CHAPTER 67 Mast Cell Tumors
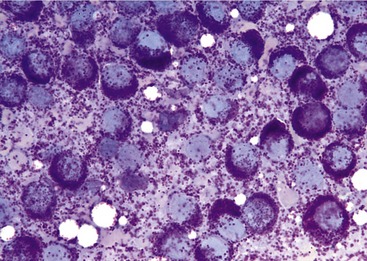
Mast cells are normal inflammatory cells that play a critical role in type I hypersensitivity reactions. They are produced in the bone marrow, enter the blood, and mature in connective tissues. They are found normally in a variety of organs including skin, lymph nodes, bone marrow, gastrointestinal tract, and respiratory tract. Mast cells are large (20 to 30 microns in diameter) round cells, with eccentric nuclei. They often are easily identified by their associated metachromatic granules, best seen with toluidine blue, Giemsa, and Romanowsky stains (Figure 67-1). These granules contain biologically active amines, including, but not limited to, histamine and heparin. As a result, significant mast cell degranulation can lead to complications including gastrointestinal ulceration, hypersensitivity reactions, coagulation disorders, and/or decreased wound healing.1,2
Neoplastic proliferation of mast cells results in the formation of a mast cell tumor (MCT). In cats MCTs typically present in one of three forms: cutaneous, visceral-splenic, and visceral-intestinal. Cats present occasionally with concomitant forms, but the relationship between these tumors remains unclear.2–4
ETIOLOGY OF MAST CELL TUMORS
The etiology of feline MCT is unknown and possibly multifactorial. A genetic predisposition seems plausible because of the high incidence of cutaneous MCTs in Siamese cats.5,6 Association with feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV) has not been reported.3 Studies of canine MCTs have demonstrated mutations in the protooncogene c-kit. Most commonly these mutations consist of internal tandem duplications in exons 11 and 12. It is believed that such mutations result in dysregulation of the tyrosine kinase receptor Kit, leading to progression of mast cell disease.7–9 The role of c-kit mutations in feline MCT is controversial. In a study of 10 formalin-fixed feline splenic MCTs, no such mutations were identified by means of polymerase chain reaction (PCR). Based on these results, the authors concluded that Kit dysregulation was an unlikely cause of splenic MCT in cats.10 In a separate study, mast cells were aspirated from the tumor of a cat with systemic mastocytosis. An internal tandem duplication was identified in exon 8 within the c-kit cDNA of this patient. The cat subsequently was treated with imatinib mesylate (Gleevec), a protein tyrosine kinase inhibitor with selectivity for c-kit in human beings (as well as Bcr-Abl and platelet-derived growth factor),11 and had a favorable response.12
FELINE MAST CELL TUMORS: CUTANEOUS
EPIDEMIOLOGY
Cutaneous MCTs are the second most common skin tumor in cats, accounting for up to 21 per cent of all reported skin tumors. Historically this was thought to be a much less common disease. However, more recent analysis has suggested that the lesions were misdiagnosed previously as eosinophilic granuloma.5 Cutaneous MCTs generally are categorized into one of three distinct histological forms—compact mastocytic, diffuse mastocytic, or histiocytic. Mastocytic forms of MCTs occur most commonly and are similar histologically to MCTs in dogs. The compact or well-differentiated mastocytic form is most common, comprising 50 to 90 per cent of cutaneous MCTs in cats. These tumors are well circumscribed and superficial. Neoplastic mast cells appear well differentiated and are accompanied by few eosinophils. Mitotic figures are infrequent, and this form is associated with a more benign behavior.13–15 The diffuse or anaplastic mastocytic form is far less common. Neoplastic mast cells are poorly differentiated with marked anisocytosis, and they often are accompanied by many eosinophils. Diffuse mastocytic MCTs are very infiltrative and generally have a more malignant behavior.13–15 The histiocytic form is rare and usually is seen on the heads of young Siamese cats. Clinically they occur as deep dermal or subcutaneous papulonodular lesions. Histologically there is a mixed population of well-differentiated mast cells, histiocytes, eosinophils, and lymphocytes. These tumors often regress spontaneously.5,6,14,15 The remainder of this section will focus on the compact mastocytic MCT.
Cutaneous MCTs occur typically in middle-age to older cats. However, they can affect cats of any age, and as mentioned, the histiocytic form of the disease occurs most commonly in young cats less than 4 years of age.4,5,15–17 Studies have suggested that Siamese cats are predisposed to both mastocytic and histiocytic MCTs, but no definitive gender predilection has been identified.5,6
CLINICAL SIGNS
Cutaneous MCTs are often solitary, raised, well-circumscribed hairless nodules (Figure 67-2), but they occur also as flat, plaquelike, and sometimes ulcerated lesions. They typically involve the dermis, but in some cases may extend into the subcutis.14,15,18 They are located most commonly on the head and neck, especially at the base of the pinna, but also may be seen on the trunk and limbs.2,4,5,16,19 They generally are small in size but range from 0.2 to 5 cm.2,13 Up to 43 per cent of cases present with multiple MCTs.16
DIAGNOSTIC EVALUATION
Metastasis to local lymph nodes and/or visceral organs is uncommon, occurring in 0 to 22 per cent of cases.4,14,16,19 For this reason the utility of staging cats with solitary cutaneous MCTs is debatable. At a minimum, tumor measurements, fine-needle aspiration and cytological examination of the mass and regional lymph node, and thorough abdominal palpation with close attention to splenic size should be performed. Because cells within these tumors exfoliate well, MCTs often are diagnosed easily with cytological evaluation.5 Photographs of the tumor also provide valuable information for the medical record. Other testing, including complete blood count, biochemical profile, FeLV antigen and FIV antibody tests, serum thyroxine (T4), urinalysis, thoracic and abdominal imaging, bone marrow aspiration, and buffy coat smear, provides a more thorough clinical picture of the cat’s overall health but rarely identifies disseminated disease. Staging cats with multiple cutaneous MCTs is recommended, because it has been proposed that the skin may be a metastatic site for visceral MCT.4,20 Histopathological examination is useful in confirming the diagnosis of cutaneous MCT. However, it is important to note that tumor grade does not correlate with biological behavior or prognosis in cats, as it does in dogs.16,18 Additionally, a study by Johnson failed to correlate cellular pleomorphism with outcome in cats with cutaneous MCT.21
TREATMENT
Surgical excision is a commonly used treatment for cutaneous MCTs, and in many cases, narrow margins are acceptable. The incidence of local recurrence is low (0 to 36 per cent), even in patients in whom the tumor is excised incompletely.4,14,16,19 The role of postoperative radiation therapy in cats with incompletely excised MCTs has not been reported.
For small, superficial tumors, strontium 90β (Sr-90) radiation therapy may be considered when surgery is not feasible (Figure 67-3). Most commonly this treatment modality is used for tumors on the face, nasal planum, and eyelids. In a study investigating this treatment modality, 54 primary cutaneous MCTs in 35 cats were treated with a median dose of 135 Gy of Sr-90 irradiation. Local tumor control was achieved in 98 per cent of affected cats with a median follow-up of 783 days and a median survival of 1075 days. Adverse effects of the treatment, including alopecia, crusting, pruritus, leukotrichia, and thinning and depigmentation of skin, were mild and self-limiting.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree