1 Introduction
More than 100 years ago, the noted medical pathologist Virchow (1860) portrayed the skin as a protective covering for more delicate and functionally sophisticated internal viscera. At that time, the skin was primarily treated as a passive barrier to fluid loss and mechanical injury. The modern approach is to consider the skin as a highly complex organ in which precisely regulated cellular and molecular interactions govern many crucial responses to environmental changes.
The skin has many functions and apart perhaps from the liver, it could be said to have the most diverse range of ‘duties’ of all the major organs. Each of these functions is involved either individually or with others in the pathogenesis of skin disease (Table 1.1). The skin plays a major role in:
1. Protection against physical, chemical and microbiological agents
2. Protection of the internal milieu against fluid, protein and electrolyte loss, and from external wetting/maceration (waterproofing)
3. Thermoregulation (sweating and heat conservation)
6. Sensory functions (touch and other specialized receptors)
7. Storage of fat, water, vitamins, carbohydrates and protein
8. Immune functions within both the inner and outer layers of the skin.
Table 1.1 The major functions of the skin that affect dermatological health
| Function | Mechanism/cells responsible |
|---|---|
| Physical protection: Chemical/physical insult Ultraviolet radiation Antigens/haptens | Keratinocytes Melanocytes Langerhans cells, dermal lymphocytes, polymorphonuclear cells, mast cells |
| Microorganisms (virus/bacteria/fungi/parasites) | Keratinocytes, Langerhans cells, mononuclear phagocytes/mast cells |
| Prevention of water/electrolyte/protein loss (internal waterproofing) | Keratinocytes |
| External waterproofing (protection against external wetting)/lubrication | Keratinocytes/sebaceous glands/hair |
| Shock absorption | Collagen elasticity in dermis/subcutaneous fat |
| Sensation | Range of specialist sensory organs for pain, touch, heat, moisture, etc. |
| Thermoregulation (prevention of external heat gain and internal heat loss) | Dermis/subcutaneous fat/blood vessels/lymphatics/sweat glands |
| Calorie/energy reserve | Subcutaneous fat |
| Vitamin D synthesis | Keratinocytes |
| Individual recognition | Hair follicles (colour patterns)/sebaceous glands |
1. Physical protection. This is afforded by the inherent strength and elasticity of the integument. The skin varies in its thickness (being thickest on the legs and back and thinnest on the eyelids, the scrotum and medial thighs). The integrity of the physical barrier is important for protection against traumatic insult, solar radiation, and potential pathogens (viruses, bacteria, fungi and other parasites). Protection against bacterial attack is afforded not only by the physical barrier of the skin – the sebum and cellular components play an active role in preventing bacterial invasion and recognition of potentially damaging pathogens. Breaks in the skin integrity and alterations in its cellular and immunological function can result in pathological infections. For example, fungal infections such as dermatophytosis are common in horses but these infections require skin damage/trauma before disease can develop. Immunocompromising disease such as Cushing’s disease can result in opportunistic skin infections including bacterial, fungal and parasitic diseases.
2. Protection of internal milieu. The skin provides an effective barrier against evaporation. The skin is also virtually waterproof as a result of the physical arrangement of the epidermis and the secretions of the sebaceous glands. Where the skin is damaged over an extensive area (e.g. in burns and skin wounds) there may be a significant loss of blood and/or blood proteins. This might result in a debilitated animal that is less able to fight potential pathogens.
3. Thermoregulation. The skin has a significant blood supply (being one of the largest body organs) and thermoregulation is a major function. In cold conditions the cutaneous blood vessels are narrowed to preserve heat loss and in high temperatures they are dilated to help heat loss. Subcutaneous fat also provides a thermoregulatory function. Sweat glands provide an additional heat loss mechanism – horses have a rather unusual regional and patchy sweating ability that results from cutaneous vasodilation and catecholamine release. Some areas have a greater ability to sweat than others. In donkeys the mechanism for sweating is significantly different. They will only start to lose sweat when their body temperature has risen significantly and they retain their sweat at the skin level as opposed to the outside of the hair coat. This means that donkeys are better able to withstand high temperatures and water deprivation.
4. Blood pressure regulation. Cutaneous vasodilation and vasoconstriction are a major means for control of blood pressure. The mechanisms for this function are controlled by catecholamine release and autonomic nerve functions.
5. Vitamin D synthesis. It is easy to forget that the skin plays a major role in calcium homeostasis within the body and in this way has an influence on the function of many major organs. The vitamin D precursor 7-hydroxycholesterol is converted to the vitamin D precursor pre-vitamin D3, which in turn is a vital component of the active form of vitamin D.
6. Sensory functions. The skin is the major organ of touch and thermal sensation. There is a plethora of sensory nerve endings in the skin that allow perception of heat, cold, wet, dry, pressure and pain as well as many other sensations. Skin that is deprived of its nerve innervation may suffer insult without any self-protective reflexes. Also the neurological functions are responsible for sweating and blood supply.
7. Metabolic store. The subcutaneous fat deposits are an important active aspect of weight maintenance. In some cases the deposition of fat can be excessive and in others there may be an absence of fat. Under normal conditions fat deposition takes place in summer and during periods of plentiful food while mobilization of skin fat occurs in cold weather and in nutritional deprivation.
8. Immunological function. The skin plays a very active role in the recognition and recall of infectious and non-infectious challenges. Historically the skin was regarded as a passive organ but this is far from the case (see below, p. 11).
Dermatological disease is one of the commonest clinical presentations in equine practice. This is possibly due to the fact that skin is the largest organ system, it may be altered by a number of exogenous and endogenous factors, and owners usually recognize cutaneous lesions easily. It is easy to overlook the fact that the hoof, ergots, chestnuts and cornea are modifications of the skin and their diseases could justifiably be included in dermatology. However, it is also true to say that many cutaneous diseases are overlooked, trivialized or belittled as being ‘cosmetic’ nuisances whilst they are more often significant than not. There are many cutaneous diseases that have systemic effects and many systemic disorders that have significant and diagnostically helpful cutaneous manifestations; in some cases the skin signs are both the earliest evidence of disease and indeed the most obvious. This makes differentiation between primary and secondary skin disease a significant aspect of the diagnostic process and it remains disappointing that the skin is often overlooked during clinical investigations.
The key to successful treatment is accurate diagnosis. The basis of disease diagnosis must, by necessity, be guided by a thorough knowledge of what may be regarded as normal. This is usually a skill acquired by regular and careful scrutiny of many ostensibly normal horses so that subtle (possibly early) abnormalities can be identified quickly. Late diagnosis may sometimes make the investigation far easier – the lesions are advanced and therefore may be very typical for any particular condition. However, in these late stages there may be secondary changes that may confuse a diagnosis even if specialized tests are applied. Early lesions may be very subtle and this can introduce diagnostic and therapeutic problems. Furthermore, early diagnosis is often difficult because of the limited number of ways in which skin can react to the full range of infectious and non-infectious challenges; different diseases can have remarkably similar overt appearances (Fig. 1.1).
Careful and critical assessment of presenting clinical signs and an understanding of their significance in relation to a disease process, combined with a basic understanding of skin morphology and function, allow the clinician to categorize skin disease into broad groups such as nodules, alopecia, change in hair/skin colour. This categorization allows a clinician to reach an accurate diagnosis more easily and accurately than if attempts are made to guess a diagnosis without knowing all the facts. However, in practical circumstances, there are few cases in which a single category/syndrome is strictly applicable because most skin diseases either have multiple presenting signs or are complicated by secondary changes that mask the underlying primary condition. Also, categorizing skin diseases into defined syndromes as opposed to identifying the primary cause of the condition carries dangers. Significantly different diseases can be remarkably similar to the casual observer (Fig. 1.1).
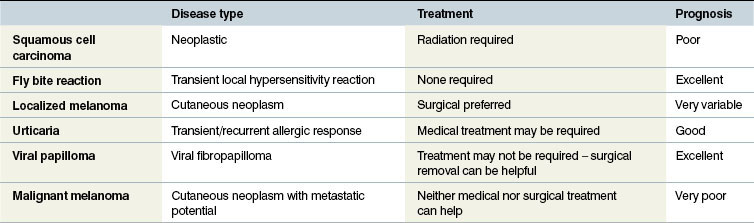
A single term for the clinical appearance of a cutaneous lesion may be very descriptive but subtle variations may perhaps not then be clearly identifiable. A broad categorization of a type of lesion is also not usually helpful. For this reason terms such as ‘eczema’ and dermatitis should be avoided as far as possible even though owners will often be satisfied with such an approach simply because these terms are commonly used in humans. For example, a diagnosis of ‘nodular skin disease’ could cover several distinctly different clinical entities and each of these would surely require very different therapy (Fig. 1.2 and Table 1.2).
Normal equine skin
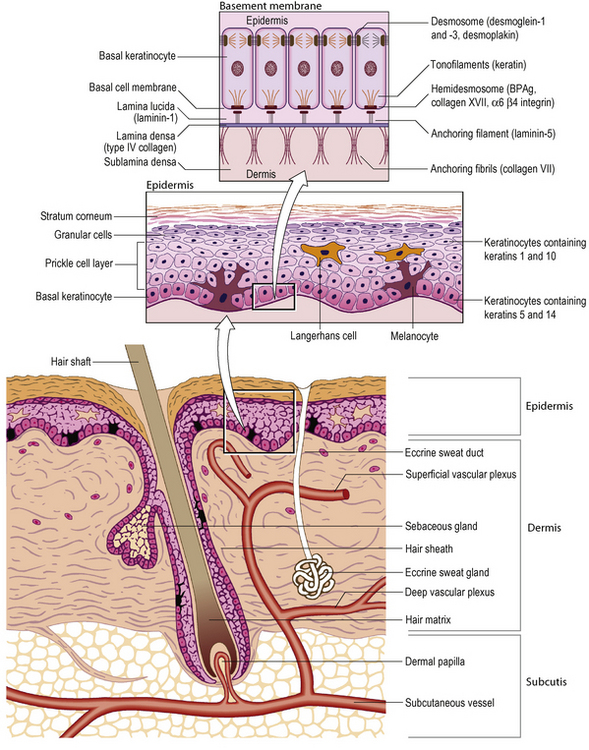
The normal anatomical structure of equine skin broadly follows the classical descriptions shown in many textbooks of anatomy (Fig. 1.3). However, there have been fewer studies on equine skin than for many other species and so significantly less is known about its particular function, the cutaneous blood supply and particular cellular behaviour patterns. Extrapolation from the other species seems an unreliable way to understand the skin of a highly adapted species but until more research is supported equine dermatology will remain behind that of other species in this respect.
Gross and histological anatomy of the skin
Epidermis
The epidermis is an avascular stratified squamous epithelium and is firmly attached to the dermis by a complex basement membrane (Fig. 1.3). This structure is important in some well-recognized skin diseases such as the pemphigus complex.
• The stratum corneum is the outermost epidermal layer and comprises many sheets of flat keratinized (anuclear) cells (keratinocytes) that eventually slough from the surface. Non-haired skin tends to have more layers in the stratum corneum than haired skin. This layer varies markedly in many disease conditions, being either excessively thick or abnormally thin.
• The stratum lucidum is absent in haired areas and is a thin layer of compacted, flattened, fully keratinized cells covering the granular layer or stratum granulosum. It consists of effete cells with basophilic keratohyalin granules. The stratum granulosum is absent or minimal in haired skin but prominent in hairless (glabrous) skin.
• Beneath these layers is the stratum spinosum, which consists of a zone of polyhedral cells attached by desmosomes; these intercellular bridges can be recognized histologically as ‘spines’. The innermost layer of the skin is the germinal layer or stratum basale, consisting of a single layer of mitotically active cuboidal to columnar cells resting on the basement membrane. There are abundant stem cells distributed in the stratum basale.
Intermixed in the basal cell layer are melanocytes, Langerhans cells and Merkel cells.
• Melanocytes synthesize melanin pigment from tyrosine, package it in the intracellular melanosomes and transfer the pigment to surrounding keratinocytes and hair bulbs via their dendritic processes, thereby imparting colour to the skin and hair. They are also present in the basal layers of the stratum spinosum.
• Langerhans cells are dendritic cells derived from bone marrow that circulate between the epidermis and the local lymph nodes. They act primarily as immune surveillance cells and are the major antigen-presenting cells of the skin. Antigens are presented to T lymphocytes and may be vital in viral and bacterial infection and in tumour cell recognition. It is possible to stain for these cells specifically but they cannot be identified on normal haematoxylin and eosin stained sections.
• Merkel cells are neuroendocrine cells and function as slowly adapting mechanoreceptors for touch sensation. A few Merkel cells are also found in the basal layer of the epidermis.
• Intra-epidermal lymphocytes are known to be T cells in the mouse and human (and likely to be similar in horses). They monitor the skin surface for extraneous potentially harming antigens.
Dermis
Adnexae
Hair follicles
Growth of hair is seasonal in animals, with the time of growth and mitotic activity termed the anagen phase. Microscopically, anagen hair follicles have a roughly spindle-shaped dermal papilla wrapped over the hair matrix in the form of a ‘ball and claw’. A transitional phase, during which cellular proliferation ceases, is the catagen phase. The follicle then enters a resting state, the telogen phase, after which mitotic activity and new hair production resume and the old hair is shed.
Special appendages (hoof/ergot, chestnut)
In solipeds such as the horse, the hooves consist of the wall, sole and frog. The sole and wall are composed of keratin. The wall consists of three layers, the inner one of which interdigitates with the dermis and acts as an anchor. The deeper portion of the dermis blends with the periosteum of the third phalanx. The frog is a dense fibro-elastic structure that has a major shock-absorbing function. Both the walls/sole and the frog are subject to significant pathological changes. An excellent description of the anatomy of the foot is available in Pollitt (1995).
Hair growth patterns
Some months before birth hairs develop over the body. Premature or dysmature foals always have a poorly developed hair coat and this is used as one of the indices of gestational age. The character of the hoof is also significant – at birth the hoof is soft but is recognizably ‘hoof’. It hardens rapidly after birth. Premature foals have a soft rubbery hoof capsule often with finger-like extensions from the sole margin. The hair of a newborn foal is soft and is usually short; in some specific lines of some breeds a longer curly coat is present. This is a ‘normal’ trait in these animals.
The horse has four types of hair:
1. The temporary hair that is shed in cycles governed by changes in daylight length. This comprises the large majority of the body and limb hair.
2. The tylotrich hairs are distributed throughout the body hair. They are recognizably larger than normal body hair and have a sensory function.
3. The permanent hair of the mane and tail. This is not shed in a coordinated way and grows continuously at the rate of about 2–5 mm per month. Eyelashes (vibrissae) are also classified in this category but clearly these do not grow as fast and are inherently shorter.
4. Tactile/sinus hairs. These are larger and more isolated hairs mostly found on the face, eyelids and ears. They are associated with sensory nerve endings and play an important tactile role.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree