CHAPTER 10 Metabolism, Diet, and Obesity
Many obese cats are healthy, and owners may not understand the veterinary concern about the increase in weight. Not all obese cats develop diseases that have been associated with obesity such as arthritis, cardiovascular disease, respiratory conditions, dermatopathies, urinary tract disease, and cancer.1,2
About 20 per cent of obese people develop diabetes,3 and although a similar assessment has not been made in cats, it is likely that obese cats also are at high risk to develop the disease, as well as other diseases associated with obesity in human beings.4 The veterinarian therefore has an important role in educating cat owners about the dangers of obesity. Veterinarians must assess a cat’s body condition at each practice visit and educate owners about the importance of monitoring their pet’s weight. Unfortunately, this is a difficult topic to discuss with owners, many of whom also suffer from weight problems.
DEFINITION
Obesity is a condition in which there is an excessive amount of body fat or adipose tissue in relation to lean body mass. It is the most common nutritional disorder in cats in the United States, affecting about one third of the cat population.1,2
Well-defined, objective parameters to distinguish between a cat with normal weight, one that is overweight, and one that is grossly obese do not exist. Obesity can be assessed subjectively using the body scoring system developed by Laflamme.5 However, it can be difficult to use in cats, especially in those who have lost weight recently or who have long hair.
Objective ways to judge obesity in cats do exist. Body mass index (BMI) is well known from human medicine, where it is used to assess adiposity. It can be calculated in cats according to the following formula6:
where height is the distance from the point of the shoulder through the point of the elbow to the proximal boundary of the metacarpal pad, and length is the distance from the point of the shoulder to the tuber ischium. Obesity also can be assessed by measuring the girth circumference immediately caudal to the last rib.7 Both girth and BMI measurements do not need any specialized equipment. Highly sophisticated evaluations of adiposity include dual energy x-ray absorptiometry (DEXA) and magnetic resonance imaging.8,9 The latter modality allows the exact localization of fat depots in the body, which is not possible with DEXA. We have found that BMI and girth correlate well with DEXA results and are excellent objective markers of adiposity that could be used by clinicians. When cats become obese, both abdominal subcutaneous and visceral fat mass increase to the same extent, and both are associated with insulin resistance.8 This contrasts with human subjects in whom obesity usually is associated with a larger increase in abdominal visceral than abdominal subcutaneous obesity, and it is the former that correlates negatively with insulin sensitivity.10
PATHOGENESIS
HORMONAL AND METABOLIC CHANGES
Insulin is one of the primary regulators of energy metabolism. In obesity, two major changes develop in cats. There is a qualitative and quantitative change in the secretion of insulin, and there is change in the tissue responsiveness to insulin called insulin resistance. In fact, it has been shown that each kilogram increase in body weight in cats is associated with a 30 per cent decrease in insulin sensitivity.8,11
Glucose is the primary physiological stimulus of insulin secretion in most species. Insulin secretion in healthy subjects follows any increase in blood glucose very tightly, thereby ensuring that blood glucose is maintained within a very narrow range even after food intake. The secretion occurs in a biphasic manner and consists of an acute first phase and a delayed second, or maintenance, phase12 (Figure 10-1). Insulin resistance primarily affects the second phase of insulin secretion. A marked hypersecretion is seen in obese cats during that phase (Figure 10-2). This is a physiological response to lower tissue uptake of glucose caused by a lower expression of the insulin-sensitive glucose transporter GLUT4 in muscle and adipose tissue.13 Short term, the pancreas is able to secrete more insulin to overcome this tissue resistance. However, maintaining hypersecretion of insulin long term is only possible if the pancreatic mass and function can adapt to the increase in demand. If it fails, overt diabetes ensues. As stated above, this adaptation fails in 20 per cent of obese people and in a large percentage of obese cats.
Figure 10-1 Mean plasma and insulin concentration in eight cats after intravenous administration of glucose (1 g/kg).12
Figure 10-2 Intravenous glucose tolerance testing in six obese cats with determination of serum feline proinsulin (FPI), insulin (INS), and glucose serum concentrations (mean + SD).14
Obesity in cats also is associated with a change in the secretion of proinsulin, which is cleaved to insulin and C-peptide in the beta cell secretory granules.14 The ratio of proinsulin to insulin in the secretory granule represents an estimate for the efficiency of this conversion process, which becomes abnormal with progressive failure of beta cells. Obese cats show an initial increased proinsulin/insulin ratio when stimulated with glucose; however, this reverses during the later phase, indicating that the cellular machinery responsible for cleavage of proinsulin to insulin can respond in a delayed fashion to a strong stimulus (see Figure 10-2). There are no data about proinsulin during the progression to diabetes and in newly diagnosed diabetic cats.
It is not known if a defect in insulin secretion in obesity develops before a change in insulin sensitivity of liver and of peripheral tissues, such as muscle and adipose tissue, is detected. We believe that a defect in the action of insulin occurs first in cats, because we have identified an increase in insulin secretion indicative of insulin resistance in a group of lean cats showing glucose intolerance when made obese; however, the same increase was not observed in lean cats who maintained normal glucose tolerance when they became obese during a 6-month ad libitum food intake period.7
It is well known that many signaling pathways become abnormal with the development of obesity, not only leading to changes in glucose transport but affecting many other metabolic functions. In human beings, obesity is one of the characteristics of metabolic syndrome, as is the coexistence of insulin resistance (or glucose intolerance) with hypertension and atherogenic dyslipidemia, among other risk factors for diabetes and cardiovascular disease.15 The lipid and lipoprotein alterations seen in obese individuals include elevated cholesterol, triglycerides, and apolipoprotein B concentrations, as well as higher very-low-density lipoprotein (VLDL), low-density lipoprotein (LDL), and lower high-density lipoprotein (HDL) cholesterol levels.16 Obese cats are insulin resistant and glucose intolerant,8,17 and yet they do not show atherosclerosis and hypertension. We hypothesized that this was because even in long-term obese and insulin-resistant cats, fasting and postprandial lipid and lipoprotein concentrations would not show similarities to those found in obese human beings. However, in a recent study using novel nuclear magnetic resonance (NMR) technology, we were able to show that cats with long-term obesity develop many of the same lipid changes that are seen in obese people, whereas this is not the case for cats who have been obese only short term.18
NMR technology has greatly expanded our knowledge of plasma lipid subclasses. It is now known that not the total concentration of a lipoprotein but the lipoprotein subclass concentration and particle size correlate highly with the development of the comorbidities of obesity in people. For example, increases in large VLDL particles have been associated with coronary artery disease. The formation of small, dense HDL particles leads to higher risk for developing cardiovascular disease and insulin resistance.19,20 Small, dense LDL particles are more susceptible to oxidative modification than large particles, and thus more likely to do damage to the endothelium, which leads to atherosclerosis.21
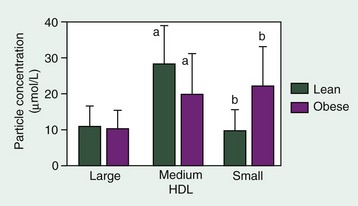
The development of obesity in cats is associated with an increase in plasma triglycerides, nonesterified fatty acids, and VLDL. The overproduction of VLDL in cats is associated with an increase in the VLDL large and medium-size particles that, in people, have been associated with cardiovascular disease.22 Despite the high VLDL concentrations, chronically obese cats show no change in baseline LDL concentrations; however, obese cats have an almost threefold higher concentration of very small and medium small LDL particles than of large particles. Increased levels of small, dense LDL particles have been shown to be strongly associated with coronary artery disease risk in people. Small HDL particles also have been associated with cardiovascular disease in human beings and are significantly higher in obese cats (Figure 10-3). It is interesting that despite all of the similarities between cats and human beings with metabolic syndrome, atherosclerosis and cardiovascular disease are not features of obesity and diabetes in cats. This suggests that additional factors present in obese people, but not in obese cats, are important in their pathogenesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree