras mutations are infrequent in canine HSA45–47; however, PTEN inactivation was demonstrated in greater than 50% of evaluated canine HSA samples in one study.48 Key growth- and apoptosis-regulating proteins such as pRB, cyclin D1, BCL2, and survivin appear overexpressed in HSA when compared with hemangiomas or normal tissues.46,49 Gene expression profiling studies indicate an enrichment for genes involved in inflammation and angiogenesis.47 In the dog, the most common primary site for HSA is the spleen.1,11,12,14,15 Other frequent sites include the right atrium, skin and subcutis, and liver.11,14,25,50–53 Occurrence has also been reported in the lung, kidney, oral cavity, muscle, bone, urinary bladder, left ventricle, uterus, tongue, digit, and retroperitoneum.12,14,54–60 In the cat, cutaneous and visceral (e.g., spleen, liver, intestine) locations are evenly distributed.10,61 Other reported sites in the cat include the heart, thoracic cavity, eyelid, and nasal cavity.10,53,61–64 HSA is the most common splenic neoplasm encountered but is by no means the only differential for splenomegaly or splenic masses in dogs. The “double two-thirds rule” has been applied to canine splenic masses: approximately two-thirds of dogs with splenic masses will have a malignant tumor, and approximately two-thirds of those malignancies will be HSA2,8,17,65; however, recent studies have found that 63% to 70% of dogs with splenic masses presenting with nontraumatic hemoabdomen were HSA.66–68 Several splenic mass lesions (e.g., HSA, hematoma, hemangioma) can have a similar gross and ultrasonographic appearance, and large masses do not necessarily denote malignancy.69 Histopathology is necessary to establish a definitive diagnosis in these cases. HSA may be solitary, multifocal within an organ, or widely disseminated at presentation. Grossly, they are of variable size, pale gray to dark red or purple, and soft or gelatinous, often containing blood-filled or necrotic areas on cut surface (Figure 33-1). They are poorly circumscribed, nonencapsulated, and often adhered to adjacent organs. They are extremely friable, and complications associated with rupture and hemorrhage are frequent presenting complaints. Histologically, HSA consists of immature, pleomorphic endothelial cells forming vascular spaces containing variable amounts of blood and/or thrombi.70,71 When such features are minimal but HSA is suspected, immunohistochemistry for von Willebrand’s factor (factor VIII–related antigen) or CD31/platelet endothelial cell-adhesion molecule (PECAM) can be used to demonstrate endothelial derivation and support the diagnosis of HSA.71–74 Recently, claudin-5 and CD117 (KIT) have also been identified as potentially useful immunohistochemical markers for distinguishing canine tumors of vascular endothelial origin.75,76 Perhaps owing to its intimate association with the vasculature, facilitating extravasation and angiogenesis of metastatic clones, canine HSA is typified by very aggressive biologic behavior, with rapid and wide metastasis occurring frequently. An exception to this rule is pure cutaneous or dermal HSA, without any clinical or histologic evidence of subdermal infiltration.51 Metastasis is typically hematogenous or through transabdominal implantation following rupture. The most frequent metastatic sites are the liver, omentum, mesentery, and lungs.14,77 One study suggested that approximately, 25% of dogs with splenic HSA will also have right atrial involvement.77 However, the experience of the author suggests that this percentage at initial presentation is significantly lower (5% or less). Other reported sites of metastasis are the kidney, muscle, peritoneum, lymph nodes, adrenal gland, brain, and diaphragm. In dogs, HSA is considered the most common metastatic tumor to the brain.78,79 HSA in cats is considered to be a less aggressive disease. Cutaneous or subcutaneous HSA often behaves in a fashion similar to other soft tissue sarcomas, and local recurrence is the major concern.72,80,81 Reports do exist of more aggressive biologic behavior in a subset of cats with cutaneous HSA, however.80–82 Visceral HSAs have a higher metastatic rate, similar to that in dogs, and the common sites include the liver, omentum, diaphragm, pancreas, and lung.10,61,81,83,84 In the cat, signs will depend on location and extent of tumor. Cats with visceral tumors usually have a history of lethargy, anorexia, vomiting, sudden collapse, dyspnea, or a distended abdomen.61,81,83 On physical examination, pallor, pleural or peritoneal fluid, and a palpable abdominal mass may be detected. In both dogs and cats, anemia is often seen, usually characterized by the presence of schistocytes (associated with microangiopathic hemolysis) and acanthocytes in the peripheral blood.* Anemia may be regenerative or nonregenerative, depending on duration. Blood typing and/or crossmatching may be indicated if surgery is planned in a severely anemic patient. In addition, a neutrophilic leukocytosis may be seen.61,66 Thrombocytopenia is observed in 75% to 97% of cases, ranging from mild to severe.66,67,86,87 Serum biochemistry changes are typically nonspecific and can include hypoalbuminemia, hypoglobulinemia, and mild elevations in liver enzymes.66,83 A coagulogram is very useful in animals with suspected HSA. Perturbations in some aspect of the coagulation cascade (prothrombin time [PT], activated partial thromboplastin time [APTT], platelet count, activated clotting time, fibrinogen concentration, fibrin degradation products) are seen in the majority of patients (Table 33-1)66,86–91 and approximately 50% have coagulation abnormalities that meet the criteria for disseminated intravascular coagulation (DIC).86,88 Tumor vasculature, especially in the case of HSA, differs significantly from normal vasculature, commonly containing blind-ended or irregular tortuous vessels, incomplete endothelial lining, arteriovenous shunts, exposed subendothelial collagen, and platelet-tumor aggregates.92 HSA-derived endothelial cells may also have an “activated” phenotype, further promoting initiation of the coagulation cascade. Table 33-1 Coagulation Abnormalities in Dogs with Hemangiosarcoma Data from Pintar J, Breitschwerdt EB, Hardie EM, et al: Acute nontraumatic hemoabdomen in the dog: a retrospective analysis of 39 cases (1987-2001), J Am Anim Hosp Assoc 39:518–522, 2003; Hammer AS, Couto CG, Swardson C, et al: Hemostatic abnormalities in dogs with hemangiosarcoma, J Vet Intern Med 5:11–14, 1991; Hargis AM, Feldman BF: Evaluation of hemostatic defects secondary to vascular tumors in dogs: 11 cases, J Am Vet Med Assoc 198:891–894, 1991; Maruyama H, Miura T, Sakai M, et al: The incidence of disseminated intravascular coagulation in dogs with malignant tumor, J Vet Med Sci 66:573–575, 2004; Mischke R, Wohlsein P, Schoon HA: Detection of fibrin generation alterations in dogs with haemangiosarcoma using resonance thrombography, Thromb Res 115:229–238, 2005; Rishniw M, Lewis DC: Localized consumptive coagulopathy associated with cutaneous hemangiosarcoma in a dog, J Am Anim Hosp Assoc 30:261–264, 1994; Maruyama H, Watari T, Miura T, et al: Plasma thrombin-antithrombin complex concentrations in dogs with malignant tumours, Vet Rec 156:839–840, 2005. Screening for metastasis is mandatory prior to definitive surgery for HSA. Dogs with gross evidence of metastasis have a grave prognosis, and surgery is purely palliative. Thoracic radiographs should be obtained in all cases. One study reported a 78% sensitivity and 74% negative predictive value for detecting pulmonary manifestations of HSA, and obtaining three views significantly decreased the false-negative rate.93 Dogs with hemopericardium secondary to cardiac HSA will typically have a globoid cardiac silhouette, with or without distension of the caudal vena cava.94 Abdominal radiographs may reveal a cranial abdominal mass in many cases; however, abdominal ultrasound is a superior modality for imaging the abdomen. Many animals with visceral HSA will have ascites, which diminishes abdominal detail with radiographs but not ultrasound. Ultrasound also allows for the more thorough evaluation of the rest of the abdomen for evidence of metastatic disease. HSA typically has a heteroechoic appearance, ranging from anechoic/cavitated to hyperechoic, or a targetoid appearance (Figure 33-2).95,96 Typical electrocardiographic signs consistent with pericardial effusion (decreased amplitude QRS complex, electrical alternans) can be seen in dogs with cardiac HSA and hemopericardium. Echocardiography can be useful in dogs with suspected pericardial effusion, and a right atrial mass may be visible in 65% to 90% of cases (Figure 33-3)97–100; however, some dogs may develop blood clots within the pericardium that can have a mass effect. Thus the absence of a mass does not rule out HSA, and the presence of a mass is not pathognomonic. Despite this, detection of a mass on echocardiography is strongly associated with a worse prognosis in dogs with pericardial effusion.94,99 Other negative prognostic factors include history of collapse and presence of ascites.94 Routine evaluation of the heart for metastatic disease in a dog with subcutaneous or visceral HSA without evidence of other metastasis is rarely rewarding. A clinical staging system for HSA is given in Table 33-2. Ultimately, a definitive diagnosis of HSA usually requires a surgical biopsy. Needle aspiration cytology of suspicious masses, although simple and cost-effective, is of low diagnostic utility due to the hemodilution that usually accompanies sampling.101 Needle core biopsies can be obtained of cutaneous or subcutaneous lesions but should not be performed on suspect visceral lesions due to the risk of induction of hemorrhage and subsequent seeding of the peritoneum. If only small samples of suspected HSA are submitted, histopathology may only reveal blood clots or other nonspecific findings. Submission of large samples of suspected HSA is preferred to maximize the likelihood of capturing a true tumor if present. This includes submission of entire spleens whenever possible or, at the very least, numerous parts of the mass. Several investigators are evaluating additional tests, which may allow more accurate presurgical diagnosis. Pericardial fluid pH was suggested to correlate with presence or absence of neoplasia in one study102; however, subsequent studies have shown pericardial fluid analysis to be of little diagnostic benefit.103,104 Recent studies have found a significant difference in concentrations of troponin I, an indicator of myocardial damage, between dogs with cardiac HSA and dogs with idiopathic pericardial effusions.105,106 Plasma concentrations of VEGF and urine concentrations of bFGF are elevated in dogs with HSA versus normal controls27,28; however, neither was found to correlate with remission status, disease stage, or outcome. Advanced imaging techniques such as contrast-enhanced ultrasound,107–113 contrast-enhanced computed tomography (CT),114 and magnetic resonance imaging (MRI)115 have been useful in discriminating malignant versus benign lesions in preliminary studies. Additional blood-based biomarkers showing early promise include measurement of serum alpha-1 acid glycoprotein,116 lipocalin region of collagen XXVII alpha 1,117 and thymidine kinase activity,118,119 as well as multiparameter flow cytometry of peripheral blood utilizing a variety of endothelial and primitive hematopoietic cell markers.120 For cutaneous or subcutaneous HSA, surgical considerations are similar to those for other soft-tissue sarcomas (see Chapter 21). Dermal HSA is usually discrete, and surgical margins of 1 to 2 cm are often adequate. Intramuscular HSA will often present with a large blood clot admixed with actual tumor. Wide margins can be difficult to achieve, short of limb amputation when possible. Debulking may provide short-term relief. For splenic HSA, splenectomy is required and can be performed with sutures, staples, or electrothermal vessel sealant devices (e.g., LigaSure Force Triad, Covidien, Mansfield, MA).121 The spleen should be carefully delivered from the abdomen to avoid iatrogenic rupture. Attached omentum should be removed en bloc. Intraoperative autotransfusion of blood has been described but requires specialized equipment and personnel and still remains controversial.122 At the time of splenectomy, the abdomen should be thoroughly explored and any suspicious lesions in the liver or omentum, especially if actively bleeding, should be excised and submitted for histopathology. Biopsy of grossly normal livers is probably not useful. The abdomen should be thoroughly lavaged and instruments changed prior to closure to minimize the risk of abdominal/wound bed or suture line seeding. Dogs undergoing splenectomy are prone to develop ventricular arrhythmias following surgery. In one study of 59 dogs, 24% developed arrhythmias.123 Poor myocardial perfusion secondary to hypoxia, hypovolemia, or anemia or a neurohormonal response associated with manipulation of the spleen are all potential causes. An electrocardiogram should be monitored intraoperatively and in the postoperative period, and arrhythmias treated as they arise. Arrhythmias usually resolve within 24 to 48 hours. Surgery can be performed for primary cardiac HSA. An open or thoracoscopic pericardiectomy can be used as a palliative procedure, allowing effusion to escape into the thorax rather than accumulating in the pericardium, where a small volume can readily restrict function. Right atrial appendage masses can be resected with a stapling device or hand stitching,124,125 and reconstructive procedures have been described in cases where extensive resection is required.126,127 A recent retrospective study suggests that dogs surviving the perioperative period have a prognosis similar to dogs with HSA of other visceral sites.125 Given the very high metastatic rate of most canine HSA and the poor outcome associated with surgery alone (see later), adjuvant chemotherapy is indicated in all cases, with the exception of pure cutaneous tumors. Single-agent and combination doxorubicin (DOX)-based chemotherapy protocols are most frequently used (Box 33-1).128–134 Other combinations such as vincristine, cyclophosphamide, and methotrexate (VCM) have yielded only modest improvements in survival time.14 Recently, ifosfamide was shown to also have some modest antitumor activity in canine HSA.134,135 Both epirubicin and liposome-encapsulated DOX appear to have roughly equivalent activity to conventional DOX.136,137 In cats, similar DOX-based protocols are employed, although reports of systematic evaluations are lacking. For cases in which surgery is declined or impossible due to size/location or presence of metastasis, DOX-based chemotherapy induces meaningful tumor regression in a large minority of animals138–140; however, remissions are typically incomplete and brief in duration. Isolated reports of antitumor activity have been reported with carboplatin as well.141 Very few studies have been conducted to evaluate biologic therapy for HSA (see Chapter 13). One study used a mixed killed bacterial vaccine following surgery and showed some improvement in survival time in dogs with splenic HSA.14 More recently, a surgical adjuvant study was conducted in dogs with splenic HSA to compare chemotherapy (DOX and cyclophosphamide) to the same chemotherapy combined with immunotherapy using liposome-encapsulated muramyl tripeptide-phosphatidylethanolamine (L-MTP-PE). The median survival time (MST) for those dogs treated with chemotherapy alone was 5.7 months versus 9.1 months (p = 0.03) for those treated with L-MTP-PE and chemotherapy, with 40% of dogs in the L-MTP-PE group experiencing long-term survival.133 L-MTP-PE is currently unavailable in the United States but has been granted orphan drug status for the treatment of pediatric osteosarcoma in the European Union. Investigations of allogeneic tumor cell vaccine approaches in combination with chemotherapy have shown initial promise in small numbers of dogs.142 Radiation therapy (RT) is rarely utilized for HSA due to the anatomic sites involved and high metastatic rate. Coarsely fractionated (palliative) RT for peripheral masses (e.g., cutaneous and subcutaneous lesions) may dramatically decrease local disease but may not significantly impact overall survival.143–145 It is conceivable that a combination of palliative RT and chemotherapy may provide better control, but this awaits further investigation. Full-course (definitive) RT may be reasonable for dogs with incompletely resected, solitary dermal HSA or feline nonvisceral HSA due to their reduced potential for metastasis. Given the endothelial derivation of HSA, therapy directed against angiogenesis is a logical avenue of exploration, and murine HSA has been used as a model for the evaluation of novel antiangiogenic strategies. Antitumor activity has been seen in a murine HSA model to a variety of antiangiogenic treatments, such as VEGF receptor kinase inhibitors,146 TNP-470,147 and several others,148–150 and objective responses have been observed with several angiogenic receptor tyrosine kinase inhibitors in human reports.151,152 Interleukin-12 (IL-12) has been shown to retard tumor growth in a canine HSA xenograft as well.33 A small pilot study recently reported the outcome following treatment of dogs with splenic HSA with a combination of splenectomy, a nonsteroidal antiinflammatory drug (NSAID), and low-dose continuous (metronomic) chemotherapy with alternating courses of cyclophosphamide and etoposide. Outcome was similar to what has been reported following DOX-based injectable chemotherapy.153 In humans with various vascular tumors, antitumor activity has been observed following the local administration of IL-2,154,155 and the local or systemic administration of interferon-α (IFNα) in combination with traditional cytotoxics.156–159 Additionally, paclitaxel, docetaxel, and gemcitabine appear to have activity against human HSA.157,160–162 A summary of the results of several reports on the treatment of splenic HSA is presented in Table 33-3. Overall, the prognosis for dogs with splenic HSA treated by surgery alone is extremely poor. MSTs for splenic HSA range from 19 to 86 days, and less than 10% survive to 12 months.2,8,14,163,164 Primary hepatic HSA is thought to carry an equally poor prognosis. In contrast, one study suggests that dogs with primary renal HSA may have a more favorable outcome than those with HSA of other visceral sites.60 Surgery plus anthracycline-based chemotherapy following surgery will increase median survival times to 141 to 179 days.* Even with the addition of chemotherapy, the 12-month survival percentage is 10% or less. In one report, the addition of immunotherapy (L-MTP-PE) to standard chemotherapy increased median survival time to 273 days.133 In splenic HSA, stage I (nonruptured) tumors may have a more favorable outcome than stage II (ruptured) tumors when postoperative chemotherapy is used.14,130,133 One study employed a histologic grading scheme, and demonstrated that dogs with low-grade tumors had a better prognosis than dogs with intermediate- or high-grade tumors.129 In a study of surgically treated cutaneous HSA, tumors involving the dermis (without subdermal invasion) had a MST of 780 days (n = 10).51 Tumors with invasion into the subcutaneous tissues or muscle generally have worse outcomes than those confined to the dermis.11,51,165,166 Therefore adjuvant medical therapy should be offered for subcutaneous or intramuscular HSA, although reports regarding efficacy are divergent.165,166 Overall, the prognosis is poor for cardiac HSA. In dogs undergoing surgery for right atrial HSA, the average survival time ranges from 1 to 4 months.99,124 A recent study reported an outcome following surgery and chemotherapy roughly equivalent to that reported for HSA of the spleen.125 In cats, the prognosis for visceral HSA is poor. Most cats die from recurrence of the primary tumor or metastasis, and MSTs are generally short, owing to metastasis.61,84 HSAs located in cutaneous and subcutaneous sites have recurrence rates of 60% to 80%,61,72 although one recent case series reported a favorable outcome following aggressive surgery, and complete excision is associated with improvement in outcome.80,81 Metastasis can develop following surgical resection in some cases, although the frequency is unknown.82 In humans, a spectrum of endothelial tumors, including hemangioma, hemangioblastoma, Kaposi’s sarcoma, hemangioendothelioma, and angiosarcoma, is seen. Angiosarcoma is extremely rare in humans and can be a late sequela to RT in women treated for breast cancer.167 With this exception, it has a lesion distribution and behavior similar to canine HSA. As in dogs, metastasis is frequent and adjuvant chemotherapy provides minimal benefit. 1. Priester, W, McKay, F. The occurrence of tumors in domestic animals. Washington, DC: National Cancer Institute Monograph; 1980. 2. Spangler, WL, Culbertson, MR. Prevalence, type, and importance of splenic diseases in dogs: 1,480 cases (1985-1989). J Am Vet Med Assoc. 1992;200:829–834. 3. Bastianello, SS. A survey on neoplasia in domestic species over a 40-year period from 1935 to 1974 in the republic of South Africa. VI. Tumors occurring in dogs. Onderspoort J Vet Res. 1983;50:199–220. 4. Dorn, CR, Taylor, DON, Schneider, R, et al. Survey of animal neoplasms in Alameda and Contra Costa Counties. Cancer morbidity in dogs and cats from Alameda County. J Natl Cancer Inst. 1968;40:307–318. 5. MacVean, DW, Monlux, AW, Anderson, PS, et al. Frequency of canine and feline tumors in a defined population. Vet Pathol. 1978;145:700–715. 6. Rostami, M, Tateyama, S, Uchida, K, et al. Tumor in domestic animals examined during a ten-year period (1980 to 1989) at Miyazaki University. J Vet Med Sci. 1991;56:403–405. 7. Day, MJ, Lucke, VM, Pearson, H. A review of pathological diagnoses made from 87 canine splenic biopsies. J Small Anim Pract. 1995;36:426–433. 8. Spangler, WL, Kass, PH. Pathologic factors affecting postsplenectomy survival in dogs. J Vet Intern Med. 1997;11:166–171. 9. Carpenter, JL, Andrews, LK, Holzworth, J. Tumors and tumor-like lesions. In: Holzworth J, ed. Diseases of the cat: medicine and surgery. Philadelphia: WB Saunders, 1987. 10. Patnaik, AK, Liu, SK. Angiosarcoma in cats. J Small Anim Pract. 1977;18:191–198. 11. Schultheiss, PC. A retrospective study of visceral and nonvisceral hemangiosarcoma and hemangiomas in domestic animals. J Vet Diagn Invest. 2004;16:522–526. 12. Oksanen, A. Haemangiosarcoma in dogs. J Comp Pathol. 1978;88:585–595. 13. Arp, LH, Grier, RL. Disseminated cutaneous hemangiosarcoma in a young dog. J Am Vet Med Assoc. 1984;185:671–673. 14. Brown, NO, Patnaik, AK, MacEwen, EG. Canine hemangiosarcoma: retrospective analysis of 104 cases. J Am Vet Med Assoc. 1985;186:56–58. 15. Srebernik, N, Appleby, EC. Breed prevalence and sites of haemangioma and haemangiosarcoma in dogs. Vet Rec. 1991;129:408–409. 16. Moe, L, Gamlem, H, Dahl, K, et al, Canine neoplasia–population-based incidence of vascular tumours. APMIS Suppl 2008:63–68. 17. Gamlem, H, Nordstoga, K, Arnesen, K. Canine vascular neoplasia–a population-based clinicopathologic study of 439 tumours and tumour-like lesions in 420 dogs. APMIS. 2008;Suppl:41–54. 18. Falk, H, Herbert, J, Crowley, S, et al. Epidemiology of hepatic angiosarcoma in the United States: 1964-1974. Environ Health Perspect. 1981;41:107–113. 19. Weaver, J, Billings, SD. Postradiation cutaneous vascular tumors of the breast: a review. Semin Diagn Pathol. 2009;26:141–149. 20. Gessi, M, Cattani, P, Maggiano, N, et al. Demonstration of human herpesvirus 8 in a case of primary vaginal epithelioid angiosarcoma by in situ hybridization, electron microscopy, and polymerase chain reaction. Diagn Mol Pathol. 2002;11:146–151. 21. Remick, SC, Patnaik, M, Ziran, NM, et al. Human herpesvirus-8-associated disseminated angiosarcoma in an HIV-seronegative woman: report of a case and limited case-control virologic study in vascular tumors. Am J Med. 2000;108:660–664. 22. Fink-Puches, R, Zochling, N, Wolf, P, et al. No detection of human herpesvirus 8 in different types of cutaneous angiosarcoma. Arch Dermatol. 2002;138:131–132. 23. Palacios, I, Umbert, I, Celada, A. Absence of human herpesvirus-8 DNA in angiosarcoma. Br J Dermatol. 1999;140:170–171. 24. Benjamin, SA, Lee, AC, Angleton, GM, et al. Mortality in beagles irradiated during prenatal and postnatal development. II. Contribution of benign and malignant neoplasia. Radiat Res. 1998;150:330–348. 25. Hargis, AM, Ihrke, PJ, Spangler, WL, et al. A retrospective clinicopathologic study of 212 dogs with cutaneous hemangiomas and hemangiosarcomas. Vet Pathol. 1992;29:316–328. 26. Nikula, KJ, Benjamin, SA, Angleton, GM, et al. Ultraviolet radiation, solar dermatosis, and cutaneous neoplasia in beagle dogs. Radiat Res. 1992;129:11–18. 27. Clifford, CA, Hughes, D, Beal, MW, et al. Plasma vascular endothelial growth factor concentrations in healthy dogs and dogs with hemangiosarcoma. J Vet Intern Med. 2001;15:131–135. 28. Duda, LE, Sorenmo, KU, Urine basic fibroblast growth factor in canine hemangiosarcoma. 73, Chicago. Proceedings of the Veterinary Cancer Society Annual Conference 1997 . 29. Amo, Y, Masuzawa, M, Hamada, Y, et al. Observations on angiopoietin 2 in patients with angiosarcoma. Br J Dermatol. 2004;150:1028–1029. 30. Brown, LF, Tognazzi, K, Dvorak, HF, et al. Strong expression of kinase insert domain-containing receptor, a vascular permeability factor/vascular endothelial growth factor receptor in AIDS-associated Kaposi’s sarcoma and cutaneous angiosarcoma. Am J Pathol. 1996;148:1065–1074. 31. Hashimoto, M, Oshawa, N, Ohnishi, A, et al. Expression of vascular endothelial growth factor and its receptor mRNA in angiosarcoma. Lab Invest. 1995;73:859–863. 32. Yamamoto, T, Umeda, T, Yokozeki, H, et al. Expression of basic fibroblast growth factor and its receptor in angiosarcoma. J Am Acad Dermatol. 1999;41:127–129. 33. Akhtar, N, Padilla, ML, Dickerson, EB, et al. Interleukin-12 inhibits tumor growth in a novel angiogenesis canine hemangiosarcoma xenograft model. Neoplasia. 2004;6:106–116. 34. Fosmire, SP, Dickerson, EB, Scott, AM, et al. Canine malignant hemangiosarcoma as a model of primitive angiogenic endothelium. Lab Invest. 2004;84:562–572. 35. Yonemaru, K, Sakai, H, Murakami, M, et al. Expression of vascular endothelial growth factor, basic fibroblast growth factor, and their receptors (flt-1, flk-1, and flg-1) in canine vascular tumors. Vet Pathol. 2006;43:971–980. 36. Kodama, A, Sakai, H, Matsuura, S, et al. Establishment of canine hemangiosarcoma xenograft models expressing endothelial growth factors, their receptors, and angiogenesis-associated homeobox genes. BMC Cancer. 2009;9:363. 37. Arbiser, JL, Larsson, H, Claesson-Welsh, L, et al. Overexpression of VEGF 121 in immortalized endothelial cells causes conversion to slowly growing angiosarcoma and high level expression of the VEGF receptors VEGFR-1 and VEGFR-2 in vivo. Am J Pathol. 2000;156:1469–1476. 38. Lee, RJ, Springer, ML, Blanco-Bose, WE, et al. VEGF gene delivery to myocardium: deleterious effects of unregulated expression. Circulation. 2000;102:898–901. 39. Donehower, LA, Harvey, M, Slagle, BL, et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature. 1992;356:215–221. 40. Naka, N, Tomita, Y, Nakanashi, H, et al. Mutations of p53 tumor-suppressor gene in angiosarcoma. Int J Cancer. 1997;71:952–955. 41. Arbiser, JL, Moses, MA, Fernandez, CA, et al. Oncogenic H-ras stimulates tumor angiogenesis by two distinct pathways. Proc Natl Acad Sci USA. 1997;94:861–866. 42. DeVivo, I, Marion, MJ, Smith, SJ, et al. Mutant c-Ki-ras p21 protein in chemical carcinogenesis in humans exposed to vinyl chloride. Cancer Causes Control. 1994;5:273–278. 43. Garcia, JM, Gonzalez, R, Silva, JM, et al. Mutational status of K-ras and TP53 genes in primary sarcomas of the heart. Br J Cancer. 2000;82:1183–1185. 44. Onda, H, Lueck, A, Marks, PW, et al. Tsc2(+/−) mice develop tumors in multiple sites that express gelsolin and are influenced by genetic background. J Clin Invest. 1999;104:687–695. 45. Mayr, B, Zwetkoff, S, Schaffner, G, et al. Tumour suppressor gene p53 mutation in a case of haemangiosarcoma of a dog. Acta Vet Hung. 2002;50:157–160. 46. Yonemaru, K, Sakai, H, Murakami, M, et al. The significance of p53 and retinoblastoma pathways in canine hemangiosarcoma. J Vet Med Sci. 2007;69:271–278. 47. Tamburini, BA, Phang, TL, Fosmire, SP, et al. Gene expression profiling identifies inflammation and angiogenesis as distinguishing features of canine hemangiosarcoma. BMC Cancer. 2010;10:619. 48. Dickerson, EB, Thomas, R, Fosmire, SP, et al. Mutations of phosphatase and tensin homolog deleted from chromosome 10 in canine hemangiosarcoma. Vet Pathol. 2005;42:618–632. 49. Murakami, M, Sakai, H, Kodama, A, et al. Expression of the anti-apoptotic factors Bcl-2 and survivin in canine vascular tumours. J Comp Pathol. 2008;139:1–7. 50. Priester, WA. Hepatic angiosarcomas in dogs: an excessive frequency as compared with man. J Natl Cancer Inst. 1976;57:451–454. 51. Ward, H, Fox, LE, Calderwood-Mays, MB, et al. Cutaneous hemangiosarcoma in 25 dogs: a retrospective study. J Vet Intern Med. 1994;8:345–348. 52. Ware, WA, Hopper, DL. Cardiac tumors in dogs: 1982-1995. J Vet Intern Med. 1999;13:95–103. 53. Aupperle, H, Marz, I, Ellenberger, C, et al. Primary and secondary heart tumours in dogs and cats. J Comp Pathol. 2007;136:18–26. 54. Erdem, V, Pead, J. Haemangiosarcoma of the scapula in three dogs. J Small Anim Pract. 2000;41:461–464. 55. Liptak, JM, Dernell, WS, Ehrhart, EJ, et al. Retroperitoneal sarcomas in dogs: 14 cases (1992-2002). J Am Vet Med Assoc. 2004;224:1471–1477. 56. Liptak, JM, Dernell, WS, Withrow, SJ. Haemangiosarcoma of the urinary bladder in a dog. Aust Vet J. 2004;82:215–217. 57. Pirkey-Ehrhart, N, Withrow, SJ, Straw, RC, et al. Primary rib tumors in 54 dogs. J Am Anim Hosp Assoc. 1995;31:65–69. 58. Wobeser, BK, Kidney, BA, Powers, BE, et al. Diagnoses and clinical outcomes associated with surgically amputated feline digits submitted to multiple veterinary diagnostic laboratories. Vet Pathol. 2007;44:362–365. 59. Dennis, MM, Ehrhart, N, Duncan, CG, et al. Frequency of and risk factors associated with lingual lesions in dogs: 1,196 cases (1995-2004). J Am Vet Med Assoc. 2006;228:1533–1537. 60. Locke, JE, Barber, LG. Comparative aspects and clinical outcomes of canine renal hemangiosarcoma. J Vet Intern Med. 2006;20:962–967. 61. Scavelli, TD, Patnaik, AK, Mehlhaff, CJ, et al. Hemangiosarcoma in the cat: retrospective evaluation of 31 surgical cases. J Am Vet Med Assoc. 1985;187:817–819. 62. Merlo, M, Bo, S, Ratto, A. Primary right atrium haemangiosarcoma in a cat. J Feline Med Surg. 2002;4:61–64. 63. Pirie, CG, Dubielzig, RR. Feline conjunctival hemangioma and hemangiosarcoma: a retrospective evaluation of eight cases (1993-2004). Vet Ophthalmol. 2006;9:227–231. 64. Newkirk, KM, Rohrbach, BW. A retrospective study of eyelid tumors from 43 cats. Vet Pathol. 2009;46:916–927. 65. Johnson, KA, Powers, BE, Withrow, SJ, et al. Splenomegaly in dogs: predictors of neoplasia and survival after splenectomy. J Vet Intern Med. 1989;3:160–166. 66. Pintar, J, Breitschwerdt, EB, Hardie, EM, et al. Acute nontraumatic hemoabdomen in the dog: a retrospective analysis of 39 cases (1987-2001). J Am Anim Hosp Assoc. 2003;39:518–522. 67. Hammond, TN, Pesillo-Crosby, SA. Prevalence of hemangiosarcoma in anemic dogs with a splenic mass and hemoperitoneum requiring a transfusion: 71 cases (2003-2005). J Am Vet Med Assoc. 2008;232:553–558. 68. Aronsohn, MG, Dubiel, B, Roberts, B, et al. Prognosis for acute nontraumatic hemoperitoneum in the dog: a retrospective analysis of 60 cases (2003-2006). J Am Anim Hosp Assoc. 2009;45:72–77. 69. Mallinckrodt, MJ, Gottfried, SD. Mass-to-splenic volume ratio and splenic weight as a percentage of body weight in dogs with malignant and benign splenic masses: 65 cases (2007-2008). J Am Vet Med Assoc. 2011;239:1325–1327. 70. Pulley, LT, Stannard, AA. Tumors of the skin and subcutaneous tissues. In Moulton JE, ed.: Tumors in domestic animals, ed 3, Berkeley: University of California Press, 1990. 71. Gamlem, H, Nordstoga, K. Canine vascular neoplasia–histologic classification and inmunohistochemical analysis of 221 tumours and tumour-like lesions. APMIS. 2008;Suppl:19–40. 72. Miller, MA, Ramos, JA, Kreeger, JM. Cutaneous vascular neoplasia in 15 cats: clinical, morphologic, and immunohistochemical studies. Vet Pathol. 1992;29:329–336. 73. von Beust, BR, Suter, MM, Summers, BA. Factor VIII-related antigen in canine endothelial neoplasms: An immunohistochemical study. Vet Pathol. 1988;25:251–255. 74. Ferrer, L, Fondevila, D, Rabanal, RM, et al. Immunohistochemical detection of CD31 antigen in normal and neoplastic canine endothelial cells. J Comp Pathol. 1995;112:319–326. 75. Jakab, C, Halasz, J, Kiss, A, et al. Claudin-5 protein is a new differential marker for histopathological differential diagnosis of canine hemangiosarcoma. Histol Histopathol. 2009;24:801–813. 76. Sabattini, S, Bettini, G. An immunohistochemical analysis of canine haemangioma and haemangiosarcoma. J Comp Pathol. 2009;140:158–168. 77. Waters, D, Caywood, D, Hayden, D, et al. Metastatic pattern in dogs with splenic hemangiosarcoma. J Small Anim Pract. 1988;29:805–814. 78. Waters, D, Hayden, D, Walter, P. Intracranial lesions in dogs with hemangiosarcoma. J Vet Intern Med. 1989;3:222–230. 79. Snyder, JM, Lipitz, L, Skorupski, KA, et al. Secondary intracranial neoplasia in the dog: 177 cases (1986-2003). J Vet Intern Med. 2008;22:172–177. 80. McAbee, KP, Ludwig, LL, Bergman, PJ, et al. Feline cutaneous hemangiosarcoma: a retrospective study of 18 cases (1998-2003). J Am Anim Hosp Assoc. 2005;41:110–116. 81. Johannes, CM, Henry, CJ, Turnquist, SE, et al. Hemangiosarcoma in cats: 53 cases (1992-2002). J Am Vet Med Assoc. 2007;231:1851–1856. 82. Kraje, AC, Mears, EA, Hahn, KA, et al. Unusual metastatic behavior and clinicopathologic findings in eight cats with cutaneous or visceral hemangiosarcoma. J Am Vet Med Assoc. 1999;214:670–672. 83. Culp, WT, Drobatz, KJ, Glassman, MM, et al. Feline visceral hemangiosarcoma. J Vet Intern Med. 2008;22:148–152. 84. Gordon, SS, McClaran, JK, Bergman, PJ, et al. Outcome following splenectomy in cats. J Feline Med Surg. 2010;12:256–261. 85. Hirsch, V, Jacobsen, J, Mills, J. A retrospective study of canine hemangiosarcoma and its association with acanthocytosis. Can Vet J. 1981;22:152–155. 86. Hammer, AS, Couto, CG, Swardson, C, et al. Hemostatic abnormalities in dogs with hemangiosarcoma. J Vet Intern Med. 1991;5:11–14. 87. Hargis, AM, Feldman, BF. Evaluation of hemostatic defects secondary to vascular tumors in dogs: 11 cases. J Am Vet Med Assoc. 1991;198:891–894. 88. Maruyama, H, Miura, T, Sakai, M, et al. The incidence of disseminated intravascular coagulation in dogs with malignant tumor. J Vet Med Sci. 2004;66:573–575. 89. Mischke, R, Wohlsein, P, Schoon, HA. Detection of fibrin generation alterations in dogs with haemangiosarcoma using resonance thrombography. Thromb Res. 2005;115:229–238. 90. Rishniw, M, Lewis, DC. Localized consumptive coagulopathy associated with cutaneous hemangiosarcoma in a dog. J Am Anim Hosp Assoc. 1994;30:261–264. 91. Maruyama, H, Watari, T, Miura, T, et al. Plasma thrombin-antithrombin complex concentrations in dogs with malignant tumours. Vet Rec. 2005;156:839–840. 92. Thamm, DH, Helfand, SC. Acquired coagulopathy III: neoplasia. In Feldman BF, Zinkl JG, Jain NC, eds.: Schalm’s veterinary hematology, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2000. 93. Holt, D, Van Winkle, T, Schelling, C, et al. Correlation between thoracic radiographs and postmortem findings in dogs with hemangiosarcoma: 77 cases (1984-1989). J Am Vet Med Assoc. 1992;200:1535–1539. 94. Stafford Johnson, M, Martin, M, Binns, S, et al. A retrospective study of clinical findings, treatment and outcome in 143 dogs with pericardial effusion. J Small Anim Pract. 2004;45:546–552. 95. Cuccovillo, A, Lamb, CR. Cellular features of sonographic target lesions of the liver and spleen in 21 dogs and a cat. Vet Radiol Ultrasound. 2002;43:275–278. 96. Wrigley, RH, Park, RD, Konde, LJ, et al. Ultrasonographic features of splenic hemangiosarcoma in dogs: 18 cases (1980-1986). J Am Vet Med Assoc. 1988;192:1113–1117. 97. Thomas, W, Sisson, D, Bauer, T, et al. Detection of cardiac masses in two-dimensional echocardiography. Vet Radiol. 1984;25:65–71. 98. Berg, RJ, Wingfield, W. Pericardial effusion in the dog: a review of 42 cases. J Am Anim Hosp Assoc. 1984;20:721–730. 99. Dunning, D, Monnet, E, Orton, EC, et al. Analysis of prognostic indicators for dogs with pericardial effusion: 46 cases (1985-1996). J Am Vet Med Assoc. 1998;212:1276–1280. 100. Fruchter, A, Miller, C, O’Grady, M. Echocardiographic results and clinical considerations in dogs with right atrial/auricular masses. Can Vet J. 1992;33:171–174. 101. Bertazzolo, W, Dell’Orco, M, Bonfanti, U, et al. Canine angiosarcoma: cytologic, histologic, and immunohistochemical correlations. Vet Clin Pathol. 2005;34:28–34. 102. Edwards, NJ. The diagnostic value of pericardial fluid pH determination. J Am Anim Hosp Assoc. 1996;32:63–67. 103. Fine, DM, Tobias, AH, Jacob, KA. Use of pericardial fluid pH to distinguish between idiopathic and neoplastic effusions. J Vet Intern Med. 2003;17:525–529. 104. Sisson, D, Thomas, WP, Ruehl, WW, et al. Diagnostic value of pericardial fluid analysis in the dog. J Am Vet Med Assoc. 1984;184:51–55. 105. Shaw, SP, Rozanski, EA, Rush, JE. Cardiac troponins I and T in dogs with pericardial effusion. J Vet Intern Med. 2004;18:322–324. 106. Chun, R, Kellihan, HB, Henik, RA, et al. Comparison of plasma cardiac troponin I concentrations among dogs with cardiac hemangiosarcoma, noncardiac hemangiosarcoma, other neoplasms, and pericardial effusion of nonhemangiosarcoma origin. J Am Vet Med Assoc. 2010;237:806–811. 107. O’Brien, RT, Iani, M, Matheson, J, et al. Contrast harmonic ultrasound of spontaneous liver nodules in 32 dogs. Vet Radiol Ultrasound. 2004;45:547–553. 108. Kutara, K, Asano, K, Kito, A, et al. Contrast harmonic imaging of canine hepatic tumors. J Vet Med Sci. 2006;68:433–438. 109. O’Brien, RT. Improved detection of metastatic hepatic hemangiosarcoma nodules with contrast ultrasound in three dogs. Vet Radiol Ultrasound. 2007;48:146–148. 110. Ohlerth, S, Dennler, M, Ruefli, E, et al. Contrast harmonic imaging characterization of canine splenic lesions. J Vet Intern Med. 2008;22:1095–1102. 111. Webster, N, Holloway, A. Use of contrast ultrasonography in the diagnosis of metastatic feline visceral haemangiosarcoma. J Feline Med Surg. 2008;10:388–394. 112. Ivancic, M, Long, F, Seiler, GS. Contrast harmonic ultrasonography of splenic masses and associated liver nodules in dogs. J Am Vet Med Assoc. 2009;234:88–94. 113. Nakamura, K, Takagi, S, Sasaki, N, et al. Contrast-enhanced ultrasonography for characterization of canine focal liver lesions. Vet Radiol Ultrasound. 2010;51:79–85. 114. Fife, WD, Samii, VF, Drost, WT, et al. Comparison between malignant and nonmalignant splenic masses in dogs using contrast-enhanced computed tomography. Vet Radiol Ultrasound. 2004;45:289–297. 115. Clifford, CA, Pretorius, ES, Weisse, C, et al. Magnetic resonance imaging of focal splenic and hepatic lesions in the dog. J Vet Intern Med. 2004;18:330–338. 116. Yuki, M, Machida, N, Sawano, T, et al. Investigation of serum concentrations and immunohistochemical localization of alpha1-acid glycoprotein in tumor dogs. Vet Res Commun. 2010;35:1–11. 117. Kirby, GM, Mackay, A, Grant, A, et al. Concentration of lipocalin region of collagen XXVII alpha 1 in the serum of dogs with hemangiosarcoma. J Vet Intern Med. 2011;25:497–503. 118. von Euler, HP, Rivera, P, Aronsson, AC, et al. Monitoring therapy in canine malignant lymphoma and leukemia with serum thymidine kinase 1 activity—evaluation of a new, fully automated non-radiometric assay. Int J Oncol. 2008;34:505–510. 119. Thamm, DH, Kamstock, DS, Sharp, CR, et al. Elevated serum thymidine kinase activity in canine splenic hemangiosarcoma. Vet Comp Oncol. 2011. [Epub ahead of print]. 120. Lamerato-Kozicki, AR, Helm, KM, Jubala, CM, et al. Canine hemangiosarcoma originates from hematopoietic precursors with potential for endothelial differentiation. Exp Hematol. 2006;34:870–878. 121. Rivier, P, Monnet, E. Use of a vessel sealant device for splenectomy in dogs. Vet Surg. 2011;40:102–105. 122. Bower, MR, Ellis, SF, Scoggins, CR, et al. Phase II comparison study of intraoperative autotransfusion for major oncologic procedures. Ann Surg Oncol. 2011;18:166–173. 123. Keyes, M, Rush, J. Ventricular arrhythmias in dogs with splenic masses. Vet Emerg Crit Care. 1994;3:33–38. 124. Aronsohn, M. Cardiac hemangiosarcoma in the dog: a review of 38 cases. J Am Vet Med Assoc. 1985;187:922–926. 125. Weisse, C, Soares, N, Beal, MW, et al. Survival times in dogs with right atrial hemangiosarcoma treated by means of surgical resection with or without adjuvant chemotherapy: 23 cases (1986-2000). J Am Vet Med Assoc. 2005;226:575–579. 126. Brisson, BA, Holmberg, DL. Use of pericardial patch graft reconstruction of the right atrium for treatment of hemangiosarcoma in a dog. J Am Vet Med Assoc. 2001;218:723–725. 127. Morges, M, Worley, DR, Withrow, SJ, et al. Pericardial free patch grafting as a rescue technique in surgical management of right atrial HSA. J Am Anim Hosp Assoc. 2011;47:224–228. 128. Hammer, AS, Couto, CG, Filppi, J, et al. Efficacy and toxicity of VAC chemotherapy (vincristine, doxorubicin, and cyclophosphamide) in dogs with hemangiosarcoma. J Vet Intern Med. 1991;5:160–166. 129. Ogilvie, GK, Powers, BE, Mallinckrodt, CH, et al. Surgery and doxorubicin in dogs with hemangiosarcoma. J Vet Intern Med. 1996;10:379–384. 130. Sorenmo, K, Duda, L, Barber, L, et al. Canine hemangiosarcoma treated with standard chemotherapy and minocycline. J Vet Intern Med. 2000;14:395–398. 131. Sorenmo, KU, Baez, JL, Clifford, CA, et al. Efficacy and toxicity of a dose-intensified doxorubicin protocol in canine hemangiosarcoma. J Vet Intern Med. 2004;18:209–213. 132. Sorenmo, KU, Jeglum, KA, Helfand, SC. Chemotherapy of canine splenic hemangiosarcoma with doxorubicin and cyclophosphamide. J Vet Intern Med. 1993;7:370–376. 133. Vail, DM, MacEwen, EG, Kurzman, ID, et al. Liposome-encapsulated muramyl tripeptide phosphatidylethanolamine adjuvant immunotherapy for splenic hemangiosarcoma in the dog: A randomized multi-institutional clinical trial. Clin Cancer Res. 1995;1:1165–1170. 134. Payne, SE, Rassnick, KM, Northrup, NC, et al. Treatment of vascular and soft-tissue sarcomas in dogs using an alternating protocol of ifosfamide and doxorubicin. Vet Comp Oncol. 2003;1:171–179. 135. Rassnick, KM, Frimberger, AE, Wood, CA, et al. Evaluation of ifosfamide for treatment of various canine neoplasms. J Vet Intern Med. 2000;14:271–276. 136. Kim, SE, Liptak, JM, Gall, TT, et al. Epirubicin in the adjuvant treatment of splenic hemangiosarcoma in dogs: 59 cases (1997-2004). J Am Vet Med Assoc. 2007;231:1550–1557. 137. Sorenmo, K, Samluk, M, Clifford, C, et al. Clinical and pharmacokinetic characteristics of intracavitary administration of pegylated liposomal encapsulated doxorubicin in dogs with splenic hemangiosarcoma. J Vet Intern Med. 2007;21:1347–1354. 138. Ogilvie, GK, Reynolds, HA, Richardson, RC, et al. Phase II evaluation of doxorubicin for treatment of various canine neoplasms. J Am Vet Med Assoc. 1989;195:1580–1583. 139. Wiley, JL, Rook, KA, Clifford, CA, et al. Efficacy of doxorubicin-based chemotherapy for non-resectable canine subcutaneous haemangiosarcoma. Vet Comp Oncol. 2010;8:221–233. 140. Dervisis, NG, Dominguez, PA, Newman, RG, et al. Treatment with DAV for advanced-stage hemangiosarcoma in dogs. J Am Anim Hosp Assoc. 2011;47:170–178. 141. Kisseberth, WC, Vail, DM, Yaissle, J, et al. Phase I clinical evaluation of carboplatin in tumor-bearing cats: a Veterinary Cooperative Oncology Group study. J Vet Intern Med. 2008;22:83–88. 142. U’Ren, LW, Biller, BJ, Elmslie, RE, et al. Evaluation of a novel tumor vaccine in dogs with hemangiosarcoma. J Vet Intern Med. 2007;21:113–120. 143. Blake, MK, LaRue, S, Withrow, SJ, Palliative radiation therapy of solid soft tissue malignancies. In Proceedings of the Veterinary Cancer Society, Estes Park, CO, 20 1988. 144. Lawrence, JA, Thamm, DH, Adams, WM, et al, Soft tissue sarcomas: a retrospective analysis of 16 dogs treated with palliative radiotherapy (1996-2001). In Proceedings of the Veterinary Cancer Society, Kansas City, MO, 19 2004. 145. Hillers, KR, Lana, SE, Fuller, CR, et al. Effects of palliative radiation therapy on nonsplenic hemangiosarcoma in dogs. J Am Anim Hosp Assoc. 2007;43:187–192. 146. Gingrich, DE, Reddy, DR, Iqbal, MA, et al. A new class of potent vascular endothelial growth factor receptor tyrosine kinase inhibitors: structure-activity relationships for a series of 9-alkoxymethyl-12-(3-hydroxypropyl)indeno[2, 1-a]pyrrolo[3,4-c]carbazole-5-ones and the identification of CEP-5214 and its dimethylglycine ester prodrug clinical candidate CEP-7055. J Med Chem. 2003;46:5375–5388. 147. Ma, G, Masuzawa, M, Hamada, Y, et al. Treatment of murine angiosarcoma with etoposide, TNP-470 and prednisolone. J Dermatol Sci. 2000;24:126–133. 148. Liekens, S, Verbeken, E, De Clercq, E, et al. Potent inhibition of hemangiosarcoma development in mice by cidofovir. Int J Cancer. 2001;92:161–167. 149. Bai, X, Cerimele, F, Ushio-Fukai, M, et al. Honokiol, a small molecular weight natural product, inhibits angiogenesis in vitro and tumor growth in vivo. J Biol Chem. 2003;278:35501–35507. 150. Ruggeri, BA, Robinson, C, Angeles, T, et al. The chemopreventive agent oltipraz possesses potent antiangiogenic activity in vitro, ex vivo, and in vivo and inhibits tumor xenograft growth. Clin Cancer Res. 2002;8:267–274.
Miscellaneous Tumors
 Section A
Section A
Hemangiosarcoma
Incidence and Risk Factors
Pathology and Natural Behavior
History and Clinical Signs
Diagnostic Techniques and Work-Up
Treatment
Chemotherapy
Immunotherapy
Radiation Therapy
Novel Therapies
Prognosis
Feline
Comparative Aspects
References
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Miscellaneous Tumors