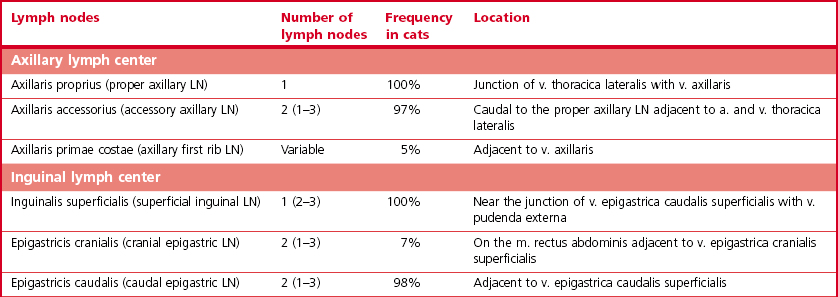
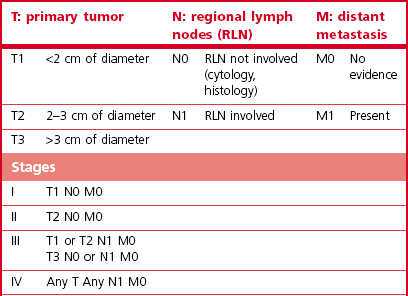
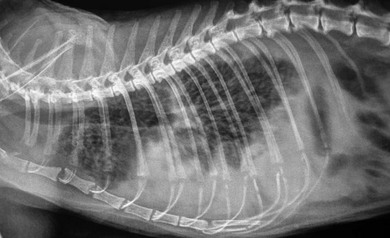
Chapter 21 Cats normally have eight mammary glands, four on each side: two thoracic (T1, T2) and two abdominal (A1, A2; A2 also referred to as the inguinal or the second abdominal mammary gland). When comparing feline and canine mammary glands, the first three pairs would be thoracic and the caudal pair abdominal or inguinal; numbered first to fourth (cranial to caudal).1–4 The terminology T1-2 and A1-2 will be used in this chapter. The nipples have five to seven lactiferous pores with one to three openings on the top and the remaining ones on the side.5 Queens may have additional rudimentary mammary glands.3 One or two rudimentary mammary glands may be found in male cats.5 The epigastric arteries supply the mammary glands. There are two arteries (cranial and caudal) that anastomose in the umbilical area, with some branches crossing the midline. The venous drainage mirrors the arterial pattern, but veins cross the midline more frequently than arteries. This makes extension of malignancy from one side to the other possible.1,6 Malignant cells from A1 and A2 may also be spread hematogenously directly via the internal thoracic and/or intercostal veins1,7 that flow into the vertebral veins.8 A summary of the blood supply is detailed in Table 21-1. Table 21-1 The arterial blood supply of feline mammary glands1 The axillary glands drain to the axillary lymph nodes and the inguinal glands to the inguinal lymph nodes (Table 21-2). The exact lymphatic drainage pattern is still debatable and there is controversy as to whether it is possible to have lymphatic spread of feline mammary malignancy from one mammary gland to other mammary glands. A summary of the conclusions relating to lymphatic drainage and potential means of metastasis is shown in Box 21-1.1,3,4,9–11 Based on the initial cytological results, further investigations might include thoracic radiographs (both right and left lateral and dorsoventral views) to check for pulmonary metastasis; abdominal ultrasound to check for pregnancy, ovarian remnants, uterine disease or lymphatic, splenic or hepatic metastasis. Computed tomography is useful for detecting pulmonary metastatic disease and for staging the tumor more effectively (Table 21-3).12 Table 21-3 Clinical staging of feline mammary tumors (Modified from Owen LN. Classification of tumors in domestic animals. Geneva: World Health Organization; 1980. http://whqlibdoc.who.int/hq/1980/VPH_CMO_80.20_eng.pdf) Feline mammary glands can be affected by benign non-neoplastic lesions (non-inflammatory and inflammatory) and tumors (benign and malignant). The diseases affecting cats are listed in Table 21-4.13,14 An accurate diagnosis is critical for staging, treatment, and prognosis. Table 21-4 Classification of feline neoplastic and non-neoplastic mammary lesions (Modified from Hampe JF, Misdorp W. Tumours and dysplasias of the mammary gland. Bull World Health Organ 1974;50:111–33; and Misdorp W, Else RW, Hellmen E, Lipscomb TP. Histological classification of mammary tumors of the dog and the cat. In Schulman FY, editor. World Health Organization International Histological Classification of Tumors of the Domestic Animals, second series, vol. 7. Washington DC: Armed Forces Instistute of Pathology; 1999. p. 11–56.) The most common benign non-neoplastic lesion in the cat is fibroepithelial hyperplasia (also known as fibroadenomatous or lobular hyperplasia) with or without ductal ectasia. There is a rapid and abnormal stromal and epithelial duct proliferation of one or more mammary glands.15 It usually affects young intact female cats at puberty, sometimes occurring after a silent estrus.16 Pseudopregnant and pregnant queens of any age can be affected due to the effects of ovarian progesterone. The condition has also been described in both male and female cats after treatment with synthetic progestagens.17–20 The exaggeratedly enlarged mammary glands (Fig. 21-1) are non-lactating, with a firm and elastic consistency. They may be edematous (with swelling extending to the pelvic limbs and potentially causing lameness), hot, painful and ulcerated, with areas of localized and superficial necrosis. Systemic signs may also be present.15,16,21 Acute mastitis should be considered as a differential diagnosis; both conditions can occur concurrently.22 A summary of the condition is listed in Box 21-2. The treatment of fibroepithelial hyperplasia is summarized in Box 21-3. Feline mammary tumors are the third most common tumors after lymphoproliferative and skin tumors in cats. They account for about 17% of neoplasia in the queen and 1–5% of all tumors in male cats.16,27–29 Benign tumors (Table 21-4) account for about 10–15% of all mammary lesions seen in cats. They occur in queens ranging in age from 1 to 9.5 years.6,16 Once the benign nature of the lesion has been ascertained, marginal surgical excision is the treatment of choice (simple mammectomy). Surgical resection is recommended as these lesions could undergo malignant transformation.15 Histology should be performed on the excised specimen, including evaluation of excision margins. Malignancy is recognized histologically in 85–93% of all mammary lesions and more than 80% are adenocarcinomas but other tumors are occasionally seen (Table 21-4).16,30,31 A viral cause has been advocated but not proven for adenocarcinomas.32,33 Predisposition has been advocated for domestic shorthaired and Siamese cats;27 in the latter breed even younger cats may be affected.31 Mammary tumor incidence increases after six years of age;34,35 the reported mean age of affected queens is 10–12 years;16 males may be a little older.28 No definitive predilection for any specific gland has been demonstrated. Adenocarcinoma may involve one (Fig. 21-3) or more glands, with at least half of the cats having more than one gland affected.16 The rate of growth is usually rapid and cats are usually presented at an advanced stage with lesions adherent to the skin and/or deep muscular fascia. Ulceration develops in over 25% of cases, and even in small lesions nipples may be swollen and exude fluid (Fig. 21-4).2,15,16 Pelvic limb thromboembolism has been reported.15 Metastasis occurs in 50–90% of cats, most commonly to regional lymph nodes (Fig. 21-5), lungs, pleura (Fig. 21-6), liver and less commonly to the adrenal glands, kidneys, diaphragm, and other organs.2,6,15,16,31,35,36 If the tumor is left untreated, the reported mean survival of cats is about one year.15,36 Figure 21-3 Feline mammary adenocarcinoma affecting single mammary glands. Gross appearance in two different elderly female cats. Fine needle aspiration should be performed in order to confirm the diagnosis. ((B) Courtesy of Lisa Mestrinho.) Figure 21-4 Ulcerated cystic mammary adenocarcinoma affecting several glands in a 12-year-old female entire cat. Figure 21-5 (A) A single ulcerated adenocarcinoma that had metastatized to both the axillary lymph nodes; (B) clinical appearance of the left axillary lymph node (arrow). (Courtesy of Julius Liptak.) Figure 21-6 Lateral thoracic radiograph showing disseminated miliary metastasis and pleural effusion secondary to a mammary adenocarcinoma. Two studies have shown a significant decrease in the risk of developing a mammary tumor if ovariohysterectomy is performed before the cat is 6 months of age34,37 and a slightly reduced risk, but still significant, if ovariohysterectomy is done when the cat is between 6 months and 1 year of age (86% risk reduction).37 There is at least a threefold increased risk of mammary tumor development (and fibroepithelial hyperplasia) in intact queens when progestagens or estrogen/progesterone combinations have been administered;32,38 this has been also documented in male cats29,39 and in zoo felids.40,41 The hormonal influence implies a receptor activity in feline mammary tumors, usually low for estrogen and moderate for progesterone receptors.18,42–46 In undifferentiated tumors the receptors are absent or only present in low numbers. Feline mammary adenocarcinoma has been proposed as a model for human mammary disease.43,47 Mammary carcinoma should be staged according to the TNM clinical staging system as described in Chapter 13 (see Table 21-3).12 If feasible, aggressive surgery is the treatment of choice, but unfortunately it is rarely curative as mammary adenocarcinoma is often presented at too advanced stage. Surgery may be combined with other therapeutic options, especially in more advanced cases. A unilateral or preferably a bilateral mastectomy should always be planned in cats. Bilateral mastectomy may be performed in one single stage or four to eight weeks apart (two-staged total mastectomy, performing a unilateral mastectomy each time). Antibiotics are given intravenously at induction of anesthesia (20 mg/kg of cephazolin). The inguinal lymph node should be removed together with A2 mammary gland and both submitted for histopathological analysis. Through a supplemental and cranial incision (or cranial extension of the mastectomy incision) the axillary node(s) are removed if enlarged and submitted for histological analysis. If not enlarged, their prophylactic removal is controversial as it is unclear whether it results in any clinical benefit.16,48,49 No real benefit has been demonstrated to performing concurrent ovariohysterectomy from an oncologic point of view.15,16,31
Mammary glands
Surgical anatomy
Blood supply
Region
Arteries
T1–T2
Axial: perforating branches of the internal thoracic arteries; cutaneous branches of the intercostal arteries from T7 caudally
Abaxial: Lateral thoracic arteries
A1
Cranial superficial epigastric artery
Cutaneous branches of the caudal intercostal arteries
Some cutaneous branches of phrenicoabdominal and deep circumflex iliac arteries
A2
Caudal superficial epigastric artery (from external pudendal artery)
Some cutaneous branches of phrenicoabdominal and deep circumflex iliac arteries
Lymphatic drainage
Diagnosis and general considerations
Further investigations
Surgical diseases
Lesion
Common
Less common / Rare
Mammary tumors: malignant
Non-infiltrating (in situ) carcinoma
Tubulopapillary carcinoma
Solid carcinoma
Cribriform carcinoma
Squamous cell carcinoma
Mucinous carcinoma73
Sarcoma and carcinosarcoma74
Carcinoma or sarcoma in a benign tumor
Inflammatory carcinoma75
Lipid-rich carcinoma76
Lymphangiosarcoma77
Histiocytic sarcoma58
Mammary tumors: benign
Simple adenoma
Complex adenoma Fibroadenoma
Benign mixed tumor
Duct papilloma
Inflammatory lesions
Mastitis
Abscessation
Benign lesions
Duct ectasia
Lobular hyperplasia (fibroadenomatous hyperplasia or fibroepithelial hyperplasia)
Cyst
Focal fibrosis (fibrosclerosis)
Ductal hyperplasia
Benign non-neoplastic lesions
Fibroepithelial hyperplasia
Mammary tumors
Benign tumors
Malignant tumors





Preoperative considerations and planning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree