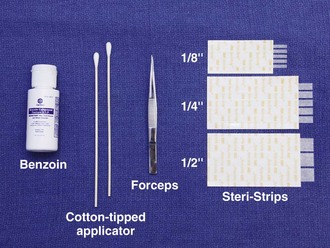
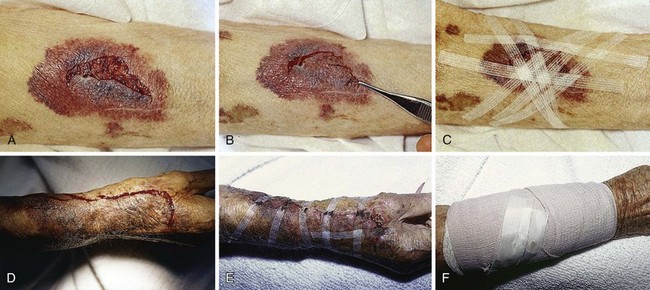
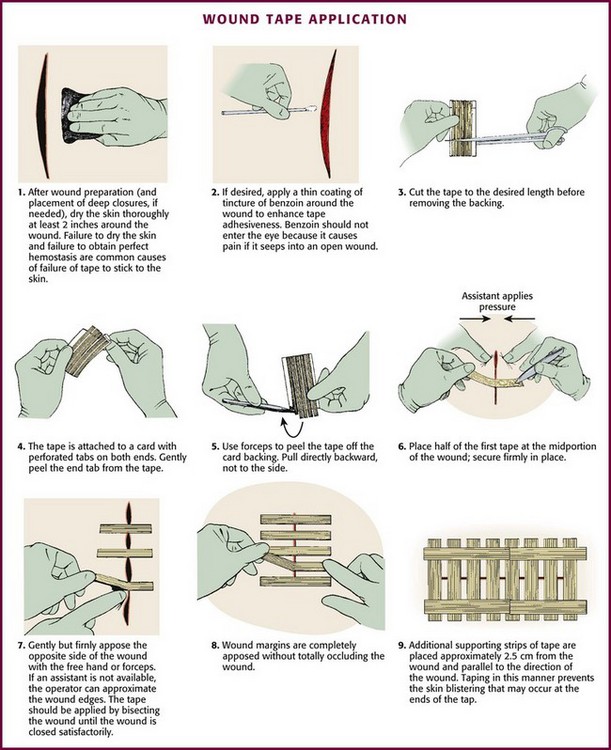
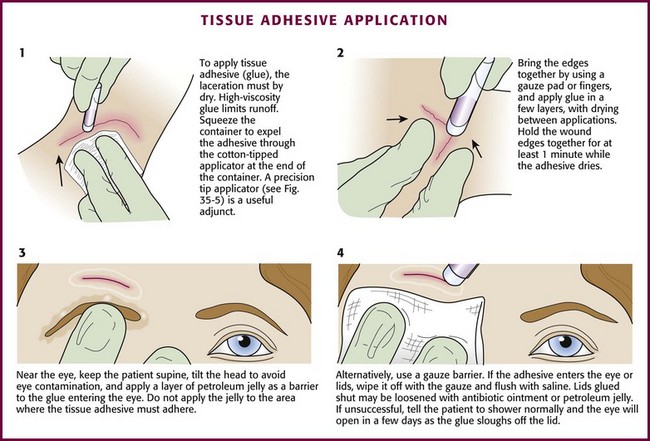
Chapter 35 Not all wounds require definitive closure at the first emergency department (ED) encounter; however, once the decision to close a wound has been made, the clinician must select the closure technique best suited for the location and configuration of the wound. The most commonly used techniques include tape, tissue adhesive, metal staples, and sutures. All traumatic wounds should be cleaned, and wounds containing devitalized tissue should be débrided before closure (see Chapter 34). Surgical tape strips are now routinely used to close simple wounds. Tape strips can be applied by health care personnel in many settings, including EDs, operating rooms, clinics, and first aid stations. Advantages include ease of application, reduced need for local anesthesia, evenly distributed wound tension, no residual suture marks, minimal skin reaction, no need for suture removal, superiority for some grafts and flaps, and suitability for use under plaster casts. One main advantage of wound tape over standard sutures and wound staples is its greater resistance to wound infection.1–4 Currently, several brands of tape with different porosity, flexibility, strength, and configuration are available. Steri-Strips (3M Corporation, St. Paul, MN) are microporous tapes with ribbed backing (Fig. 35-1). They are porous to air and water, and the ribbed backing provides extra strength. Cover-Strips (Beiersdorf, South Norwalk, CT) are woven in texture and have a high degree of porosity. They allow not only air and water but also wound exudates to pass through the tape. Shur-Strip (Deknatel, Inc, Floral Park, NY) is a nonwoven microporous tape. Clearon (Ethicon, Inc, Somerville, NJ) is a synthetic plastic tape whose backing contains longitudinal parallel serrations to permit gas and fluid permeability. An iodoform-impregnated Steri-Strip (3M Corporation) is intended to further retard infection without sensitization to iodine.3 Other tape products include Curi-Strip (Kendall, Boston), Nichi-Strip (Nichiban Co., Ltd, Tokyo), Cicagraf (Smith & Nephew, London), and Suture Strip (Genetic Laboratories, St. Paul, MN). Scientific studies of wound closure tapes provide some comparisons of products. Koehn5 showed that Steri-Strip tape maintains adhesiveness about 50% longer than Clearon tape does. Rodeheaver and coworkers6 compared Shur-Strip, Steri-Strip, and Clearon tape in terms of breaking strength, elongation, shear adhesion, and air porosity. The tapes were tested in both dry and wet conditions. Steri-Strip tape had about twice the breaking strength of the other two tapes in both dry and wet conditions; there was minimal loss of strength in all tapes when wetted. Shur-Strip tape showed approximately two to three times the elongation of the other tapes at the breaking point, whether dry or wet. Shear adhesion (amount of force required to dislodge the tape when a load is applied at the place of contact) was slightly better for the Shur-Strip tape than for the Steri-Strip tape and approximately 50% better than for the Clearon tape. Of these three wound tapes, the investigators considered Shur-Strips to be superior for wound closure. One comprehensive study of wound tapes compared Curi-Strip, Steri-Strip, Nichi-Strip, Cicagraf, Suture Strip, and Suture Strip Plus.7 All tapes were 12 mm wide except for Nichi-Strip, which was 15 mm. Each tape was compared for breaking strength, elongation under stress, air porosity, and adhesiveness. Curi-Strip, Cicagraf, and Steri-Strip exhibited equivalent dry breaking strength. However, when wet (a condition that can occur in the clinical setting), Cicagraf outperformed all tapes. All the tapes tested had similar elongation-under-stress profiles with the exception of Suture Strip Plus. This tape did not resist elongation under low or high force. Excessive elongation may allow wound dehiscence. Nichi-Strip was the most porous to air, and Cicagraf was almost vapor impermeable. Nichi-Strip and Curi-Strip had the best adherence to untreated skin. When the skin was treated with tincture of benzoin, however, Steri-Strip dramatically outperformed all other products. When all study parameters were considered, Nichi-Strip, Curi-Strip, and Steri-Strip achieved the highest overall performance rankings. In experimental wounds inoculated with Staphylococcus aureus, tape-closed wounds resisted infection better than did wounds closed with nylon sutures.2 Tape closure works well under plaster casts when superficial suture removal would be delayed. Tape closure effectively holds flaps and grafts in place, particularly over the fingers, the flat areas of the extremities, and the trunk (Fig. 35-2).3,4 Wounds on the pretibial area are difficult to close, especially in the elderly because of tissue atrophy. Wound tape provides an alternative to suture closure in this situation. Tape closure can also be applied to wounds after early suture removal, particularly on the face, to maintain approximation of the wound edges while reducing the chance of permanent suture mark scarring. Finally, because of the minimal skin tension created by tape, it can be used on skin that has been compromised by vascular insufficiency or altered by prolonged use of steroids. Do not place tape tightly and circumferentially around digits because it has insufficient ability to stretch or lengthen (Fig. 35-3). If placed circumferentially, the natural wound edema of an injured digit can make the tape act like a constricting band, which can lead to ischemia and possible necrosis of the digit. Use semicircular or spiral placement techniques if digits are to be taped. For simple tape closure, the equipment required includes forceps and tape of the proper size (see Fig. 35-1). Most taping can be done in the ED with Proper wound preparation, irrigation, débridement, and hemostasis must precede tape closure. Fine hair may be cut short. Dry the area of tape application thoroughly to ensure proper adhesion. Do not attempt to apply tape to a wet area or over a wound that is slowly oozing blood because it will usually result in failure of the tape to stick to the skin. On fingers, tape can be applied to a wound that is kept dry by temporarily placing a tourniquet at the base of the finger (see Fig. 35-3). The technique of applying tape is shown in Figure 35-4. After the wound has been dried, apply a liquid adhesive such as tincture of benzoin or Mastisol to the skin adjacent to the wound to increase adhesion of the tape.2 All tape comes in presterilized packages. Open them directly onto the operating field. Handle tape with gloved hands. With the backing still attached, cut the tape to the desired length or long enough to allow approximately 2 to 3 cm of overlap on each side of the wound. After the end tab is removed, gently remove the tape from its backing with forceps by pulling straight back. Do not pull to the side because the tape will curl and be difficult to apply to the wound. Place half of the tape securely at the midportion of the wound. Gently but firmly appose the opposite wound edge to its counterpart. Apply the second half of the tape next. Hold the wound edges as close together as possible and at equal height to prevent the development of a linear, pitted scar. Apply additional tape by bisecting the remainder of the wound. Place a sufficient number of tape strips so that the wound is completely apposed without totally covering the entire length of the wound. Finally, place additional cross tapes to add support and prevent blistering caused by unsupported tape ends.1 Complications are uncommon with tape closure. The wound infection rate in clean wounds closed with tape compares favorably with rates for other standard closures.1 However, some investigators believe that tape closure leads to inferior cosmetic results.8 Premature tape separation occurs in approximately 3% of cases.6 Other complications include (1) skin blistering, which occurs if the tape is not properly anchored with cross-strips or the tape is stretched too tightly across the wound, and (2) wound hematoma, which results if hemostasis is inadequate. Tape may loosen prematurely over shaved areas as hair grows back. When tincture of benzoin is used, apply it carefully to the surrounding, uninjured skin. Be careful because if spillage into the wound occurs, there is a higher risk for infection.9 Benzoin vapor can cause pain when applied near an open wound that has not been anesthetized. Benzoin can also injure the conjunctival and corneal membranes of the eye. Modern tape products and techniques serve a valuable role in the management of minor wounds in the ED. In selected wounds, tape closure is as successful as suture closure.1,10 Closure tape should be considered for superficial wounds in cosmetically unimportant areas and for wounds on relatively flat surfaces that are too wide for simple dressings but do not require sutures. Tissue adhesive (also called tissue “glue”) provides a simple, rapid method of wound closure. Tissue adhesive has been approved for use in the United States since 1998. Two types of tissue adhesive are available: N-2-octylcyanoacrylate (Dermabond, Ethicon, Inc.) and N-butyl-2-cyanoacrylate (Indermil, Tyco Healthcare Group LP). Animal studies have shown octylcyanoacrylate-based adhesive to have significantly greater strength and flexibility than butylcyanoacrylate-based adhesive. Dermabond and Indermil are packaged in sterile, single-use ampules (Fig. 35-5). These bonding agents can be used on superficial wounds, even in hair-bearing areas. Tissue adhesives polymerize on contact with water. These substances are biodegradable but remain in the wound until well after healing.11,12 Figure 35-5 Tissue adhesive, 2-octylcyanoacrylate, comes in a variety of commercially available dispensers. Tissue adhesive can be used to approximate wounds that do not require deep-layer closure and do not have significant tension on the edges of the wound (Fig. 35-6). In preparation for closure, clean and anesthetize the wound. Débride the wound if necessary. Control bleeding of the wound. Hold the wound edges together with forceps, gauze pads, or fingers. Squeeze the small, cylindrical plastic container to expel droplets of tissue adhesive through the cotton-tipped applicator at the end of the container. Apply the adhesive in at least three to four thin layers along the length of the wound’s surface and extend it approximately 5 to 10 mm from each side of the wound. Alternatively, place the adhesive in strips perpendicular to the laceration (analogous to the placement of closure tape). The purple color of the solution facilitates placement of the droplets. Support and hold the edges of the wound together for at least 1 minute while the adhesive dries. Low-viscosity tissue adhesives may seep into the wound or trickle off rounded surfaces during application. This tendency toward migration or “runoff” can be minimized by using high-viscosity adhesives13 (e.g., Dermabond HV Topical Skin Adhesive, Ethicon, Inc.), positioning the wound horizontally, or applying the adhesive slowly. Contain runoff with wet gauze or by creating a barrier of petrolatum. Tissue adhesives can also be used to treat superficial skin tears that do not extend past the dermis. After the wound and skin flap are cleaned, lay the flap over the base of the wound and approximate the edges of the wound. Any remaining blood and serum are expressed from under the flap, and the entire area is dried. A thin layer of adhesive is applied over the wound margins and 1 to 2 cm beyond the margin. After the first layer dries, a second layer of adhesive is applied. A dressing is not required unless there is a reason to protect the wound from repeated injury.”14,15 The primary advantage of tissue adhesive is the speed of closure. Wounds can be closed in as little as one sixth the time required for repair with sutures. Application is rapid and painless. Use of tissue adhesive avoids suture marks adjacent to the wound and reduces the risk for needlestick injuries to health care personnel. Wounds closed with tissue adhesive have less tensile strength in the first 4 days than do sutured wounds,16,17 but 1 week after closure, the tensile strength and overall degree of inflammation in wounds closed with tissue adhesive are equivalent to those closed with sutures.12,18 Cosmetic results are similar to those obtained with suture repair.17,19–25 Tissue adhesive serves as its own wound dressing and has an antimicrobial effect against gram-positive organisms.26,27 The material sloughs off in 5 to 10 days, thereby saving the patient from a clinician visit. Do not apply ointments or occlusive bandages on wounds closed with tissue adhesive. Although tissue adhesive is classified as nontoxic and does not cause a significant foreign body reaction, some authors warn against placing it within the wound cavity.17,18 However, various investigators have applied specially formulated octyl-2-cyanoacrylate (“liquid adhesive bandage”) directly to open minor lacerations, abrasions, and partial-thickness wounds. When compared with adhesive bandages, wounds covered with this tissue adhesive had equivalent rates of healing and complications.”28,29 If hemostasis is inadequate or an excessive amount of adhesive is applied too quickly, the patient can experience a burning sensation or sustain a local burn from the heat of polymerization. After polymerizing, tissue adhesive can fracture with excessive or repetitive movement. Although gentle rinsing is permitted, if the adhesive is washed or soaked, it will peel off in a few days, before the wound is healed.17 If the clinician’s gloved fingers, gauze, or plastic instruments contact the tissue adhesive during application, the glove may adhere to the patient’s skin. Tissue adhesive can be removed with antibiotic ointment or petrolatum jelly or more rapidly with acetone.25 Indermil must be stored under refrigeration. One risk involving the use of tissue adhesive is its ease of use—clinicians may fail to adequately clean wounds before closure with tissue adhesive.30 Tissue adhesive should not be used to close infected wounds. There is a slightly higher risk for wound dehiscence in closures with tissue glue than with sutures.31,32 If the edges of the wound cannot be held together without considerable tension, tissue adhesive should not be used.25 Percutaneous sutures provide a more secure immediate closure than tissue adhesive does.12 Tissue adhesive should not be used near the eyes, over or near joints, on moist or mucosal surfaces, or on wounds under significant static or dynamic skin tension. See Figure 35-6 for information on managing eyelids that are accidentally glued shut. Automatic stapling devices have become commonplace for closure of surgical incisions and traumatic wounds (Fig. 35-7). Clinical studies of patients with stapled surgical incisions have found no significant difference between stapling and suturing when infection rates, healing outcome, and patient acceptance are compared.33–37 Wound stapling and nylon suture closure of skin compared favorably in wound tensile strength, complication rates, patient tolerance, efficiency of closure, scar width, color, general appearance, suture or staple marks, infection rates, and cost. In animal models, staples caused less wound inflammation and offered more resistance to infection with contaminated wounds.38–41 The most significant advantage of wound stapling over suturing is speed of closure. The most significant downside is loss of the cosmetic effect that can be achieved with meticulous suture closure. On average, stapling is three to four times faster than suturing traumatic wounds.42–44 When clinician time and cost of instruments are considered, the difference in cost between stapling and suturing is minimal43 or favors stapling.42,45 Before stapling, sometimes it is necessary to place deep, absorbable sutures to close deep fascia and reduce tension in the superficial fascia and dermal layers. To facilitate the stapling process, the edges of the wound should be everted, preferably by a second operator (Fig. 35-8, step 1). The assistant precedes the operator along the wound and everts the edges of the wound with forceps or pinches the skin with the thumb and forefinger. Stapling flattened wound edges may place the staple precisely but results in inversion of the wound. Once the edges are held in eversion, the staple points are gently placed across the wound. It is imperative to place the center of the staple device over the center of the wound to ensure the best closure and to avoid overriding or misaligned edges (difficult in an uncooperative patient). When the stapler handle or trigger is squeezed, the staple is advanced automatically into the wound and bent to the proper configuration (see Fig. 35-8, steps 2 and 3). The operator should not press too hard on the skin surface to prevent placing the staple too deeply and causing ischemia within the staple loop. When placed properly, the crossbar of the staple is elevated a few millimeters above the surface of the skin (see Fig. 35-8, step 4). A sufficient number of staples should be placed to provide proper apposition of the edges of the wound along its entire length. (One suggested method is to place a staple in the midpoint of the length of the wound and then bisect either side of the wound with additional staples. Continue the process until the edges of the wound are well opposed.) After the wound is stapled, an antibiotic ointment may be applied to minimize adherence of the dressing, and a sterile dressing is applied. If necessary, the patient can remove the dressing and gently clean the wound in 24 to 48 hours. Scalp lacerations can be cleansed by showering within a few hours. Removal of staples requires a special instrument made available by each manufacturer of stapling devices. The lower jaw of the staple remover is placed under the crossbar, and the handle is squeezed (see Fig. 35-8, steps 5 and 6). This action compresses the crossbar and bends the staple outward, thereby releasing the points of the staple from the skin. Many primary care physicians do not routinely stock the instrument. If referred for office removal of staples, the patient can be given a disposable staple removal device. Motivated patients can remove their own staples if given the removal device. The interval between staple application and removal is the same as that for standard suture placement and removal. Staples can cause significant scarring if left in place too long (Fig. 35-9). A common error during insertion of staples is failure to evert the edges of the skin before stapling (see Fig. 35-9). Eversion avoids the natural tendency of the device to invert the closure. Eversion may be accomplished with forceps or by pinching the skin with the thumb and index finger, a procedure that requires some practice. Another common error is to fail to align the middle of the staple exactly in the midline of the wound. Staples do cause marks in the skin similar to sutures. In patients who tend to scar more easily, the scar resulting from staples may be more pronounced than that produced by sutures, especially if the staples are left in place for prolonged periods. Wound stapling achieves results that are generally comparable to those of sutures for the closure of traumatic, linear lacerations in noncosmetic areas, such as the scalp, trunk, and extremities. Stapling is much faster than suturing. Wound stapling does not differ significantly from suturing in terms of cost, infection rates, wound healing, and patient acceptance. Cosmesis does, however, suffer, especially if the staples are left in too long (see Fig. 35-9D and E). In the United States, most traumatic wounds are closed by suturing. In addition to the instruments used for débridement, a needle holder and suture scissors are required for suturing (Fig. 35-10). The mechanical performance of disposable needle holders distributed by different surgical instrument companies varies considerably.46 The size of the needle holder should match the size of the needle selected for suturing—that is, the needle holder should be large enough to hold the needle securely as it is passed through tissue, yet not so large that the needle is crushed or bent by the instrument. In addition, 2.5 loupe magnification may improve inspection of wounds and facilitate the repair of facial and hand wounds.47 A wide variety of suture material is available (Fig. 35-11). Clinician preference varies widely, and there are no definitive standards on which to base the use of suture material for a particular wound or particular site. For most wounds that require closure of more than one layer of tissue, the clinician must choose sutures from two general categories: an absorbable suture for the deeper, subcutaneous (SQ) layer and a nonabsorbable suture for surface (percutaneous) closure. Sutures can be described in terms of four characteristics: 1. Composition (i.e., chemical and physical properties) 2. Handling characteristics and mechanical performance Composition: Sutures are made from natural fibers (cotton, silk), from sheep submucosa or beef serosa (plain gut, chromic gut), or from synthetic material such as nylon (Dermalon, Ethilon, Nurolon, Surgilon), Dacron (Ethiflex, Mersilene), polyester (Ti-Cron), polyethylene (Ethibond), polypropylene (Prolene, Surgilene), polyglycolic acid (Dexon), and polyglactin (Vicryl, coated Vicryl). Stainless steel sutures are rarely, if ever useful in wound closure in the ED setting because of handling difficulty and fragmentation. Some sutures are made of a single filament (monofilament); others consist of multiple fibers braided together (Table 35-1).48 Handling and Performance: Desirable handling characteristics in a suture include smooth passage through tissue, ease in knot tying, and stability of the knot once tied (Table 35-2). Smooth sutures pull through tissue easily, but knots slip more readily. Conversely, sutures with a high coefficient of friction have better knot-holding capacity but are difficult to slide through tissue. Smooth sutures will loosen after the first throw of a knot is made, and thus a second throw is needed to secure the first in place. However, the clinician may want to tighten a knot further after the first throw is made. This is difficult with rougher types of suture. TABLE 35-2 Characteristics of Suture Material Modified with permission from Hollander J, Singer A. Laceration management. Ann Emerg Med. 1999;34:351. Multifilament sutures have the best handling characteristics of all sutures, whereas steel sutures have the worst. In terms of performance and handling, significant improvements have been made in the newer absorbable sutures. Gut sutures have many shortcomings, including relatively low and variable strength, a tendency to fray when handled, and stiffness despite being packaged in a softening fluid.49,50 Multifilament synthetic absorbable sutures are soft and easy to tie and have few problems with knot slippage. Polyglactin 910 (coated Vicryl) sutures have an absorbable lubricant coating. The “frictional drag” of these coated sutures as they are pulled through tissue is less than that of uncoated multifilament materials, and resetting of knots after the initial throw is much easier. This characteristic allows retightening of a ligature without knotting or breakage and with smooth, even adjustment of suture line tension in running subcuticular stitches.51 Synthetic monofilament sutures have the troublesome property of “memory”—a tendency of the filament to spring back to its original shape, which causes the knot to slip and unravel. Some nonabsorbable monofilament sutures are coated with polytetrafluoroethylene (Teflon) or silicone to reduce their friction. This coating improves the handling characteristics of these monofilaments but results in poorer knot security.42 Three square knots will secure a stitch made with silk or other braided, nonabsorbable material, and four knots are sufficient for synthetic, absorbable, and nonabsorbable monofilament sutures.52 Five knots are needed for the Teflon-coated synthetic Tevdek.53 When coated synthetic suture material is used, attention to basic principles of knot tying is even more important. An excessive number of throws in a knot weakens the suture at the knot. If the clinician uses square knots (or a surgeon’s knot on the initial throw, followed by square knots) that lie down flat and are tied securely, knots will rarely unravel.54 Absorption and Reactivity: Sutures that are rapidly degraded in tissue are termed absorbable; those that maintain their tensile strength for longer than 60 days are considered nonabsorbable (see Table 35-1). Plain gut may be digested by white blood cell lysozymes in 10 to 40 days; chromic gut will last 15 to 60 days. Remnants of both types of suture, however, have been seen in wounds more than 2 years after placement.49,52,55 Ethicon catgut is rapidly absorbed within 10 to 14 days and is associated with less inflammation than chromic catgut is.56 Vicryl is absorbed from the wound site within 60 to 90 days49,52 and Dexon, within 120 to 210 days.57,58 When placed in the oral cavity, plain gut disappears after 3 to 5 days, chromic gut after 7 to 10 days, and polyglycolic acid after 16 to 20 days.59 In contrast, SQ silk may not be completely absorbed for as long as 2 years.52 The rate of absorption of synthetic absorbable sutures is independent of suture size.57 Sutures may lose strength and function before they are completely absorbed in tissues. Braided synthetic absorbable sutures lose nearly all their strength after about 21 days. In contrast, monofilament absorbable sutures (modified polyglycolic acid [Maxon, Davis & Geck] and polydioxanone [PDS, Ethicon]) retain 60% of their strength after 28 days.60,61 Gut sutures treated with chromium salts (chromic gut) have prolonged tensile strength; however, all gut sutures retain tensile strength erratically.49,52 Of the absorbable types of suture, a wet and knotted polyglycolic acid suture is stronger than a plain or chromic gut suture subjected to the same conditions.50,62 Polypropylene remains unchanged in tissue for longer than 2 years after implantation.63 In comparison testing, sutures made of natural fibers such as silk, cotton, and gut were the weakest; sutures made of Dacron, nylon, polyethylene, and polypropylene were intermediate in tensile strength; and metallic sutures were the strongest.50 Comparison of suture strength versus wound strength is a measure of the usefulness of a suture. Catgut is stronger than the soft tissue of a wound for no more than 7 days; chromic catgut, Dexon, and Vicryl are stronger for 10 to 21 days; and nylon, wire, and silk are stronger for 20 to 30 days.64 All sutures placed within tissue will damage host defenses and provoke inflammation. Even the least reactive suture impairs the ability of the wound to resist infection.63 The magnitude of the reaction provoked by a suture is related to the quantity of suture material (diameter × total length) placed in the tissue and to the chemical composition of the suture. Among absorbable sutures, polyglycolic acid and polyglactin sutures are the least reactive, followed by chromic gut. Nonabsorbable polypropylene is less reactive than nylon or Dacron.50,65,66 Significant tissue reaction is associated with catgut, silk, and cotton sutures. Absorbable polyglycolic acid sutures are less reactive than those made of nonabsorbable silk.67 Highly reactive material should be avoided in contaminated wounds. The chemical composition of sutures is a factor in early infection. The infection rate in experimentally contaminated wounds closed with polyglycolic acid sutures is lower than the rate when gut sutures are used.63 However, other authors have compared plain gut and nonabsorbable nylon sutures for skin closure in children and found comparable cosmetic results and infection rates.68 Lubricant coatings on sutures do not alter suture reactivity, absorption characteristics, breaking strength, or the risk for infection.51,63 Multifilament sutures provoke more inflammation and are more likely than monofilament sutures to produce infection if left in place for prolonged periods.69,70 Monofilament sutures elicit less tissue reaction than do multifilament sutures, and multifilament materials tend to wick up fluid by capillary action. Bacteria that adhere to and colonize sutures can envelop themselves in a glycocalix that protects them from host defenses,71 or they can “hide” in the interstices of a multifilament suture and, as a result, be inaccessible to leukocytes.69 PDS provides the advantages of a monofilament suture in an absorbable form, thus making it a good choice as a subcuticular stitch. Polypropylene sutures have a low coefficient of friction, and subcuticular stitches with this material are easy to pull out.72 Size and Strength: The size of suture material (thread diameter) is related to the tensile strength of the suture; threads with greater diameter are stronger. The strength of the suture is proportional to the square of the diameter of the thread. Therefore, a 4-0 suture of any type is larger and stronger than a 6-0 suture. The correct suture size for approximation of a layer of tissue depends on the tensile strength of that tissue. The tensile strength of the suture material should be only slightly greater than that of the tissue because the magnitude of damage to local tissue defenses is proportional to the amount of suture material placed in the wound.52,73 Synthetic absorbable sutures have made the older, natural suture material unnecessary for most wound closures. Polyglycolic acid (Dexon) and polyglactin 910 (coated Vicryl) have improved handling characteristics, knot security, and tensile strength. Their absorption rates are predictable, and tissue reactivity is minimal.74,75 The distinct advantages of synthetic nonabsorbable sutures over silk sutures are their greater tensile strength, low coefficient of friction, and minimal tissue reactivity.63,74 They are extensible and elongate without breaking as the edges of the wound swell in the early postoperative period.73,74 In contrast to silk sutures, synthetics can easily and painlessly be removed once the wound has healed. The monofilament synthetic suture Novafil has elasticity that allows a stitch to enlarge with wound edema and to return to its original length once the edema subsides. Stiffer materials lacerate the encircled tissue as the wound swells.76 The eyeless, or “swaged,” needle is used for wound closure in most emergency centers (Fig. 35-12). Selection of the appropriate needle size and curvature is based on the dimensions of the wound and the characteristics of the tissue to be sutured. The needle should be large enough to pass through tissue to the desired depth and then to exit the tissue or skin surface far enough that the needle holder can be repositioned on the distal end of the needle at a safe distance from the tip of the needle (Fig. 35-13). Although it is tempting to use the fingers to grasp the tip of the needle to pull it through the skin, this practice risks a needlestick. The clinician should either reposition the needle holder or use forceps to disengage the needle from the laceration. In wound repair, needles must penetrate tough, fibrous tissue—skin, SQ tissue, and fascia—yet should slice through this tissue with minimal resistance or trauma and without bending. The type of needle best suited for closure of SQ tissue is a conventional cutting needle in a three-eighths or one-half circle (Fig. 35-14). Double-curvature needles (coated Vicryl with PS-4-C cutting needles, Ethicon) may be easier to maneuver in narrow, deep wounds. For surface closure, a conventional cutting-edge needle permits more precise needle placement and requires less penetration force (Fig. 35-15).77,78 Figure 35-17 Instrument tie. (From Custalow C. Color Atlas of Emergency Department Procedures. Philadelphia: Elsevier; 2005.) Clinician preference varies widely, and there are no definitive standards on the exact method of wound preparation, manipulation of tissue, or closure technique that is preferred for any given wound. There is a tendency to overuse sutures for minor lacerations that will heal nicely with no intervention. Therefore, before suturing, one must assess the need for the procedure (Fig. 35-18). Minimizing Tissue Trauma: The importance of careful handling of tissue has been emphasized since the early days of surgery. Skin and SQ tissue that has been stretched, twisted, or crushed by an instrument or strangled by a suture that is tied too tightly may undergo necrosis, and increased scarring and infection may result. When the edges of a wound must be manipulated, the SQ tissues should be lifted gently with toothed forceps or a skin hook while avoiding the surface of the skin. When choosing suture size, the clinician should select the smallest size that will hold the tissues in place. Skin stitches should incorporate no more tissue than is needed to coapt the wound edges with little or no tension. Knots should be tied securely enough to approximate the edges of the wound but without blanching or indenting the skin surface.79 Relieving Tension: Many forces can produce tension on the suture line of a reapproximated wound. Static skin forces that stretch the skin over bones cause the edges of a new wound to gape, and they also continuously pull on the edges of the wound once it has been closed. Traumatic loss of tissue or wide excision of a wound may have the same effect. The best cosmetic result occurs when the long axis of a wound happens to be parallel to the direction of maximal skin tension; such alignment brings the edges of the wound together.76 Muscles pulling at right angles to the axis of the wound impose dynamic stress. Swelling after an injury creates additional tension within the circle of each suture.79 Skin suture marks result not only from tying sutures too tightly but also from failing to eliminate any underlying forces distorting the wound. Tension can be reduced during wound closure in two ways: undermining of the wound edges and layered closure. Undermining.: The force required to reapproximate the edges of a wound correlates with the subsequent width of the scar.80 Wounds subject to significant static tension require the undermining of at least one tissue plane on both sides of the wound to achieve a tension-free closure. To undermine a wound, the clinician frees a flap of tissue from its base at a distance from the edge of the wound approximately equal to the width of the gap that the laceration presents at its widest point (Fig. 35-19). The depth of the incision can be modified, depending on the orientation of the laceration to skin tension lines and the laxity of skin in the area. A No. 15 scalpel blade held parallel to the surface of the skin is used to incise the adipose layer or the dermal layer of the wound. The clinician can also accomplish this technique by spreading scissors in the appropriate tissue plane. Undermining allows the edges of the skin to be lifted and brought together with gentle traction.81 Potential complications of this procedure include injury to cutaneous nerves and creation of a hematoma under the flap. Because undermining may harm the underlying blood supply, this technique should be reserved for relatively uncontaminated wounds when no other methods adequately relieve wound tension.77 Layered Closure.: The structure of skin and soft tissue varies with the location on the body (Fig. 35-20). Most wounds handled in an ED require approximation of no more than three layers: fascia (and associated muscle), SQ tissue, and skin surface (papillary layer of the dermis and epidermis).82 Any “dead space” (or unapposed edges) within a wound may fill with blood or exudate and enhance the development of infection. Closure of individual layers obliterates this dead space (Fig. 35-21). Several exceptions exist to the general rule of multilayered closure. The adipose layer of soft tissue should not be closed separately. A “fat stitch” is not necessary because little support is provided by closure of the adipose layer and additional suture material may increase the possibility of infection.2,83 Scalp wounds are generally closed in a single layer. For lacerations penetrating the dermis in the fingers, hands, toes, and feet and the sebaceous skin of the nasal tip, the amount of SQ tissue is too small to warrant layered closure; in fact, SQ stitches may leave tender nodules in these sensitive locations. Layered closure is not recommended for wounds without tension, those with poor vascularity, and those with a moderate or high risk for infection. With single-layer closure, the surface stitch should be placed more deeply.64
Methods of Wound Closure
Wound Tape
Background and Tape Comparisons
Indications
Contraindications
Equipment
 × 3-inch strips. For wounds larger than 4 cm, however,
× 3-inch strips. For wounds larger than 4 cm, however,  strips provide greater strength. Most companies manufacture strips up to 1 inch wide and 4 inches long.
strips provide greater strength. Most companies manufacture strips up to 1 inch wide and 4 inches long.
Procedure
Complications
Summary
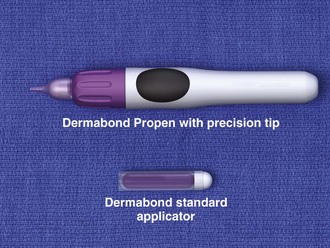
Tissue Adhesive (Tissue Glue)
Procedure
Complications
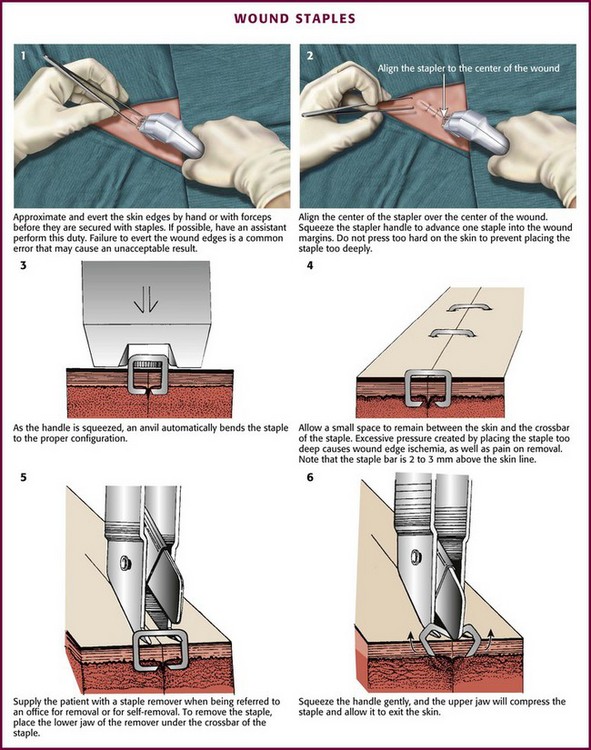
Wound Staples
Procedure
Complications
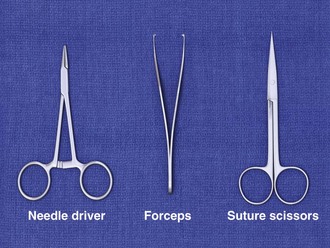
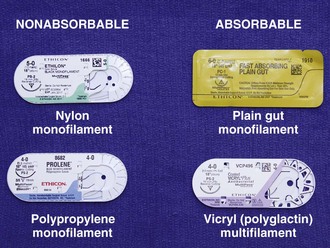
Sutures
Equipment
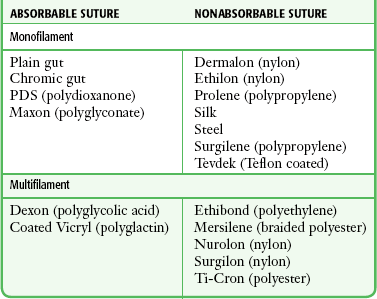
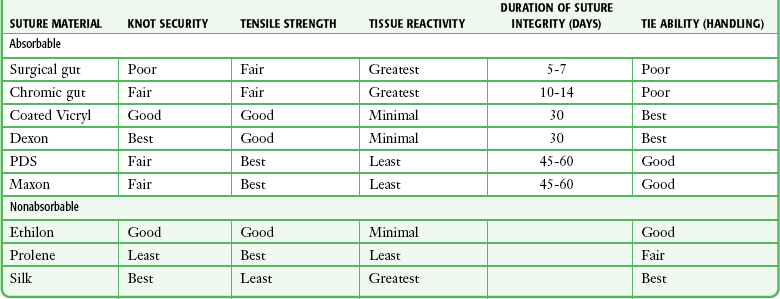
Suture Material
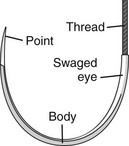
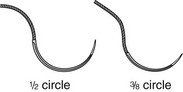
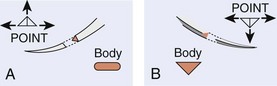
Needles
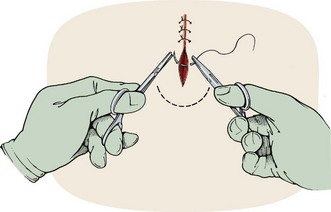
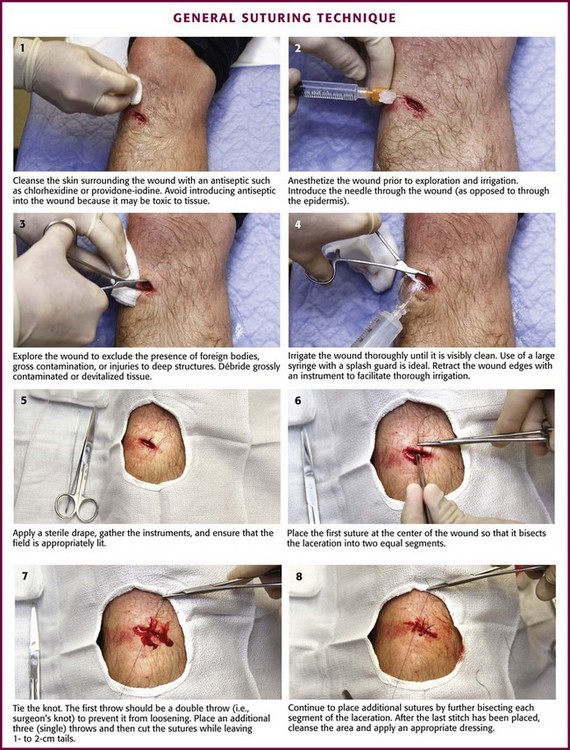
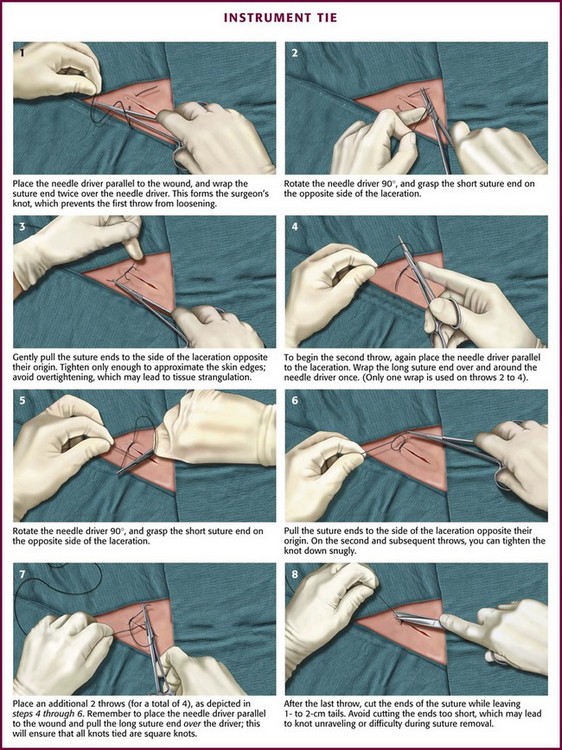
Suturing Techniques (Figs. 35-16 and 35-17)
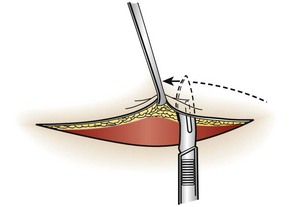
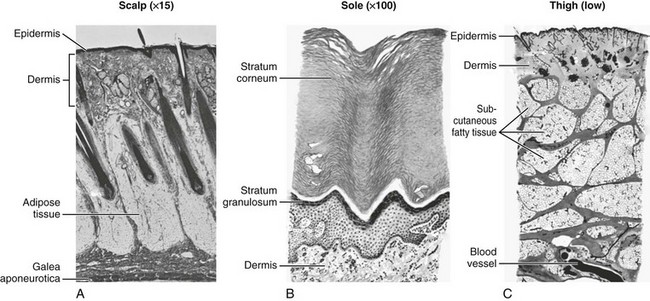
Closure Principles
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree