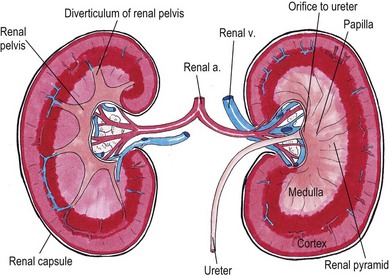
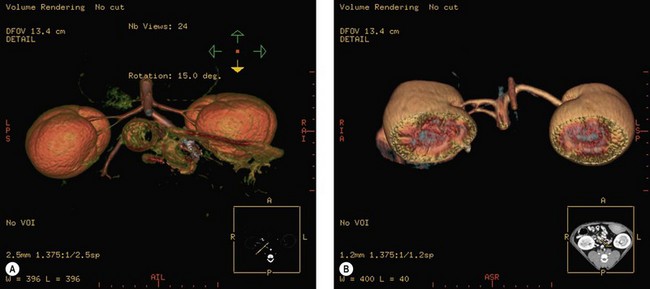
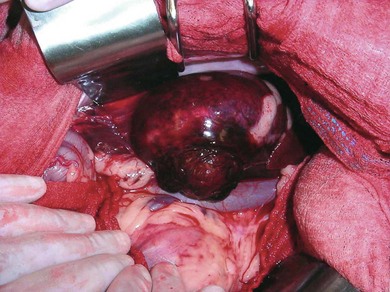
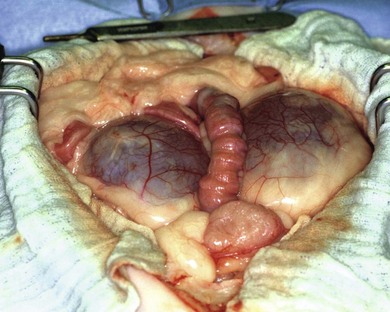
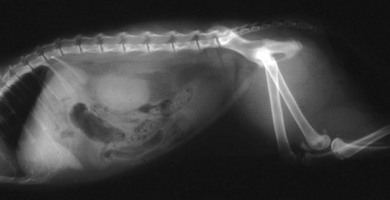
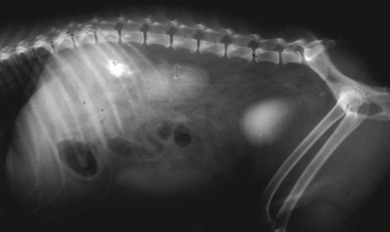
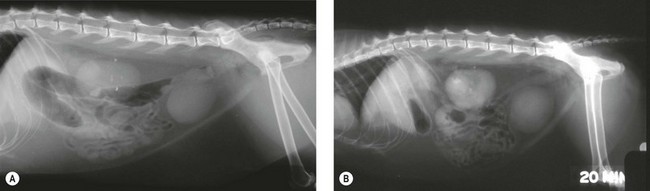
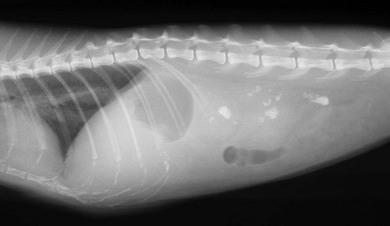
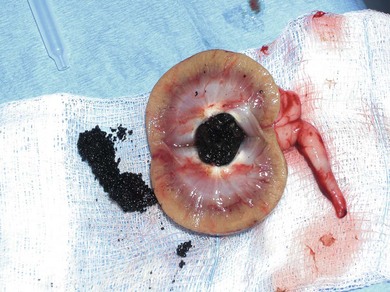
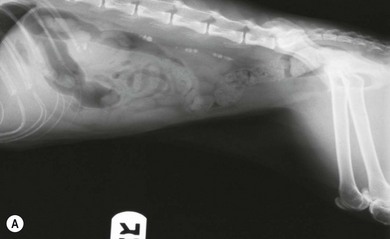
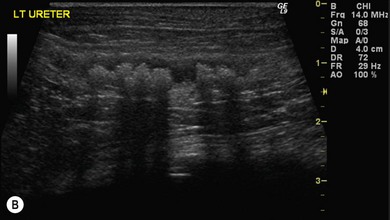
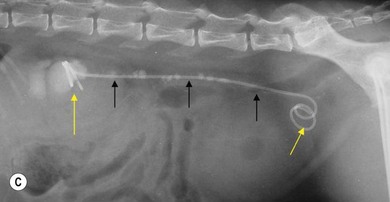
Chapter 36 The kidneys are retroperitoneal organs that lie adjacent to the sublumbar musculature on either side of the abdominal aorta and caudal vena cava. The right kidney lies more cranial than the left, lying within the renal fossa of the caudate lobe of the liver attached by the hepatorenal ligament. Although the right kidney is located at the L1–L4 vertebrae and the left kidney is located at L2–L5, the kidneys are not rigidly fixed to the surrounding tissues and are equally mobile. The entire left kidney can often be easily palpated on physical examination; the cranial pole of the right kidney may be harder to palpate because of its location adjacent to the ribs and liver. Normal renal size in the cat has been determined radiographically by calculating the ratio of kidney length to the second lumbar vertebral body length. Based on multiple studies, a normal renal size ratio of 2.0–3.0 has been reported.1–5 Additionally, there is a significant difference in the ratios between neutered and intact cats. Neutering of cats resulted in a ratio of 1.9–2.6 compared with 2.1–3.2 for intact cats and should be taken into consideration when evaluating kidney size, particularly in the diseased state.6 The renal hilus, located medially, is the opening into the renal sinus and transmits the renal artery, vein, nerves and is the location of the renal pelvis (Fig. 36-1). Because the aorta is normally located to the left of the caudal vena cava, the left kidney has a long renal vein and the right kidney has a long renal artery. The renal artery in the cat typically lies dorsal and sometimes slightly cranial to the renal vein. Upon entering the kidney, the renal artery divides into interlobar arteries. These vessels radiate through the medulla to the corticomedullary junction, where arcuate arteries are formed.7 These arteries then give rise to other interlobar arteries that run perpendicular through the cortex and eventually give rise to the afferent arterioles of the glomerulus.7,8 The surface of the feline kidney is grooved because of the presence of large subcapsular veins that eventually join the renal vein at the renal hilus.8 The left testicular or ovarian vein typically drains into the left renal vein. Normal renal vascular anatomy was evaluated in a group of 114 healthy feline kidney donors using helical computed tomography angiography (CTA). Similar to humans, multiple renal veins were more common on the right (45/114) compared to the left (3/114) and multiple renal arteries were more common on the left (8/114) compared to the right (0/114).9 Additionally, a split vena cava was occasionally identified. The ureter, which is retroperitoneal for the proximal two-thirds and intraperitoneal for the distal third, courses adjacent to the sublumbar musculature from the renal hilus, travels through the two layers of peritoneum which form the lateral ligaments of the bladder and terminates on the dorsal surface at the bladder neck.10 It courses in a ‘J’ shape, looping around the ductus deferens in the male, eventually passing obliquely through the bladder wall to empty into the lumen just cranial and lateral to the vesicourethral juncture. The oblique passage of the distal ureter is important in preventing reflux from the bladder into the ureter. As the bladder expands, the terminal ureter becomes compressed. Enough pressure generated by a peristaltic wave is necessary to force urine through the compressed distal ureter.11 The blood supply of the feline ureter is derived from multiple sources including a cranial supply from the renal artery, a caudal supply from the vaginal or prostatic artery, and additional branches that join the ureteral artery from surrounding sources.12,13 The cranial and caudal arteries anastomose along the length of the ureter within the outer layers of the adventitia.14 Venous drainage follows the arterial supply.4 The ureter is composed of smooth muscle with an inner longitudinal layer and middle circular layers. An outer longitudinal layer is also present and is best developed adjacent to the bladder.11 The normal pacemaker for this muscle is located within the kidney15 and when the muscle contracts, urine is propelled from cranial to caudal in peristaltic waves. Surrounding the smooth muscle is a layer of adventitia containing the ureteral vessels, lymphatics, and fat. Innervation of the ureter is derived from sympathetic, parasympathetic, and sensory nerves. This innervation is not necessary for normal ureteric function; however, sympathetic tone may affect the frequency and force of an individual peristaltic wave.16 In addition to taking a history and performing a physical examination, a complete blood count, serum chemistry profile, and urinalysis should be performed. Blood work may reveal varying degrees of azotemia and anemia or may be unremarkable in patients with unilateral disease. Neither the cause nor the reversibility of renal dysfunction can be determined from the degree of azotemia.17 A routine urinalysis should be performed to evaluate the physical and chemical properties of the urine as well as evaluate the urine sediment. If the patient has a history of urinary tract infections or if there is evidence of bacteria, pyuria, and/or hematuria on sediment evaluation, then a urine culture should be performed on aseptically collected urine. Plain abdominal radiography provides information on renal size, shape, and position. The right kidney is positioned slightly cranial to the left kidney although it can be superimposed, and renal size can be assessed by comparing renal length with the length of vertebra L2. Although plain abdominal radiography does not often provide additional information when evaluating a normal ureter, the technique can be very informative for patients with radiopaque renal and/or ureteral calculi. Additionally, this technique can be helpful in the assessment of the retroperitoneal space. Urine leakage or hemorrhage in the retroperitoneal space can result in widening of the space, displacement of the kidneys from their normal position, as well as an increased heterogeneous opacity that can be visualized (Fig. 36-2). Figure 36-2 Lateral abdominal radiograph of a four-year-old male (castrated) domestic short-haired cat that was hit by a car and had a partial avulsion of the renal pelvis. There is an increase in density as well as a widening of the retroperitoneal space secondary to urine leakage. Additionally, displacement of the kidneys is identified. Ultrasonography is often performed in conjunction with plain radiography and provides information regarding the size, shape, internal architecture and location, information on surrounding tissues and allows for the differentiation of solid from fluid-filled lesions. Normal ureters are typically not visible, but the distal portion of the ureter as well as the vesicoureteral junction may be seen using a high resolution transducer.16,17 Diseases of the upper urinary tract identified with ultrasonography that may require surgical intervention include neoplastic disease, hydronephrosis and/or hydroureter secondary to urolithiasis, blood clots, mural fibrosis or extramural compression, perinephric pseudocysts, ectopic ureter, and a ureterocele.17 It is important to note that the presence of urinary dilation does not definitely diagnose an obstruction and the presence of a surgically correctable disorder.18,19 The presence of retroperitoneal fluid in conjunction with renal pelvic and ureteral dilation may be visualized in a patient with a ruptured ureter.20 Additionally, patients that are candidates for renal transplantation may have changes suggestive of end stage or polycystic kidney disease. Baseline films should be taken first to make sure that the colon is empty. General anesthesia is necessary to ensure accurate positioning and minimize adverse reactions associated with contrast administration. IVU can be performed using a bolus technique or an infusion technique. The bolus technique is useful for assessing the renal vasculature as well as identifying any parenchymal lesions during the angiographic, nephrographic, and pyelographic phases. The infusion technique optimizes visualization of the ureters and any pathology that may exist.10 The technique can provide detailed information regarding the location, size, morphology, and integrity of the kidneys and ureters. Contrast seen outside of the kidneys or ureters is indicative of rupture (Fig. 36-3). Figure 36-3 Intravenous urography performed in a five-year-old female (spayed) domestic short-haired cat that was attacked by a dog. Note the extravasation of contrast from the renal pelvis. The urine leakage was confined to the retroperitoneal space and the patient was not azotemic on presentation. A ureteronephrectomy was performed. In patients with a complete ureteral obstruction, the pyelographic phase of an IVU may be inadequate and percutaneous antegrade pyelography may be the preferred technique (Fig. 36-4). The technique can be performed under ultrasonographic and/or fluoroscopic guidance. To perform this technique, a 22G spinal needle is placed percutaneously into the renal cortex perpendicular to the capsule and into the renal pelvis. Nephropyelocentesis is performed until the diameter of the pelvis is reduced by about one-half and a small bolus of a non-ionic contrast media such as iohexol is administered. A urinalysis and culture should be performed. If ultrasound guidance is used, abdominal radiographs should be taken immediately after injection to visualize the ureters and then repeated in 15 minutes.10,21 Potential risks include renal injury and bleeding, clot formation resulting in a ureteral obstruction, laceration of the renal pelvis, and contrast ± urine leakage from the pyelocentesis site.22 In a study of antegrade pyelography for suspected ureteral obstruction in 11 cats (18 kidneys), leakage of contrast developed in 8/18 cases and prevented interpretation in five of those cases.23 For the 13 cases that did not have leakage of contrast material, the technique allowed for correct identification of the anatomical location of the ureteral obstruction. Figure 36-4 A five-year-old male (castrated) domestic short-haired cat that presented acutely azotemic. (A) Note the small right kidney and the compensatory hypertrophy of the left kidney. Multiple nephroliths are present in the left kidney as well as a proximal ureterolith obstructing the left kidney. (B) Intravenous urography was performed. Although the pyelographic phase of the unobstructed right kidney is easily visible, the pyelographic phase of the obstructed left kidney is inadequate. (C–E) CT angiography was performed in conjunction with antegrade pyelography to determine the location of the ureteral obstruction. Additionally, CT angiography was able to identify a more distal ureteral calculus (yellow arrow) not identified on plain survey radiographs. Calcium oxalate (CaOx)-containing uroliths are the predominant stone type identified in the kidney and ureter of cats (Fig. 36-6).24,25 The increase in occurrence of CaOx urolithiasis in cats over the past 20 years has paralleled the increase in identification of these stones in the kidneys and ureters.26 In fact, information collected from nine different veterinary teaching hospitals during this time period found a tenfold increase in frequency of upper urinary tract uroliths, with calcium oxalate emerging as the predominant mineral type.26 Seventy per cent of nephro-ureteroliths evaluated from 1599 cats between 1981 and 2003 were composed of CaOx; only 8% were composed of magnesium ammonium phosphate.26 Figure 36-6 A seven-year-old female (spayed) domestic long-haired cat with multiple renal and ureteral uroliths. In addition to urolithiasis, dried solidified blood (DSB) calculi have also been identified in the upper urinary tract of cats associated with ureteral obstructions (Fig. 36-7). These DSB calculi are firm and feel like stones, but typically do not contain crystalline material.27 These stones present a diagnostic challenge since they are not typically radiopaque and often not identified on ultrasonographic examination. Although uncommon, fibrosis, congenital stenosis, stricture, circumcaval ureter, neoplasia, blood clots, surgical trauma, and retroperitoneal infarction have all been associated with ureteral obstruction in cats.28–35 Figure 36-7 Dried solidified blood calculi within the renal pelvis and ureter of a cat. (Courtesy of Dr Allyson Berent.) It is not clear if CaOx uroliths lodged in the kidney or ureter will migrate into the bladder. Anecdotal evidence suggests that some stones will eventually pass into the bladder without therapy. In one report of 11 cats with ureteral CaOx uroliths, however, imaging studies were performed over periods of 11 to 42 days and no stone migrated in any of the cats over these time periods.36 Patients diagnosed with ureteroliths are often treated initially with a period of medical management, including the parenteral administration of fluids alone or in combination with diuretic therapy (mannitol) to determine if passage of ureteral calculi will occur. Additional therapies with anecdotal efficacy include the administration of various smooth muscle relaxants including prazosin, the tricyclic antidepressant amitryptilline, and other alpha antagonists such as tamsulosin. There are no reported studies as to the efficacy of any of these drugs in cats with ureterolithiasis. Unfortunately, these uroliths are less susceptible to fragmentation using shock wave lithotripsy compared to those in dogs. Because of the high number of shock waves that may be necessary in cats in order to fragment a nephrolith or ureterolith, significant renal injury may occur.37 Cats with uroliths affecting the kidney and ureter can appear asymptomatic on presentation, or with non-specific clinical signs including lethargy, weight loss, anorexia, vomiting, fever, and polydipsia and polyuria.36,38 Hematuria may or may not be present, but was the most commonly reported sign in one study on feline nephrolithiasis.39 Patients may also present with abdominal pain and splinting or renomegaly.36 A complete physical examination is performed, as many affected cats are older and may have concurrent disease(s). A urinalysis and urine culture, complete blood count, biochemical profile, and plain abdominal radiographs are usually recommended as initial investigative steps. In a study of 163 cases of ureteral calculi, azotemia (83%; 134/162) and hyperphosphatemia (54%; 84/156) were commonly identified; hypercalcemia (14%;22/152) was less commonly reported.38 A urinary tract infection was documented in 8% of cases (10/119).38 Uroliths are often visualized on plain radiographs, although small ureteroliths, radiolucent ureteroliths or those calculi overlying colonic contents are occasionally missed. Further imaging studies including ultrasonography, excretory urography, antegrade pyelography, and computed tomography are often helpful in identifying small ureteroliths, the presence of hydronephrosis and hydroureter, as well as delineating the level of a ureteral obstruction. In one report, a combination of survey radiography and abdominal ultrasonography revealed ureteroliths in 90% (63/73) of cats.38 In cats with unilateral obstructions, 76% (58/76) were azotemic and ultrasonographic evaluation of the contralateral kidney revealed changes suggestive of parenchymal disease. It is important to note that using these modalities, the end point of the ureteral obstruction is not always identified. As medical dissolution of CaOx uroliths is not available, surgical removal is often recommended if the stones are causing clinical disease. The presence of nephrolithiasis in normal cats and those with naturally occurring stage 2 or 3 chronic kidney disease is not necessarily an indication for surgical removal. In a recent study in cats with nephrolithiasis and mild or moderate chronic kidney disease, the presence of nephrolithiasis was not associated with disease progression or an increase in mortality rate.40 If surgical intervention is necessary, it is not always clear how long one should wait to address either renal or ureteral uroliths. The degree of dilatation of the renal pelvis does not correlate with the amount of functional damage.36 In the author’s experience, if medical management does not appear to be effective within 24–48 hours and a partial or complete ureteral obstruction is present, or the ureterolith is associated with an infection that does not respond to medical therapy, surgical removal is recommended. Factors that also need to be considered with regards to prognosis include the function of the contralateral kidney and the overall health of the patient. The ability of the feline kidney to recover from partial or complete outflow obstruction is unknown. Recovery of renal function depends on the severity and duration of the obstruction and the presence of pre-existing renal disease. Unfortunately, in cases of unilateral ureteral obstruction, a diagnosis may go undetected if function in the opposite kidney is normal. There are two options for removing nephroliths, a nephrotomy or pyelithotomy (see Box 36-3). Pyelithotomy may be performed if the renal calculi have created dilation of the renal pelvis and avoids occlusion of the renal vasculature. Stones lodged in the proximal ureter may be removed by ureterotomy (see Box 36-6). This technique can also be used for the mid to distal ureter or the affected area of the ureter may be removed in toto and ureteral re-implantation or a ureteroneocystostomy performed (Fig. 36-8; see Box 36-8). Ureteral stenting is a novel technique currently being performed in cats. The author has used this technique for patients with multiple ureteroliths located unilaterally or bilaterally with or without the presence of nephroliths (Fig. 36-9). Nephroliths do have the potential to pass into a ureter that was recently unobstructed, but the exact occurrence of this complication is unknown in cats.41 As the majority of stent cases are performed surgically (in some female cats they can be placed cystoscopically), knowing the incidence of re-obstruction in cases with nephroliths but only a few ureteroliths would be important when making a decision regarding the appropriate treatment option (ureterotomy vs stenting). Patients that have had a ureterotomy performed should be evaluated periodically following surgery since nephroliths have the ability to migrate into the ureter and cause subsequent obstructions. Figure 36-9 (A) Abdominal radiograph of a four-year-old female (spayed) Himalayan cat with multiple ureteroliths bilaterally. (B) Abdominal ultrasound revealing extensive shadowing from the multiple ureteroliths along the length of the left ureter. (C) Post ureteral stent placement. Stent is bypassing the ureteroliths in the right ureter. Black arrows identify the shaft of the stent, yellow arrows are the double pigtails curled in the renal pelvis and bladder. An ECG trace should be recorded and if hyperkalemia is present, it should be treated (see Chapter 2). In some severely unstable patients that present with a uroperitoneum, temporary peritoneal dialysis (see Box 36-3), hemodialysis or urinary diversion may be necessary to more completely resolve azotemia and fluid, electrolyte, and acid-base imbalances prior to definitive surgery. A complete blood count, serum biochemical analysis and urinalysis should be performed. Depending on the time to presentation, degree of trauma, and concurrent abnormalities, the complete blood count may reveal a regenerative or non-regenerative anemia and if significant hemorrhage has occurred, the platelet count may be low due to consumption. A neutrophilia with or without a left shift may be indicative of inflammation or sepsis, particularly if there was a urinary tract infection present prior to the injury. Serum biochemistry may reveal azotemia, hyperkalemia, hyperphosphatemia, hypochloremia, and hyponatremia. A venous blood gas may reveal a metabolic acidosis due to lactic acidosis in hypoperfused patients, uremia, or renal tubular acidosis. If peritoneal effusion is present, a sample should be obtained by abdominocentesis with or without ultrasound guidance or from a peritoneal dialysis catheter if one had been previously placed. The concentration of the creatinine and potassium in the fluid retrieved on abdominocentesis should be compared with that of the peripheral blood (see Chapter 37). Cytological evaluation of the abdominal fluid should also be performed to evaluate for signs of inflammation, sepsis or evidence of damage to other intra-abdominal organs. Isolated renal trauma is often difficult to diagnose since clinical signs are often non-specific. Historical information in conjunction with the presence of gross or microscopic hematuria and pain on palpation in the sublumbar region may be suggestive of a primary renal injury, but are not pathognomonic for the condition.42,43 It is important to note that the degree of hematuria does not necessarily correlate with the severity of the injury.44 Survey radiographs may reveal loss of detail and the inability to visualize one or both kidneys, displacement or asymmetry of the kidneys, and an increase in density as well as widening of the retroperitoneal space secondary to fluid accumulation. Fluid evaluation is important to determine if uroretroperitoneum or hemorrhage in the retroperitoneal space is present. If the peritoneal lining has been compromised, fluid accumulation within the peritoneal cavity will result in loss of normal abdominal detail. Occasionally, renal injury can be confirmed by excretory urography and abdominal ultrasound; however, if the renal vascular pedicle has been damaged, CT and MR angiography or exploratory surgery may be necessary in order to make a diagnosis. If excretory urography is performed, it is important that a patient be hemodynamically stable ensuring adequate renal perfusion prior to the administration of contrast material. An increased risk of toxicity exists when contrast material is administered to azotemic animals.45 Treatment of renal trauma is dictated by the extent of injury. Many patients that are azotemic secondary to renal contusions are treated with supportive care to address their renal failure. Simple lacerations as well as the presence of a subcapsular hematoma may be successfully managed conservatively; some lacerations of the kidney need to be sutured. This can be performed using a fine, absorbable suture material such as Polydioxanone (3/0 or 4/0) in a continuous, interrupted or mattress suture pattern. Additionally, depending on the extent of the injury, the laceration can be augmented with a transversus abdominis muscle flap or omentum. In some cases in which significant damage has occurred to the renal pelvis resulting in urine extravasation, surgical repair can be augmented with the placement of an ipsilateral nephrostomy tube (see below) with or without a ureteral stent (see below). Both of these techniques can be performed at the time of surgical repair or percutaneously with intraoperative fluoroscopic guidance. If severe injury has occurred resulting in persistent hemorrhage, urine extravasation, or the presence of non-viable tissue, a ureteronephrectomy (see below) is often necessary, provided the remaining kidney is thought to be functional. Although not common, complete avulsion of the kidney can occur, potentially resulting in severe and often fatal hemorrhage in the patient (Fig. 36-10). Similar to unilateral renal injury, unilateral ureteral tears can be difficult to diagnose if urine accumulation is confined to the retroperitoneal space. Clinical signs in these patients are often vague and may include lethargy, dehydration, weak peripheral pulses, pale mucous membranes, prolonged capillary refill time, sublumbar pain, vomiting, anorexia, and pyrexia.46 Clinicopathological findings in these patients may be normal. Similar to renal trauma, abdominal radiographs often reveal a loss of retroperitoneal detail and an increased size of the retroperitoneal space. Ultrasound may identify fluid accumulation. If both ureters are disrupted, signs of acute azotemia will occur. If urine leakage enters the peritoneal cavity secondary to traumatic disruption of the parietal peritoneum, uroperitoneum will develop. Excretory urography, antegrade pyelography or contrast enhanced CT is beneficial in cases of both unilateral and bilateral ureteral abnormalities. Similar to patients that have sustained renal injury, it is imperative that the patient be hemodynamically stable prior to performing the study. In cases of ureteral pelvic disruption or avulsion, repair of the injury should be performed in conjunction with a nephrostomy tube and a ureteral stent for urinary diversion as well as to promote healing and prevent stricture.42 Anastomosis of the ureter to the renal pelvis is performed with 5/0 or smaller synthetic absorbable monofilament suture in an interrupted pattern. If the contralateral kidney function is normal, ureteronephrectomy is considered because of the technical difficulty in performing this type of repair and associated complications. The effect of devascularization or crushing of the feline ureter has not been previously evaluated. In dogs, damage to the ureteral vascular supply and the duration and extent of the obstruction dictate the severity of injury to the ureter and associated kidney. In dogs, devascularization injuries were more devastating than crush injuries.47 In one canine research study, approximately 50% of ureters that were devascularized by removing 2–3 cm of proximal adventitia developed persistent strictures and obstruction.47 In contrast, crushing injuries lasting up to 60 minutes did not result in permanent renal damage and radiographic evaluation demonstrated that 90% of the strictures returned to normal within 12 weeks. Crushing of the ureter iatrogenically during surgery by grasping or ligation (e.g., inadvertently during ovariohysterectomy) may not require treatment following release of the ureter.48 If a ligature can be removed from the ureter within one week of placement, normal function of the kidney and ureter should be regained.49 In humans, obstruction of the ureter for greater than or equal to four weeks results in complete loss of function.50,51 The effect of a partial obstruction of the feline ureter on long-term function is unknown. Although rare, urinomas (para-ureteral pseudocysts) have been described in cats secondary to trauma.52,53 These pseudocysts contain extravasated urine following disruption of the proximal urinary tract. Physical examination might reveal a palpable dorsal abdominal mass and imaging confirms the presence of a fluid-filled mass in the retroperitoneal space with evidence of ureteral obstruction. A diagnosis is confirmed with exploratory laparotomy. Ureteronephrectomy with or without omentalization of the cavity has been performed to treat the condition.54 If contralateral renal function is normal the prognosis for these patients is very good. Perinephric pseudocysts are fluid-filled cavities in a perirenal location, usually a subcapsular accumulation of a transudate, which lack a true epithelial lining. Pseudocysts can be unilateral or bilateral and patients often present with renomegaly and abdominal distension (Fig. 36-11). These occur most commonly in older male cats, with clinical signs of renal dysfunction, but no history of trauma.55,56 In these cases, underlying renal pathology often dictates the prognosis. Percutaneous drainage is not effective in controlling recurrence of fluid accumulation. Resection of the pseudocyst wall can relieve clinical signs, but is not likely to provide long-term benefit unless the underlying disease is reversible (Fig. 36-12).57 If surgical resection is performed, omentalization may be helpful to resolve continued transudation.58 Survival in these patients is dictated by the degree of azotemia at presentation.
Kidney and ureter
Surgical anatomy
Kidney
Ureter
Diagnosis and general considerations
Diagnostic imaging
Radiography
Ultrasonography
Contrast radiographic studies
Intravenous urography
Antegrade pyelography

Surgical diseases
Urolithiasis in cats
Medical and minimally invasive management
Clinical presentation and investigation
Surgical management of uroliths
Ureteral stenting
Renal and ureteral trauma
Initial stabilization
Clinicopathological evaluation
Kidney
Ureter
Ureteral pelvic disruption
Devascularization or crushing injuries
Para-ureteral and perinephric pseudocysts and urinomas
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Kidney and ureter