CHAPTER 47 Linking Treatment to Staging in Chronic Kidney Disease
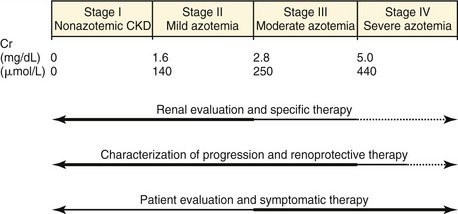
The International Renal Interest Society (IRIS) has proposed that the terms chronic renal failure and chronic renal insufficiency be replaced by chronic kidney disease (CKD) and that a staging system be used to facilitate the management of feline patients with CKD.1 This classification scheme is based on a two-step process: (1) establish a diagnosis of CKD and (2) establish the stage of the disease. Stage of disease also can be linked to prognosis,2 diagnostic approach, and treatment recommendations (Figure 47-1).1
Most feline CKD is not reversible, and once acquired, rarely resolves. Although congenital disease causes a transient increase in incidence of CKD in cats less than 3 years of age, the prevalence of CKD increases with advancing age from 5 to 6 years upward. In aged populations at referral institutions, CKD affects up to 35 per cent of cats.3,4 A reasonable estimate of the prevalence of CKD in the general feline population is 1 to 3 per cent.
ESTABLISHING A DIAGNOSIS OF CHRONIC KIDNEY DISEASE
Confirmation of a reduced GFR is a highly reliable indicator of renal dysfunction, although it must be remembered that reductions of GFR (and elevations of serum creatinine) can be caused by renal, prerenal, and postrenal factors and that renal function may be lost due to acute kidney injury (also known as acute renal failure) or CKD. In the research laboratory, GFR is assessed as urinary clearance of marker substances, such as inulin or creatinine. In clinical patients, urinary clearance tests generally are not practical; however, the measurement of the disappearance from plasma of renally cleared marker substances such as creatinine, inulin, iohexol, or diethylenetriamine pentaacetic acid (DTPA), following intravenous administration, can provide an approximation of GFR.5–9
The IRIS recommendations recognize that in most clinical patients, GFR is assessed by the measurement of plasma or serum concentrations of creatinine (Cr) and/or blood urea nitrogen (BUN). The BUN is affected by several nonrenal factors, such as protein intake, liver function, and urine flow rate, making Cr a better index of GFR. Classically, CKD in cats was diagnosed (Box 47-1) as the presence of renal azotemia (elevated Cr) accompanied by low urine specific gravity (USG) (<1.035). The wide reference range for Cr has led to the oversimplified assertion that 75 per cent of nephrons must be destroyed before Cr (and BUN) rises out of the range. Unfortunately, although valid, these diagnostic criteria are insensitive, often failing to identify CKD until dramatic loss of functional renal mass has occurred. However, any structural damage that reduces GFR almost always will be reflected as an increase in Cr (or BUN), initially within the normal range. The IRIS recommends that serial measurements of Cr be interpreted with this relationship in mind, noting that increases in Cr, even within the normal range, suggest a declining GFR and the presence of a renal disease.
Box 47-1 Establishing a Diagnosis of Renal Disease*
Recently, tests for identification of proteinuria in cats that are both sensitive and specific have been developed.10 These include the protein-creatinine ratio (UPC) and feline-specific albuminuria tests. The ability to identify persistent renal proteinuria with these tests offers promise for identifying early CKD.10 The presence of persistent renal proteinuria in a cat is suggestive of renal disease.
INITIAL EVALUATION OF CATS WITH CHRONIC KIDNEY DISEASE
For all patients with CKD, a thorough history and physical examination should be accompanied by complete clinical pathology testing, which includes a serum biochemical panel, hematology, and urinalysis with specific proteinuria tests and aerobic bacterial culture. Survey radiography, abdominal ultrasonography when available, and blood pressure measurements also should be performed (see Chapter 49). This initial battery of tests (best conducted while the disease is stable) allows the veterinarian to stage the disease and to choose proper therapeutic and diagnostic strategies.
STAGING OF CHRONIC KIDNEY DISEASE
CKD in cats often progresses along a continuum from an initial nonazotemic stage to end-stage uremia. In many cats with CKD, the rate of progression is remarkably slow. As veterinarians, we are obligated to address the specific problems and patient needs that characterize the animal’s disease, and these vary from stage to stage. Staging of an animal with an established diagnosis of CKD is based on measurement of Cr in a well-hydrated patient with stable renal function (Table 47-1).1 This classification system employs four stages: Stage I: nonazotemic CKD disease; Stage II: mild renal azotemia; Stage III: moderate renal azotemia; and Stage IV: severe renal azotemia.
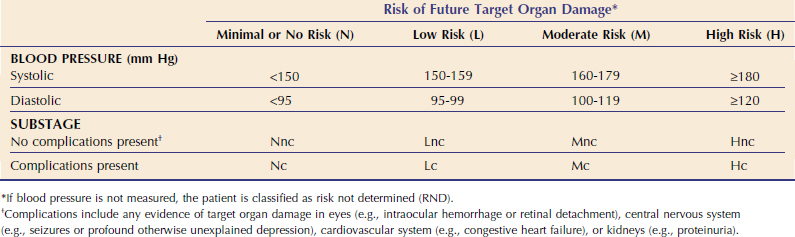
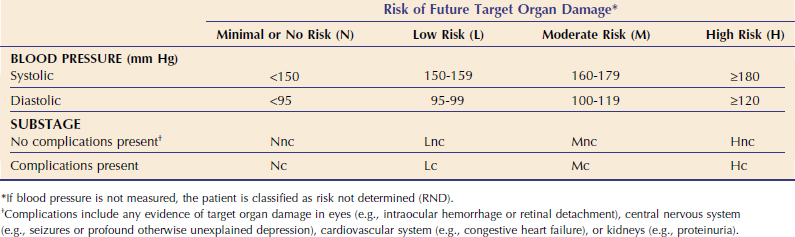
SUBSTAGING CHRONIC KIDNEY DISEASE ON BASIS OF BLOOD PRESSURE
Cats with CKD frequently exhibit elevations of systemic arterial blood pressure (BP)11 (see Chapter 49). The American College of Veterinary Internal Medicine Consensus Statement11 and IRIS1 define systemic hypertension as any elevation of BP that leads to target-organ damage (TOD) and defined blood pressure ranges associated with minimal, low, moderate, and severe risk of TOD (Table 47-2). The target organs of concern in cats are the kidneys (TOD: progression of CKD, proteinuria); eyes (TOD: blindness, intraocular hemorrhage, retinal detachment, retinal vessel tortuosity); brain (TOD: seizures, depression); and cardiovascular system (TOD: congestive heart failure, vessel rupture). Left ventricular hypertrophy (LVH) is observed commonly in hypertensive cats, although there is controversy as to whether this constitutes true TOD or is simply an adaptive change. Nonetheless, the presence of LVH in a cat with CKD should be taken as presumptive evidence of clinically significant hypertension unless proven otherwise. The IRIS recommends that BP be measured using a device and method individualized for each clinical practice in every cat with CKD and that target organs be evaluated carefully for the presence of TOD, which is referred to as a complication. Although some devices provide both systolic and diastolic BP, staging most often is done on the basis of systolic BP measurements; recent evidence suggests that systolic hypertension is the most important determinant of TOD in other species.11 Additional information about blood pressure measurement and feline hypertension can be found in Chapter 49.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree