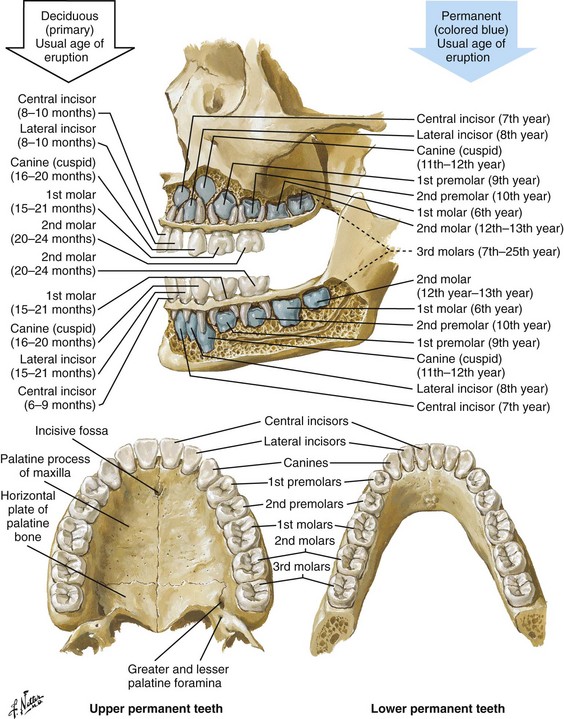
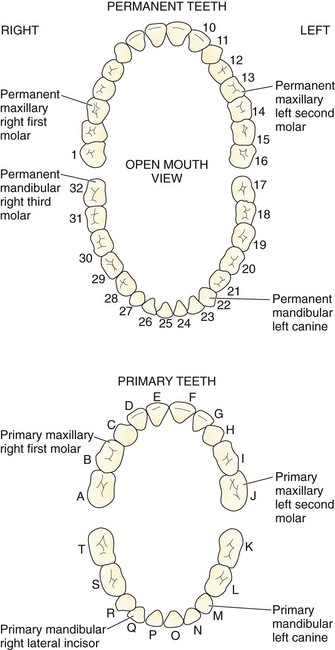
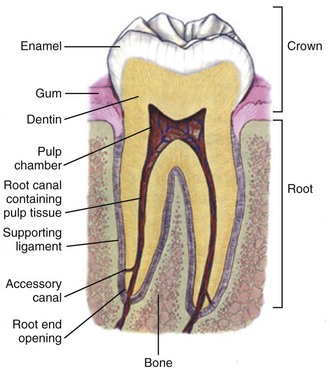
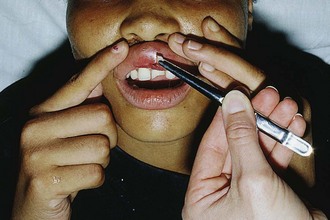
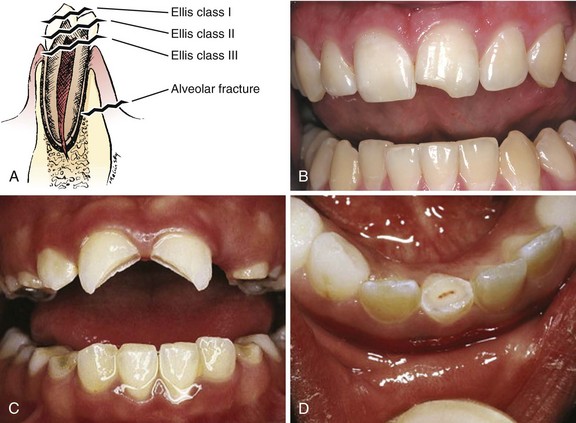
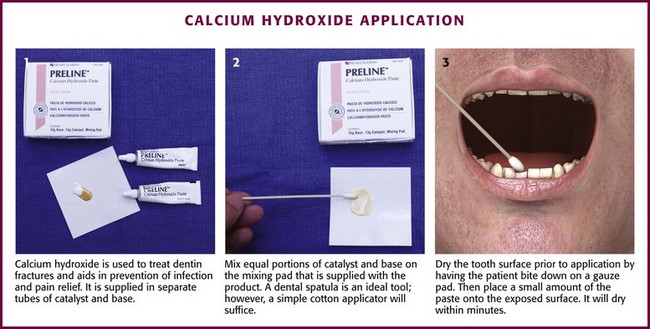
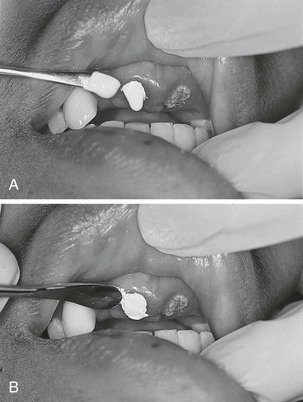
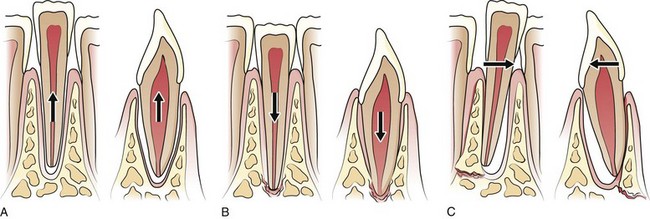
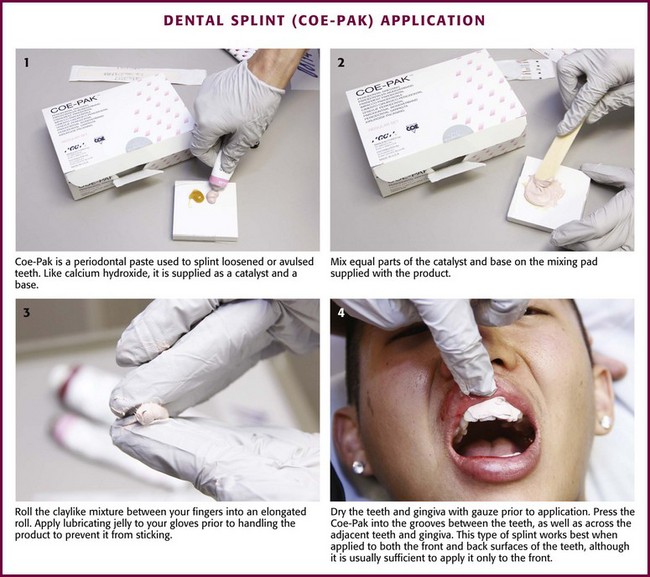
Chapter 64 The adult dentition normally consists of 32 teeth: 8 incisors, 4 canines, 8 premolars, and 12 molars. From the midline to the back of the mouth on each side, there is a central incisor, a lateral incisor, a canine, two premolars (bicuspids), and three molars, the last of which is the wisdom tooth (Fig. 64-1). The 20 primary or deciduous (baby) teeth include 8 incisors, 4 canines, and 8 molars. From the midline to the back of the mouth, there is a central incisor, a lateral incisor, a canine, and two molars (Fig. 64-2). Agenesis, or lack of proper formation of a tooth or teeth, is not uncommon, especially in the maxilla. Likewise, supernumerary, or extra, teeth may also occur. The adult teeth are numbered from 1 to 32, with the first tooth being the right upper third molar and the 16th tooth being the left upper third molar. The left lower third molar is the 17th, and the 32nd tooth is the right lower third molar. Numerous classification and numbering systems of the teeth exist; however, it is probably best for clinicians to simply describe the location and type of tooth in question (e.g., upper left second premolar, lower right canine). This removes any question wh en discussing a case with a consultant. A tooth consists of the central pulp, the dentin, and the enamel (Fig. 64-3). The pulp contains the neurovascular supply of the tooth, which is responsible for carrying nutrients to the dentin, a microporous substance that consists of a system of microtubules. The dentin makes up the majority of the tooth, is a primary determinant of tooth color, and cushions the tooth during mastication. The enamel is the relatively translucent, outermost portion of the tooth and the hardest part of the body. The tooth may also be described in terms of the crown (coronal portion) and the root. The crown is the portion covered in enamel; the root is the part that serves to anchor the tooth in alveolar bone. l. Facial: The part of the tooth that faces the opening of the mouth. This is the part that you see when somebody smiles. It is a general term applicable to all teeth. l. Labial: The facial surface of the incisors and canines. l. Buccal: The facial surface of the premolars and molars. l. Oral: The part of the tooth that faces the tongue or the palate. This is a general term applicable to all teeth. l. Lingual: Toward the tongue; the oral surface of the mandibular (and maxillary) teeth. l. Palatal: Toward the palate; the oral surface of the maxillary teeth. l. Approximal/interproximal: The contacting surfaces between two adjacent teeth. l. Mesial: The interproximal surface facing anteriorly or closest to the midline. l. Distal: The interproximal surface facing posteriorly or away from the midline. l. Occlusal: Biting or chewing surface of the premolars and molars. l. Incisal: Biting or chewing surface of the incisors and canines. l. Apical: Toward the tip of the root of the tooth. l. Coronal: Toward the crown or the biting surface of the tooth. Patients with an acute toothache (odontalgia) often come to the ED for dental evaluation and relief of symptoms. Although multiple problems can initially cause pain in the area of the teeth, the cause is usually pulpitis or dental trauma. Referral to a dentist is the logical definitive course of action, but pain relief can be initiated in the ED. Dental pain is, however, also a common complaint in drug seekers. Nonsteroidal antiinflammatory drugs (NSAIDs), acetaminophen, narcotics, and local nerve blocks can provide relief of pain, depending on the scenario. Hile and Linklater1 recently reported significant pain relief in a fractured tooth by applying 2-octylcyanoacrylate tissue adhesive (Dermabond, Ethicon Products) directly to the tooth. This intervention is currently anecdotal but may also provide temporary pain relief for patients with open decay when air and temperature exacerbate the pain. Dry the tooth thoroughly with gauze, and generously apply a few layers of the product to the affected area. This intervention lasts for a few days only but should not interfere with subsequent dental intervention. Note that the use of skin adhesives has not been approved for intraoral use; they tend to break down quickly in the oral cavity. Acute dental pain may also be referred pain, so a complete evaluation should be conducted if the area appears to be normal (Fig. 64-4). For example, acute sinusitis can cause tooth pain and vice versa. Obvious dental infection should be treated with antibiotics (e.g., penicillin, clindamycin, erythromycin, metronidazole, amoxicillin-clavulanate [Augmentin]) while awaiting dental evaluation. Chronic acetaminophen overdose is a known complication of overaggressive use of analgesics by patients unable to obtain dental care for an acute toothache.2 Unfortunately, many patients have irreversible pulpitis by the time that they seek emergency care.3 Antibiotics provide no benefit for pain from a simple toothache, dental cavity, or pulpitis, although some clinicians prescribe them because follow-up dental care may be delayed or difficult to obtain.4 Individual teeth (except the posterior molars) can be temporarily anesthetized with total pain relief by simply giving a periapical injection of a local anesthetic (see Chapter 30). Bupivacaine has a long duration of action (4 to 12 hours) and has been shown to decrease the narcotic requirement of postoperative oral surgery patients even after the anesthetic properties of the medication have worn off. Molars, which are more difficult to anesthetize with periapical injections, can be blocked via nerve block techniques. Recently, articaine (Septocaine) has been used for this purpose. It is fast acting and penetrates well. Many dentists have replaced lidocaine with articaine for local tooth anesthesia. Note, however, that this anesthetic is not used for nerve blocks, only local injection, because persistent paresthesias have been associated with nerve blocks. Dentoalveolar trauma is a common reason for ED visits. Injury to the maxillary central incisors accounts for between 70% and 80% of all fractured teeth.5–7 Trauma to the teeth is not usually life-threatening; however, the morbidity associated with dental fractures can be significant and includes failure to complete eruption, change in color of the tooth, abscess, loss of space in the dental arch, ankylosis, abnormal exfoliation, and root resorption. Dental injuries are often associated with intraoral lacerations. When a tooth is chipped or missing and there is a concomitant intraoral laceration, it should be noted that the missing portion of the tooth might be embedded in the depths of the laceration (Fig. 64-5). Management of fractured teeth depends on the extent of fracture with regard to the pulp, the degree of development of the apex of the tooth, and the age of the patient. Dentoalveolar injuries and, in particular, tooth fractures can be classified in many ways.8 The Ellis classification is one system often cited in the emergency medicine literature; however, many dentists and maxillofacial surgeons do not use this nomenclature, thus making it less than ideal when discussing these types of injuries (Fig. 64-6).6 The most easily understood method of classification is one based on a description of the injury. Uncomplicated crown fractures through only the enamel are known as Ellis class I fractures (see Fig. 64-6B). They are not usually sensitive to either temperature or forced air. These fractures generally pose minimal threat to the health of the dental pulp. They may feel sharp to the patient’s tongue, lips, or buccal mucosa. Immediate treatment is not necessary but may consist of smoothing the sharp edge of the tooth with an emery board or rotary disk sander. The patient should be reassured that a dentist can restore the tooth to its normal appearance with composite resins and bonding material. Follow-up is important with these injuries because pulp necrosis and color change can occur in rare cases (<1%).6,9,10 Uncomplicated fractures through the enamel and dentin are called Ellis class II fractures. Fractures that extend into the dentin are at higher risk for pulp necrosis and therefore need more aggressive treatment by the emergency clinician (see Fig. 64-6C). The risk for pulp necrosis in these patients is less than 10%, but it increases as treatment time extends beyond 24 hours.6 These patients often complain of sensitivity to heat, cold, or forced air. Physical examination reveals the yellow tint of the dentin in contrast to the white hue of the enamel. With fractures closer to the pulp cavity, the dentin will have a pink tinge. The tooth is usually sensitive to percussion with a tongue blade. The porous nature of dentin allows passage of bacteria from the oral cavity to the pulp, which may result in inflammation and infection of the pulp chamber. This is more likely to occur after 24 hours of dentin exposure but occurs sooner if the fracture site is closer to the pulp. Likewise, patients younger than 12 years have a pulp-to-dentin ratio larger than that in mature adults and are at increased risk for pulp contamination. For this reason, younger patients should be treated aggressively and be seen by a dentist within 24 hours.10,11 The goal of treating dentin fractures is twofold: to cover the exposed dentin and thus prevent secondary contamination or infection and to provide relief of the pain. After the tooth is covered, the dentist, using modern composites, can often rebuild the tooth directly over the calcium hydroxide (CaOH) cap that was placed in the ED. Perform supraperiosteal infiltration or a regional tooth block before any manipulation of the tooth. This will make application of the dressing easier because manipulation of the tooth will not cause discomfort. Dressings that may be applied to the surface of the tooth include CaOH, zinc oxide, skin adhesives, and glass ionomer composites. Some literature suggests that glass ionomer may be superior to other coverings; however, the difference is probably slight, and the increased cost of glass ionomer is not justified for routine use in the ED at this time.5,12 Certain composites may be cured with a bonding light. This is routinely done in the dentist’s office and is beyond the scope of most emergency practice. Bone wax and skin glue such as the cyanoacrylates are not recommended as dressings. Most dressings come as a base and a catalyst, which require mixing. This is easily accomplished with a dental spatula and a mixing pad, which can be obtained from any dental supply house. A commonly used ED dressing is calcium hydroxide (Dycal or other similar products). Mix the catalyst and the base in equal portions, and place a small amount on the exposed area with an applicator such as a dental spatula or another appropriate instrument (Fig. 64-7). Dry the surface of the tooth before application to ensure adherence of the CaOH. Have the patient bite into gauze pads to accomplish this. Dycal will dry within minutes after being exposed to the moist environment of the mouth. Although placing dental foil over the CaOH dressing is recommended, it is not usually necessary if the patient plans to follow up with a dentist within 24 to 36 hours. To prevent dislodgment of the dressing, instruct the patient to eat only soft foods until seen by a dentist. Begin antibiotic treatment with penicillin or clindamycin until definitive dental treatment can be obtained.13 Complicated fractures involving the pulp are also known as Ellis class III fractures (see Fig. 64-6D). Complicated fractures of the crown that extend into the pulp of the tooth are true dental emergencies. These fractures result in pulp necrosis in 10% to 30% of cases even with appropriate treatment.6 They may be distinguished from fractures of the dentin by the pink color of the pulp. Wipe the fractured surface of the tooth with gauze and observe for frank bleeding or a pink blush, which indicates exposure of the pulp. Fractures through the pulp are often excruciatingly painful, but occasionally, there is lack of sensitivity secondary to disruption of the neurovascular supply of the tooth. Immediate management includes referral to a dentist, oral surgeon, or endodontist. The patient often requires pulpectomy (complete removal of the pulp) or, in the case of primary teeth, pulpotomy (partial removal of the pulp) as definitive treatment.5,9 The longer the pulp is exposed, the greater the likelihood of contamination and abscess formation. If a dentist cannot see the patient immediately, attempt to relieve the pain and cover the exposed pulp (Fig. 64-8). If significant pain is present, perform a dental block. Subsequently, cover the tooth with one of the dressings described earlier. Sometimes the bleeding is brisk. Control such bleeding by applying a dressing. Ask the patient to bite onto a gauze pad that has been soaked with a topical anesthetic containing a vasoconstrictor such as epinephrine. Alternatively, inject a small amount of anesthetic/vasoconstrictor into the pulp to control bleeding. After the covering is applied, instruct the patient to follow up as soon as possible with a dentist. Antibiotics with coverage directed at oral flora (e.g., penicillin, clindamycin) should be considered and only soft foods should be eaten. Removal of the pulp with specialized instruments by the emergency clinician is not recommended, although some authors have advocated this in the past. This procedure is the realm of the dental professional and is likely to result in complications if not done properly. Subluxation refers to teeth that are mobile but not displaced. Luxation refers to teeth that are displaced, either partially or completely, from their sockets. Luxation injuries are divided into four types (Fig. 64-9): 1. Extrusive luxation is an injury in which the tooth is forced partially out of the socket in an axial direction (see Fig. 64-9A). 2. Intrusive luxation, or intrusion, occurs when the tooth is forced apically. It may be accompanied by crushing or fracture of the tooth apex (see Fig. 64-9B). 3. Lateral luxation occurs when the tooth is displaced either facially, lingually, mesially, or distally (see Fig. 64-9C). This injury is often associated with injuries to the alveolar wall. 4. Complete luxation, also known as complete avulsion, results in loss of the entire tooth from the socket. Teeth that are minimally mobile and are not displaced do very well with just conservative treatment. The tooth will tighten up in the socket if not retraumatized. Instruct patients to eat only a soft diet for 1 to 2 weeks and see their dentist as soon as possible. Note that a seemingly lost (avulsed) tooth may actually be deeply intruded into the soft tissue (Fig. 64-10). Grossly mobile teeth require some form of stabilization as soon as possible. It is important to note that in certain patients with poor gingival health, luxated teeth may not be salvageable because of disease of the attachment apparatus. Stabilization is best performed by a dental specialist with enamel bonding material or wire ligation. Although many different “home remedies” exist for splinting loosened teeth in the ED, the clinician must be aware of the possibility of aspiration of teeth if the splint fails. Avoid the use of unapproved medications in the mouth. Splinting techniques are suitable for the emergency clinician to perform as temporizing measures until definitive care can be arranged. One simple technique for emergency use is to apply periodontal paste, commercially available as Coe-Pak or other similar commercial products (Fig. 64-11). These products usually consist of a base and a catalyst that when mixed, form a moderately sticky claylike dressing that becomes firm after application. It is applied over the enamel and gingiva, as well as the adjacent teeth, to splint the subluxed tooth into place. Although the splint performs best if placed on the facial and buccal surfaces of the teeth, it is usually sufficient to apply the paste only to the front (facial) surface of the teeth. Make sure that the gingiva and enamel are completely dry. Lubricate your gloves with water or lubricating jelly before applying the dressing. Apply the dressing into the grooves between the teeth, as well as on the adjacent teeth. Remind the patient to eat a soft diet until seen in follow-up within 24 hours. Coe-Pak and other similar products are usually fairly simple for the dentist to remove during formal restoration.
Emergency Dental Procedures
Teeth
Acute Toothache in the ED
Dentoalveolar Trauma
Ellis Class I Fractures
Ellis Class II Fractures
Ellis Class III Fractures
Luxation, Subluxation, Intrusion, and Avulsion
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Emergency Dental Procedures