CHAPTER 61 Miscellaneous Parasitic Diseases
TRYPANOSOMIASIS
The trypanosomes are spindle-shaped protozoal parasites, most of which propel themselves with a flagellum and undulating membrane. Infection of horses with Trypanosoma equiperdum, Trypanosoma evansi, and Trypanosoma brucei brucei has traditionally been associated with the diseases dourine, surra, and African animal trypanosomiasis (AAT), respectively. These species make up the subgenus Trypanozoon (Protozoa: Sarcomastigophora: Kinetoplastida: Trypanosomatidae).1 Differentiation of the parasite species in this subgenus on a morphologic, serologic, and molecular basis is unclear, and recent reports suggest that current species designations may ultimately prove to be incorrect.1–5
The other trypanosomes that infect horses, Trypanosoma congolense (subgenus Nannomonas) and Trypanosoma vivax (subgenus Duttonella), with T. brucei brucei, are etiologic agents of AAT. Because of the considerable confusion in nomenclature for specific trypanosomes that infect horses and the considerable overlap in clinical disease that may result from infection with these parasites, this chapter discusses the trypanosomal infections of horses as clinical syndromes (dourine, surra, and AAT) rather than individual etiologic agents.
Dourine
Etiology
Dourine is a chronic trypanosomal disease of horses that is transmitted predominantly by coitus and is characterized by genital edema, neurologic dysfunction, and death. A disease similar to dourine was described in early Arab texts4; the first mention of this disease in European literature was in 1796.6 In 1894, Rouget7 isolated T. equiperdum from the blood of an Algerian horse. Disease was later reproduced by subcutaneous inoculation of a horse with another isolate of the parasite, and the name Trypanosoma equiperdum was proposed by Doflein in 1901.8–10
Epidemiology and Pathogenesis
Historically, dourine has been present in Europe, North America, Asia, and Africa.4 After World War I, the disease was eradicated from Western Europe by serologic screening, strict sanitation, and treatment of some horses with trypanosides.4 Currently, dourine is considered a reportable disease by the World Organization for Animal Health (OIE) and is present in most of Asia, southeastern Europe, South America, and Africa. Dourine has been reported recently in Kyrgyzstan, Botswana, Lesotho, Namibia, and South Africa.2
Equids are considered the only natural host for T. equiperdum. Clinical signs are less obvious in donkeys than in horses, and these animals may be a reservoir for infection.2 Disease is not observed in zebras, although they may be seropositive by complement fixation test (CFT).2 A variety of animal species, including dogs and rabbits, may show clinical signs of disease after experimental infection with T. equiperdum. The organism is present in the urethra of infected stallions and in vaginal discharges of infected mares. Transmission in horses primarily occurs by coitus, although mechanical transmission by arthropod vectors is also possible.11,12 T. equiperdum can pass through intact mucous membranes. Transmission is considered most likely during the early stages of disease. The incubation period between exposure and initial clinical signs is highly variable; it may be as short as 1 to 2 weeks or as long as several years.11
Clinical Findings
In endemic regions, clinical signs of dourine are milder in native equids than in recently introduced breeds. The strain prevalent in southern Africa may be less virulent than the European, Asian, or North African strains, producing a very chronic, insidious disease with a long incubation period. Clinical signs may be precipitated by stress.13 The observations of geographic differences in disease severity are supported by a recent report of genetic differences between African T. equiperdum isolates and isolates from China and South America.1
The first signs of dourine in mares are vaginal discharge with edema of the vulva, perineum, mammary gland, and ventral abdomen. Some mares exhibit signs of vulvitis and vaginitis with polyuria or other signs of perineal discomfort. Abortion may occur if mares are infected with virulent strains. In stallions, initial clinical signs include edema of the external genitalia and perineum. Paraphimosis may occur.13 Cutaneous plaques, when they occur, are considered pathognomonic for dourine (“silver dollar plaques”); however, these plaques do not occur with all strains of the parasite.4 Conjunctivitis and keratitis may occur in some infected horses. Chronically infected horses develop signs of neurologic dysfunction with progressive weakness and ataxia, leading ultimately to recumbency and death. These horses usually exhibit wasting despite a good appetite and frequently have anemia. Clinical signs may wax and wane for many months or years before death, depending on the strain of infecting parasite and the host immune response.13
Diagnosis
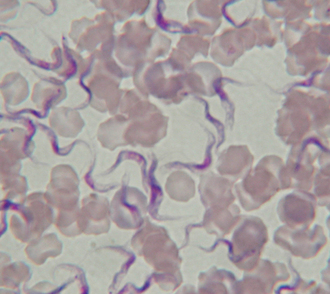
In endemic regions, the diagnosis of dourine is usually made on the basis of characteristic clinical signs. Serum, whole blood in ethylenediaminetetraacetic acid (EDTA) and blood smears from affected horses may be submitted for identification of the parasite (Fig. 61-1); however, these attempts are not often successful. The OIE-prescribed test for diagnosis of dourine is the CFT; this test does not distinguish between infection with T. equiperdum and infection with the closely related T. evansi, T. gambiense, or T. brucei.14,15 Despite this cross-reactivity, the CFT has been used effectively for the eradication of dourine in many countries, including Canada,16 Ethiopia,17 Italy,12 Morocco,18 South Africa,11,19 and Russia.20–22 Alternative serologic tests include indirect fluorescent antibody (IFA), card agglutination, agar-gel immunodiffusion (AGID), arrayed immunodiffusion, and enzyme-linked immunosorbent assays (ELISA).19,23–25
Therapy
In most situations, treatment of horses with dourine is not recommended because it may result in an inapparent carrier state.13 There are reports of treatment of affected horses with neoarsphenamine,26 suramin,27 and quinapyramine dimethylsulfate.28 Of these, neoarsphenamine and suramin have been used in large dourine eradication programs.18,21,22,29 In vitro testing suggests that T. equiperdum is also susceptible to diminazene, melarsomine, and isometamidium.30–32
Prevention and Public Health Considerations
Dourine has been successfully eradicated from many parts of the world using programs based on CFT testing. The Terrestrial Code of the OIE contains recommendations for testing and quarantine of horses imported from an endemic area into a dourine-free country. Two conditions should be met before importation of semen from a stallion that resides in a country that is not considered free of dourine: (1) the stallion should be housed for 6 months before semen collection in an establishment or artificial insemination center where no case of dourine was reported during that period, and (2) the stallion should be seronegative for T. equiperdum.
Surra
Etiology
Surra is caused by infection with the hemoparasite Trypanosoma evansi. The name is a Hindi word meaning “rotten.”33 Surra, the first pathogenic trypanosome to be discovered, was originally described by Griffith Evans, a British veterinarian, who described the condition in horses and camels in India in 1880.33 Surra is characterized by anemia, weight loss, recurrent fever, and death in a wide variety of domestic animals, including horses, cattle, buffalo, and camels, in Asia, Africa, and South America.
Epidemiology and Pathogenesis
Surra is most severe and most frequently diagnosed in horses and camels. It may also affect cattle, buffalo, llamas, dogs, cats, sheep, goats, pigs, and elephants. In some species, only occasional mild or inapparent infections are seen. The disease is seen in South America, northern Africa, the Middle East, Asia, Indonesia, and the Philippines.34,35 The etiologic agent, T. evansi, is transmitted mechanically by hematophagous biting flies of the species Tabanus and Stomoxys. Transmission by vampire bats is also possible.35 Mortality rate in horses can be quite high in areas where the disease has been newly introduced. Outbreaks of surra tend to occur in areas where there are large numbers of commingled horses, large numbers of appropriate vectors, and reservoir hosts. The incubation period after infection is approximately 1 to 2 weeks. There is no known age, breed, or gender predilection.
Clinical Findings
Horses with surra present with fever, progressive anemia, weight loss despite a good appetite, and neurologic abnormalities.36 Disease is usually acute, although some horses will experience chronic manifestations. Intermittent fever correlates with intermittent episodes of parasitemia. Urticarial lesions and edematous plaques may appear on the ventral abdomen; distal limb edema and petechial hemorrhages are common. Horses with severe anemia have pale mucous membranes. Neurologic signs, when they occur, lead to progressive weakness and ataxia, most apparent in the hindlimbs.35 Experimentally, acute infection is associated with monocytosis (up to 35%) followed by lymphocytosis.36 In an outbreak of surra on a breeding farm in Thailand, 42% of pregnant mares aborted or gave birth to stillborn foals. On this farm, 40% (19/47) of affected horses and 10% (1/10) of affected mules died.37
Diagnosis
A diagnosis of surra is suspected on the basis of compatible clinical signs in a horse residing in an area endemic for this disease. In the early stages of disease, this diagnosis is confirmed by observation of typical trypanosomes in blood or tissue fluids. This approach to diagnosis is more difficult in equids with chronic disease.38,39 Centrifugation of a blood sample and examination of the buffy coat layer may increase the sensitivity of this technique.35 Available serologic assays include ELISA, card agglutination test, and latex agglutination test. Data on their sensitivity and specificity for the field diagnosis of equine surra are largely lacking. The mouse inoculation test40 is considered the most accurate diagnostic test for surra but takes up to 6 weeks to complete and is therefore not practical for routine screening.36 The mouse inoculation test and direct review of wet blood films or buffy coat preparations are accurate for diagnosis early in disease (48 and 96 hours of infection, respectively).41,42 The reported sensitivity and specificity of other antigen detection (antigen-ELISA,39 latex agglutination43,44) and antibody detection (antibody-ELISA,39 card agglutination,45,46 IFA47) methods have varied depending on methodology and investigator.36,41,42
Therapy
Suramin is the drug that has most frequently been used for treatment of surra in horses. The recommended dose is 10 mg/kg body weight intravenously (IV), repeated 1 week later.35 Quinapyramine sulfate at 3 mg/kg has a risk of adverse local reactions, and the dose should be divided between two or more sites.35 Isometamidium chloride at 0.25 to 2 mg/kg imtramuscularly (IM)35 and melarsen oxide33 have also been suggested as treatments for surra. On a breeding farm in Thailand treatment of affected horses with diminazene aceturate at 3.5 mg/kg was initially effective in clearing T. evansi from the peripheral blood but was less effective with a second treatment. Approximately 50% of treated horses and mules showed moderate to severe signs of adverse reaction to the drug, including lip edema, salivation, recumbency, restlessness, and dyspnea.37
Prevention and Public Health Considerations
There are no vaccines for prevention of surra in horses. Prevention relies on identification and treatment of infected horses, appropriate vector control, and hygiene. Repeated treatment with antitrypanosomal medications such as suramin, quinapyramine, or isometamidium chloride has been suggested.34
There is a single report of human T. evansi infection in an Indian farmer with fluctuating parasitemia and fever who was successfully treated with suramin.48
African Animal Trypanosomiasis
Etiology
African animal trypanosomiasis (tsetse disease, tsetse fly disease, African animal nagana) is a disease complex caused by infection with Trypanosoma congolense, T. vivax, or T. brucei brucei, either singly or in combination.49–52 In East Africa, T. congolense is the most important cause of AAT. Cattle, sheep, goats, horses, and pigs develop significant clinical disease if infected. In West Africa, T. vivax is the most important cause of AAT in cattle. The polymorphic trypanosome T. brucei brucei causes significant disease in horses, dogs, cats, camels, and pigs.
Epidemiology and Pathogenesis
Infection of cattle, sheep, goats, pigs, horses, camels, dogs, cats, and monkeys with the etiologic agents of AAT results in disease that ranges from subclinical to mild to chronic to fatal.49 Numerous laboratory and wild animal species may also be infected. Wild ruminants are considered reservoirs of infection.49 In Africa, the most important biologic vectors for transmission of AAT are three species of tsetse flies: Glossina morsitans, G. palpalis, and G. fusca. Large hematophagous flies (Tabanus, Haematopa, Liperosia, Stomoxys, Chrysops) may act as mechanical vectors in some situations.49 The natural range of AAT infection is largely defined by the range of the principal vector, the tsetse fly, and includes the area from the southern edge of the Sahara desert to Angola, Zimbabwe, and Mozambique.49 Only T. vivax occurs in the Western Hemisphere (Caribbean and South and Central America), where tabanid and hippoboscid flies probably transmit the parasite mechanically.49
Trypanosomes that cause AAT replicate in the skin at the site of initial inoculation, causing a sore or chancre, and then spread to draining lymph nodes and blood. Parasitemia is detectable within a few days of experimental infection. T. congolense localizes in endothelial cells, whereas T. vivax and T. brucei brucei localize in tissues. Antibodies to the glycoprotein coat of the parasite are produced, killing the parasite and forming immune complexes with released coat protein. Parasites are not eliminated because antigenic changes in the surface coat proteins of the trypanosome occur. The result is cycles of parasitemia, antibody production, death of parasites, immune complex formation, and glycoprotein coat antigenic changes. Many of the lesions observed in animals with AAT are probably the result of immune complex disease (e.g., anemia, glomerulonephritis).49,53 Marked immunosuppression predisposes to secondary infections.
Clinical Findings
Clinical signs of AAT, regardless of the specific trypanosome involved, include anemia, intermittent fever, edema, and weight loss.49,54 Abortion and infertility may be observed. Stressors such as malnutrition or concurrent disease increase the likelihood and severity of disease. Infection with T. congolense has an incubation period that varies from 4 to 24 days; it causes severe disease in horses, cattle, sheep, goats, and camels, with milder disease in pigs. In donkeys, it may cause chronic infection with longer persistence in the blood.55 In contrast, T. vivax has an incubation period of 4 to 40 days and causes relatively mild disease in horses. Infection of horses with T. brucei brucei has a comparatively short incubation period (5-10 days) and causes severe, frequently fatal, infection of horses, camels, dogs, and cats, with mild, chronic or subclinical disease in cattle, sheep, goats, and pigs.49 Clinical signs of trypanosomiasis may be complicated by clinical signs of secondary diseases that develop as a result of immunosuppression.
Diagnosis
A diagnosis of AAT should be suspected in horses in endemic areas with anemia and poor body condition. The diagnosis is usually confirmed by demonstration of the organism in blood or lymph node smears. Parasites, especially T. vivax and T. congolense, are readily observed in whole-blood or buffy coat smears early in infection. Stained lymph node smears are most useful for diagnosis of early infection with T. vivax and T. brucei brucei or chronic T. congolense infection.49 An ELISA for detection of antigen-specific, species-specific deoxyribonucleic acid (DNA) probes for trypanosomes and polymerase chain reaction (PCR) assays to identify specific trypanosome species have been described for diagnosis of AAT in ruminants and horses.51,52,56–61
Therapy
A variety of antitrypanosomal medications have been used for the treatment and prevention of AAT; however, the development of drug resistance has complicated this approach to disease control.49,62 Quinapyramine derivatives provide effective protection against T. brucei brucei in horses for up to 3 months. Other drugs suggested for control of AAT include isometamidium chloride,62,63 homidium bromide,63 diminazene aceturate,63 and melarsen oxide; however, potential adverse effects may limit the usefulness of some of these drugs in horses.
Prevention and Public Health Considerations
The most effective way to control AAT is to control vector populations. This may include habitat manipulation (discriminative brush clearing), sterile male eradication techniques similar to those used for eradication of screwworm in the United States, ground and aerial spraying, use of synthetic pyrethroids, and odor-baited targets impregnated with insecticides.49
The trypanosomes associated with AAT are considered nonpathogenic for people.
ENTERIC COCCIDIOSIS
Etiology and Epidemiology
Horses may be infected by three species of coccidia: Eimeria leuckarti, E. solipedum, and E. uniungulsti.64–66 Infection with Cryptosporidium parvum, another coccidial parasite of horses, is discussed later. The most common coccidial oocyst identified in equine feces is that of Eimeria leuckarti. It is a rare parasite of the small intestine of horses and donkeys worldwide.64,65,67–72 Oocysts are most frequently observed in the feces of foals and yearlings but may occasionally be detected in older horses.65,67,69,73 Studies of oocyst shedding on Kentucky horse farms in 1986 and 2003 revealed shedding in approximately 40% of foals on more than 80% of farms.74,75 The mean age for the first appearance of oocysts in the feces was 70 days; the age of the oldest foal shedding oocysts was 185 days. The longest oocyst shedding period was about 4 months.
Pathogenesis and Clinical Signs
The prepatent period for experimentally induced E. leuckarti infection in horses is approximately 35 days.64,69 Early gametocytes of E. leuckarti are found in cells of the lamina propria of villi in the equine small intestine.64 Microgametes and microgametocytes are visible by 23 days after infection; at 28 days, macrogametes have begun formation of an oocyst wall in the cytoplasm of host cells. These findings suggest that the life span of parasitized host cells is up to 28 days, much longer than the expected life span for normal intestinal epithelial cells (approximately 2-3 days). The host cells parasitized by Eimeria species appear to be epithelial cells that have been displaced to the lamina propria.66 Most horses shedding oocysts of E. leuckarti show no clinical signs of gastrointestinal (GI) disease, and it is largely regarded as nonpathogenic in horses.65,73,76 It has been recorded as an incidental finding in horses with diarrhea,77,78 intestinal hemorrhage,71 and catarrhal inflammation of the jejunum.79 Experimental infections of ponies and foals have not been associated with any clinical signs attributable to coccidiosis.69,80
Diagnosis and Therapy
Oocysts can be detected in the feces of horses by standard fecal flotation with saturated sugar or sodium nitrate solution (see Fig. 58-8).67,69,72,74,81 They are dark brown, thick walled, and ovoid and contain a prominent micropyle on the narrower end.76 The oocysts of E. leuckarti are larger than those of most Eimeria spp. (80-90 μm × 49-69 μm).76 Because infection with E. leuckarti is generally considered to be nonpathogenic, no therapeutic regimens have been reported.
CRYPTOSPORIDIOSIS
Etiology, Epidemiology, and Pathogenesis
Cryptosporidium parvum is a coccidian parasite in the suborder Eimeriorina that infects the microvilli of intestinal epithelial cells in many domestic and wild animal species, including horses and humans. Strains that infect calves, horses, and humans are cross-transmissible, and cryptosporidiosis is considered a zoonotic disease.82,83
Horses become infected with C. parvum by ingestion of oocysts. Oocysts are approximately 4 to 5 μm in diameter, smaller than those of most coccidia (see Fig. 58-9). Cryptosporidia develop in the apical surfaces of parasitized GI epithelial cells, beneath the limiting cell membrane, but separate from the host cell cytoplasm.84 In contrast to other coccidia, Cryptosporidium oocysts are sporulated and infectious at the time they are excreted into the feces. Some oocysts have a thick wall that enhances survival outside the host. Other oocysts have thinner walls and the potential to release sporozoites during passage through the lower gut with immediate infection of host cells and propagation of clinical disease.76,82 Damage to intestinal microvilli results in malabsorption, maldigestion, and diarrhea.
There are relatively few studies of the prevalence of cryptosporidiosis in horses,85–90 and the prevalence of fecal shedding of oocysts is low.85,86,88–90 In contrast, a serosurvey of horses in England demonstrated that 91% of 22 horses were seropositive, suggesting that subclinical infection is common.87
A cross-sectional study of 152 horses at a large horse show, admitted to a veterinary teaching hospital, and on a breeding farm examined the prevalence and risk factors for shedding of C. parvum oocysts.85
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree