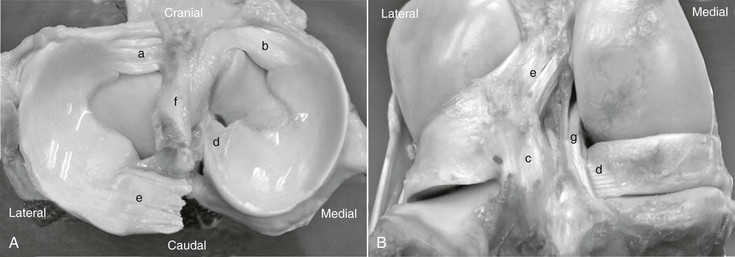
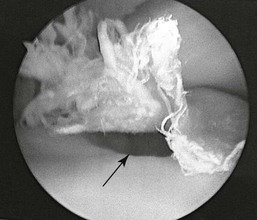
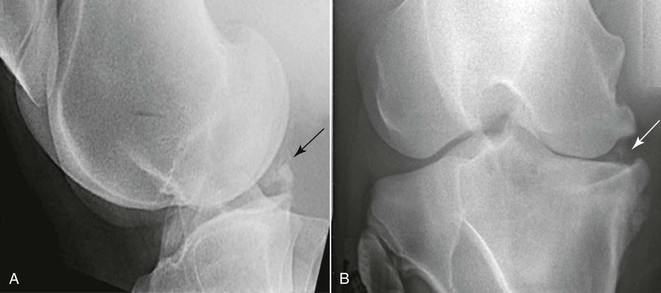
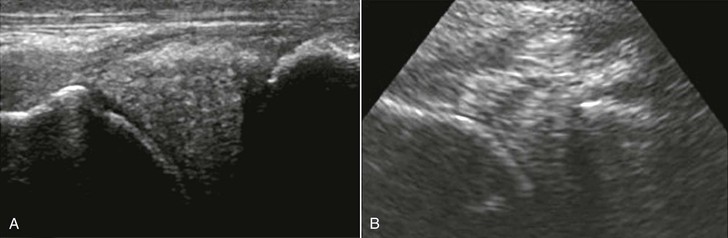
Jennifer Fowlie, John Stick The menisci are paired, semilunar, fibrocartilaginous, wedge-shaped disks interposed between the convex femoral and flat tibial condyles of the femorotibial joints. The menisci are held in place by cranial and caudal meniscotibial ligaments and an additional caudal meniscofemoral ligament on the lateral meniscus (Figure 193-1). The menisci and the associated ligaments are primarily composed of circumferential type I collagen fibers. These fibers undergo circumferential tensile strains during joint loading, a concept known as hoop stress. The menisci function in equitable load transmission, shock absorption, joint stability, joint lubrication, and proprioception. Meniscal injury may develop secondary to a fall or other type of traumatic injury, although owners often report an insidious onset. Meniscal tears are the most common soft tissue injury identified in the stifle. An isolated injury of the cranial horn of the medial meniscus and its associated meniscotibial ligament is the most common arthroscopically identified site of meniscal lesions in the horse, being affected in 79% of reported cases. The cranial horn of the medial meniscus is the least mobile of the four horns during passive flexion–extension range of motion, and it becomes compressed at full extension. The relative immobility of the cranial horn of the medial meniscus may predispose it to injury on hyperextension. Meniscal injury may also occur concurrently with other soft tissue injuries in the stifle, such as cruciate and collateral ligament injury. However, in contrast to meniscal tears in dogs and humans, only 14% of meniscal tears in horses are associated with cranial cruciate ligament injury. Medial meniscal injury has also been reported concurrently and sequentially with medial femoral condyle subchondral cystic lesions (Figure 193-2). The pathogenesis of these lesions is not established at present, but theories include the following: a single traumatic incident resulting in both lesions, alterations in femoral condyle geometry at the debrided defect resulting in meniscal trauma, or altered femoral condyle loading secondary to meniscal injury. Degenerative-appearing menisci are seen in association with chronic arthritis, although the pathophysiology of these changes has not been established. Meniscal injury leads to lameness that is often moderate to severe initially and lingers as mild to moderate lameness. A history of acute-onset unilateral hind limb lameness may be reported. A severe traumatic event may lead to injury of multiple soft tissue structures in the stifle and more severe lameness. It has been reported that only 39% of affected horses have joint effusion at presentation, so the absence of palpable effusion does not rule out a lameness of stifle origin. Hock and stifle flexion tests are commonly positive, but intraarticular anesthesia is required to definitively localize the lameness to the femorotibial joints. Localization of lameness to the stifle area with a lameness examination, flexion tests, and intraarticular anesthesia is the first step in diagnosis of meniscal injury. There are no pathognomonic clinical signs for meniscal injury. Radiographs may be unremarkable with soft tissue injuries of the stifle; however, 48% to 83% of cases of meniscal injury have been reported to have associated radiographic changes. Changes may include new bone formation at the cranial aspect of the medial intercondylar eminence of the tibia, mineralization of the meniscus, and generalized osteoarthritic changes (Figure 193-3). If the meniscus is protruding from the joint space or is severely torn, narrowing of the femorotibial joint space may be evident. Ultrasound is invaluable for diagnosis and prognostication of soft tissue injuries, and its value in evaluating meniscal tears is ever increasing. A 7- to 14-MHz linear transducer should be used to evaluate meniscal injuries in two perpendicular planes. Some meniscal lesions may be more apparent when the limb is non–weight bearing, or when a flexed cranial view is used. Ultrasound of the meniscus is challenging because the tissue fibers cannot be kept perpendicular to the probe at all sites, and a hypoechoic appearance is created in certain regions (i.e., the cranial medial meniscus). Additionally, because of the large soft tissue mass caudal to the stifle, the caudal aspect of the meniscus is very difficult to diagnostically image, even when a 4- to 6-MHz curvilinear probe is used. Abnormal ultrasonographic findings with meniscal injury may include hypoechoic regions of fiber disruption, core lesions, protrusion of the meniscus from the joint space, and generalized synovitis or arthritis changes (Figure 193-4). The sensitivity and specificity of ultrasound for identifying meniscal injuries are 79% and 56%, respectively, compared with arthroscopic findings. The apparent high rate of false-positive diagnoses may occur in part because a large portion of the meniscus is not visible on arthroscopic exam (specifically, the medial and lateral aspects of the joint) and because horizontal tears within the meniscus may not be visible on arthroscopic exam of the menisci. Thus combining findings from ultrasonographic and arthroscopic evaluation of the meniscus will yield the greatest diagnostic information. Advanced imaging modalities for the equine patient are available at select referral hospitals. Magnetic resonance imaging (MRI), considered a gold standard for soft tissue evaluation, is used extensively in humans to evaluate meniscal injury. Magnetic resonance imaging allows for excellent evaluation of bone and soft tissue components of the entire stifle joint. Given the large size of the equine stifle joint and its proximity to the abdomen, MRI of the equine stifle is limited to the large or open-bore magnets. The wide (70 cm) and ultrashort (125 cm) bore of the Siemens Magnetom Espree 1.5 T magnet1 is still only able to accommodate adult horses with relatively long limbs and narrow hips. General anesthesia is required for MRI and computed tomography (CT) evaluation of the equine stifle joint. Computed tomography is helpful in identifying soft tissue injuries, particularly when contrast arthrography is used to enhance CT imaging. The most significant advantage of MRI and CT imaging is that they enable evaluation of the entire equine stifle, which is not possible with ultrasound or arthroscopic examination. This will lead to a greater understanding of meniscal injuries and concurrent pathologic processes in the stifle joint. Nuclear scintigraphy identifies lesions based on their physiologic characteristics (blood flow and osteoblastic activity). Scintigraphy has been inconsistent in revealing stifle lesions, including subchondral bone cysts, and although it has the potential to identify meniscal lesions and associated lesions (osteoarthritis or cysts), it appears to have a relatively poor sensitivity and specificity for soft tissue lesions of the stifle.
Meniscal and Cruciate Injuries
Meniscal Injury
Clinical Signs
Diagnosis
Clinical Examination
Radiography
Ultrasound
Advanced Imaging
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Meniscal and Cruciate Injuries
Chapter 193
Only gold members can continue reading. Log In or Register to continue