CHAPTER 49 Managing and Monitoring Systemic Hypertension
Successful management of hypertension in cats relies on routine blood pressure measurement to identify patients in need of treatment. However, it is important to recognize that the decision to treat a patient for hypertension should never be made on the basis of blood pressure measurements alone. In any clinical situation in which antihypertensive therapy is contemplated, consideration should be given to the pretest probability that the cat has hypertension. For example, a young cat without any evidence of an underlying disease that would predispose to hypertension or any signs of end-organ damage (Box 49-1) is extremely unlikely to be hypertensive. If blood pressure is measured in such a cat, it should be done to provide a baseline to monitor as the cat gets older; antihypertensive therapy would be inappropriate no matter how high the result. Conversely, an old cat with chronic kidney disease (CKD), subtle areas of subretinal fluid accumulation, and moderate blood pressure elevation should receive immediate antihypertensive therapy because the pretest probability of hypertension is very high and there is evidence that end-organ damage is occurring.
Box 49-1 Hypertension in Cats: Predisposing Clinical Conditions and Potential Target Organ Damage
| Possible Target Organ Damage Resulting from Hypertension | Clinical Problems Associated with Hypertension |
|---|---|
| Ocular Neurological Cardiovascular | Common Uncommon |
EPIDEMIOLOGY OF HYPERTENSION
These case examples illustrate how awareness of the epidemiology of hypertension influences treatment decisions, especially in the absence of end-organ lesions. One epidemiological factor to consider when deciding whether a patient should be treated for hypertension is age. In published case series of cats with hypertensive ocular lesions, it is evident that most affected cats are old, with an average age at presentation of 15 years. There are very few documented cases of systemic hypertension in cats less than 10 years of age.1 Cats with primary hyperaldosteronism may be slightly younger at presentation (mean age 10 years in one study), but this disease is relatively uncommon2 (see Chapter 24). Thus any potential diagnosis of systemic hypertension in a young cat should be considered tenuous; if there is no evidence of end-organ damage, the patient should be considered to have white-coat hypertension (see White-Coat Effect, below) until proven otherwise.
CKD has been associated with the development of systemic hypertension in cats and in other species. Published studies have shown fairly consistently that about two thirds of cats who are diagnosed with hypertension are azotemic,1,3 but estimates of the proportion of azotemic cats who are hypertensive are much less consistent, ranging from 19 to 65 per cent.4,5 These widely differing estimates probably are due to differences in the populations studied and differences in the cut-off points used to define hypertension. Contrary to expectation, cats do not appear to be more likely to become hypertensive the more azotemic that they become but usually are only mildly azotemic when hypertension is diagnosed. This fact is illustrated in Figure 49-1, which shows the creatinine concentrations in a group of 103 cats with azotemic CKD; although overall there was no difference in creatinine concentration between hypertensive and normotensive cats, the cats who were hypertensive generally were not severely azotemic. There are a couple of possible explanations for these findings. First, cats who were severely azotemic may have been hypovolemic, which reduced their blood pressure; second, hypertensive cats were often presented due to development of blindness or hyphema, not due to clinical signs associated with renal failure (e.g., polydipsia, vomiting). Therefore, when using epidemiological evidence to select patients for blood pressure measurement or to assess the likelihood that a patient is truly hypertensive, it is important to recognize that any degree of azotemia, no matter how mild, should be considered as a risk factor.
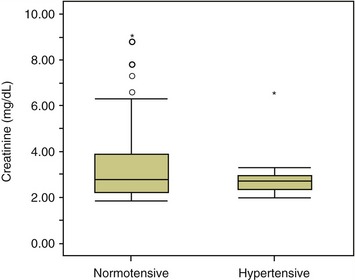
Figure 49-1 Relationship between severity of azotemia and blood pressure status. Data are taken from a cross-sectional study of 103 cats (20 of whom were hypertensive) diagnosed with azotemic chronic kidney disease in first-opinion practices.4
Interestingly, in reports of larger series of hypertensive cats published to date, about 20 to 25 per cent of the cats have been nonazotemic and nonhyperthyroid.6 Although some of these cats may have had less common causes of hypertension (see Box 49-1), it seems unlikely that rare disorders would account for this many patients. Nonazotemic, nonhyperthyroid cats have been described as having “idiopathic hypertension.” In these cats, hypertension may actually be primary—unassociated with any underlying disease process. Others have suggested that affected cats may have nonazotemic CKD. Practitioners should be aware that an identifiable cause will not be found in all hypertensive patients.
Hyperthyroidism often is cited as a common cause of hypertension in cats. However, the relationship between the two conditions is complex, not least because of the common association of both hypertension and hyperthyroidism with CKD. Experimental studies in human beings and rodents have shown that hyperthyroidism induces a reduction in total peripheral resistance (TPR) that offsets the increase in cardiac output and results in very little change in mean arterial pressure.7 This adaptation may be the reason that relatively few hyperthyroid cats have hypertensive ocular lesions8 and that similarly few cats presented for hypertensive ocular lesions have hyperthyroidism.1 Nonetheless, hyperthyroidism is the disease second most commonly associated with hypertension in cats; therefore measurement of blood pressure in all hyperthyroid cats is recommended. Hyperthyroid cats can develop hypertension following treatment, so it is important to measure blood pressure both before and after therapy.9
END-ORGAN DAMAGE
Blindness due to retinal detachment and/or intraocular hemorrhage is found commonly in cats presented with signs referable to hypertension. Less severe changes include focal retinal detachments and small intraretinal hemorrhages, areas of retinal edema, and localized narrowing of retinal arterioles. An excellent review of the ocular lesions that may be found in hypertensive cats has been published.10 One study compared oscillometric blood pressure measurements in cats with hypertensive retinopathy with measurements in healthy, nonaffected cats; more than 90 per cent of the hypertensive cats had systolic blood pressure (SBP) measurements above168 mm Hg, while 90 per cent of the healthy cats had SBP measurements below 168 mm Hg.11 These results support clinical studies that have used SBP measurements of between 160 and 170 mm Hg, in association with compatible ocular lesions, to define hypertensive retinopathy/choroidopathy.1,5,12
Neurological signs also have been reported in cats with spontaneous systemic hypertension. The signs are variable and may include focal deficits referable to the brain or spinal cord, seizures, coma, or sudden death. Development of neurological signs has been well documented in cats following renal transplantation or sub–total nephrectomy; in these patients the acuteness of the blood pressure rise may make them particularly vulnerable to injury.13,14 Anecdotally, owners report that many cats who present with severe hypertension become brighter and more active following the instigation of treatment, which may be due to resolution of neurological depression.
Cardiac changes that have been reported in hypertensive cats include auscultation of a murmur or a gallop, hypertrophy of the left ventricular free wall, asymmetric septal hypertrophy, or dilation of the aortic root (detected by echocardiography).15–17 It is important to note, however, that none of these findings are limited to cats with systemic hypertension and there is considerable overlap in echocardiographic findings in hypertensive and normotensive cats. This lack of specificity means that cardiac evaluation rarely is helpful in deciding whether a patient should be started on antihypertensive treatment. Similarly, studies of tissue Doppler imaging have shown that myocardial velocity gradients are altered to a similar degree in cats with left ventricular hypertrophy attributed to systemic hypertension and in cats with idiopathic hypertrophic cardiomyopathy.18 Heart failure has been reported in hypertensive cats but appears to be relatively uncommon.1,12,19
MEASUREMENT OF BLOOD PRESSURE
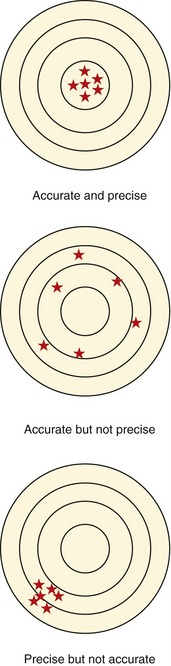
Various noninvasive methods of blood pressure measurement have been described. Unfortunately, none have been shown to measure blood pressure consistently and accurately in cats, particularly nonsedated cats. Arguably, it is more important that blood pressure measurement devices be precise, rather than accurate; however, most evaluations of the performance of blood pressure measuring devices have focused on accuracy. Using a target analogy, the different meaning of the terms accuracy and precision are represented visually in Figure 49-2. Precise measurements are reproducible, although there may be a significant bias from the “true” value. Measurement bias may not be important if it is consistent. For example, if it is known that systolic blood pressure measurements of 170 mm Hg made with a particular device predict those cats who are at risk of target organ damage, it is of no consequence if the “true” measurements are actually much greater or less than this value provided that the same device is always used for measurement. Estimates of the accuracy and/or precision of several different blood pressure measuring devices usually have been obtained in anesthetized patients. A study that compared indirect and direct blood pressure measurements in awake and anesthetized cats found that the correlation between the measurements was much stronger in anesthetized patients. This was particularly true for the oscillometric measurement device, which had a coefficient of determination (R2 value) of only 0.362 to 0.550 in conscious cats when compared with direct measurements.20 The correlation was considerably better (0.602 to 0.853) when the cats were anesthetized. Although far from ideal, the correlation between Doppler and direct measurements in awake cats was much stronger (R2 = 0.822 to 0.826) than with the oscillometric method. In a different study, measurement of blood pressure made by the Doppler method predicted the presence of end-organ damage, while those made by oscillometric methods did not.21
An additional disadvantage of the oscillometric method is the amount of time that it can take to obtain blood pressure measurements and the number of cats for which measurement is not achieved successfully. One study of 28 cats reported successful measurement in just 115 of 223 (52 per cent) attempts to measure blood pressure by the oscillometric method; in 55 per cent of cases, it took longer than 10 minutes to achieve five measurements.21 By comparison, Doppler measurement of systolic blood pressure was successful for all attempts (280) and was much faster.21 Another report describing blood pressure measurement by the oscillometric method in 203 cats also suggested that considerable time (15 to 60 minutes) be allowed for measurement.22 Blood pressure measurements were only obtained successfully using the oscillometric method in 41 of 54 (76 per cent) hypertensive cats in another study.11
For these reasons, it is the author’s opinion that blood pressure measurement in awake cats should be performed using a Doppler technique, while readily acknowledging that this method has its limitations. With practice, it usually is possible to obtain five measurements of systolic blood pressure by the Doppler method in less than 5 minutes (excluding the time allowed for acclimatization). A description of this method of blood pressure measurement is provided in Figure 49-3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree