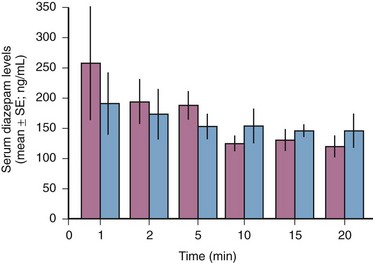
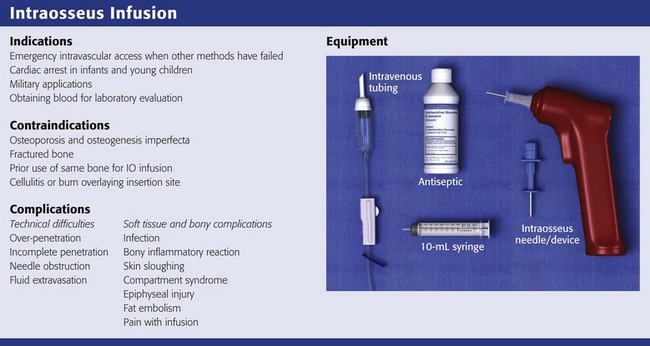
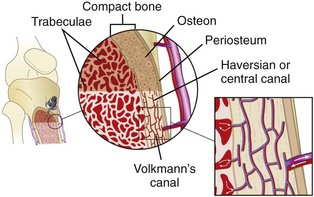
Chapter 25 Review Box 25-1 Intraosseous infusion: indications, contraindications, complications, and equipment. In a review of vascular access success rates in children in cardiac arrest, the average time needed to establish percutaneous peripheral IV access was 7.9 ± 4.2 minutes, with only a 17% success rate.1 Some authors advocate the use of central venous lines in children, but such lines are also difficult to place and are associated with risk for arterial injury, infection, and pneumothorax. Alternative routes of drug administration, such as the endotracheal and rectal routes, are not reliable in patients in shock or cardiac arrest.2 Peripheral IV access can also be difficult in adults, including those who are obese, have burn injuries, are volume-depleted, or are in shock.3 This difficulty is compounded in the prehospital or military setting, where environmental factors and the need for rapid transport can challenge even the most skilled practitioners.4 Intraosseous (IO) access can provide rapid, lifesaving intravascular access in challenging environments and in both pediatric and adult patients. The American Heart Association, the American Academy of Pediatrics, and the American College of Surgeons all recommend IO access in children in emergency situations when IV access is not immediately possible.5,6 The latest edition of the advanced trauma life support course of the American College of Surgeons also notes that IO access using specially designed equipment is an important option in adult trauma patients.5 IO access is often faster than IV access, and the success rate after failed IV attempts is high. In a retrospective study of pediatric cardiac arrest patients, time to IO access was significantly shorter than time to IV access.7 In a similar review of intravascular access during pediatric cardiac arrest, Brunette and Fischer2 noted that when compared with central venous access and venous cutdown, IO access and IV access were faster, and the success rate for IO access was 83% versus 17% for IV access. IO access can also be a rapid and successful technique in adults.8 Because of their success under difficult battlefield conditions, the U.S. military has adopted the use of IO infusion devices.5 IO access is not always successful. In a 5-year review of prehospital IO needle placement, success rates were higher in children younger than 3 years (85%) than in older children or adults (50%).7 The main causes of failure were errors in identification of landmarks and bending of the needles. Better needle design and new devices have helped overcome problems with bone penetration (see “Equipment and Setup,” later). One of the earliest references describing the IO route is attributed to Drinker and colleagues,9 who in 1922 examined the circulation of the sternum and suggested it as a site for transfusion. The route was not used clinically until 1934, when Josefson,10 a Swedish clinician, injected liver concentrate into the sternum of 12 adult patients with pernicious anemia and reported that all 12 improved. Subsequently, the technique became widespread in Scandinavian countries. In 1944, British physician Hamilton Bailey11 described the utility of sternal IO access in blackout conditions in London during World War II. In 1940, the technique was introduced to American clinicians by Tocantins and associates,12–14 who described a series of animal and clinical studies demonstrating that fluid is rapidly transported from the medullary cavity of long bones to the heart. They recommended using the manubrium in older children and adults and the upper part of the tibia or lower part of the femur in children 3 years or younger. Over the next 2 decades, thousands of cases of IO infusion of blood, crystalloid substances, and drugs were reported.15–19 The procedure was more commonly used in children because of the difficulty in achieving other forms of IV access. Nevertheless, during the 1940s, IO infusion was also used extensively in adults, and a sternal puncture kit for bone marrow infusion was a common component of emergency medical supplies during World War II.4,20 This resulted in more than 4000 reported cases of successful IO access in wounded soldiers.19 During this time, relatively few complications were reported despite the fact that the needles were often left in place for 24 to 48 hours. Heinild and coworkers in 194717 reviewed 982 cases of IO infusion and reported only 18 failures and 5 cases of osteomyelitis. None of the cases of osteomyelitis occurred in patients who received isotonic solutions. With the introduction of plastic catheters and improved cannulation techniques, the need for IO infusion as an alternative route for IV access diminished, and the technique was all but abandoned. In the mid-1980s, James Orlowski brought about a renaissance in the use of IO access for pediatric resuscitation. While traveling through India during a cholera epidemic, he observed emergency health care workers using IO access to deliver fluids and medications. In 1984 he wrote an editorial, “My Kingdom for an Intravenous Line,”20 in which he advocated the use of IO access during pediatric resuscitation. After Orlowski’s editorial, others began promoting the use of IO access to allow rapid drug delivery during cardiopulmonary resuscitation (CPR) in children.1,21,22 In 1988, IO techniques were adopted by the American Heart Association and included in the pediatric advance life support guidelines.6 Since then, the technique has become widespread throughout the United States and is recognized as an accepted alternative to IV access in pediatric emergencies and, increasingly, in neonatal and adult emergencies. In addition, the safety, ease, and effectiveness of the technique have led to its use in prehospital emergency care.7,23–26 Long bones are richly vascular structures with a dynamic circulation. They are capable of accepting large volumes of fluid and rapidly transporting fluid or drugs to the central circulation. The bone, like most organs, is supplied by a major artery (nutrient artery). The artery pierces the cortex and divides into ascending and descending branches, which further subdivide into arterioles that pierce the endosteal surface of the stratum compactum to become capillaries. The capillaries drain into medullary venous sinusoids throughout the medullary space, which in turn drain into a central venous channel (Fig. 25-1). The medullary sinusoids accept fluid and drugs during IO infusion and serve as a route for transport to the central venous channel, which exits the bone as nutrient and emissary veins.27 The medullary cavity thus functions as a rigid, noncollapsible vein, even in the presence of profound shock or cardiopulmonary arrest.28 Radiographic studies have demonstrated that radiopaque dye spreads only a few centimeters in the medullary space before being transported to the venous system.29 Figure 25-1 Schematic diagram illustrating the vascular anatomy of a long bone with an intraosseous needle in place. Almost every drug and fluid commonly used during resuscitation has been reported upon in clinical and preclinical IO studies. Medications and fluids that have been administered through IO infusion are listed in Box 25-1. Crystalloid infusion studies in animals have demonstrated that infusion rates of 10 to 17 mL/min may be achieved with gravity infusion and rates as high as 42 mL/min with pressure infusion.30–32 In a swine model of hemorrhagic shock, Neufeld and colleagues31 found that the IO delivery rate of crystalloid was similar to that with both peripheral and central venous administration. IO crystalloid infusions have also been shown to produce a significant increase in blood pressure in a hemorrhagic shock model in rabbits.32 In small animals (7 to 8 kg), the size of the marrow cavity is the rate-limiting factor, whereas in larger animals (12 to 15 kg), the size of the needle determines the flow.33,34 Blood under pressure can be infused approximately two thirds as fast as crystalloid fluids.33 However, in a swine model evaluating IO infusion for mild therapeutic hypothermia, IO infusion of ice-cold saline was not as efficacious as intravenous infusion.35 Comparisons of IO and IV infusion of drugs have demonstrated that the drugs reach the central circulation by both routes in similar concentrations and at the same time (Fig. 25-2).14,36 This holds true even during CPR, during which sodium bicarbonate has been shown to provide greater buffering capacity when administered by the IO route than by the peripheral IV route.37 Early IO access and infusion of epinephrine improved 24-hour survival in a swine model of ventricular fibrillation versus delayed IV administration.38 IO infusion of iodinated computed tomographic contrast material has also been reported as being successful,39 as has scorpion antivenin.40 Voelckel and associates36 demonstrated that bone marrow blood flow responds to both the physiologic stress of hemorrhagic shock and vasopressors given during resuscitation after hypovolemic cardiac arrest in dogs. After successful resuscitation, bone marrow blood flow decreased after high-dose epinephrine but was maintained after high-dose vasopressin. These findings in animal models suggest the need for pressurized IO infusion techniques during hemorrhagic shock and certain drug therapies. Obtaining venous access can be a difficult task even under the best circumstances. This difficulty is compounded during high-stress situations or low-flow states such as cardiac arrest. Studies have shown that IO devices provide a rapid and effective means of fluid and drug administration during pediatric CPR.1 This is also true during resuscitation of critically injured infants and children, in whom IO infusion of blood, colloids, or crystalloids (or any combination thereof) may be lifesaving. IO infusion is also beneficial in the management of children with other medical conditions, including those with respiratory distress, neurologic insults, dehydration and sepsis.42–44 The widespread use of IO devices has led to improved prehospital vascular access and a marked reduction in critical transport with failed vascular access.45 IO access is not commonly used in infants, but it is recommended as an alternative for medication and crystalloid administration when venous access is not readily obtained.46 IO infusion has been used with success in both premature and term infants.47–49 In one study, 30 IO lines were placed in 20 preterm and 7 full-term neonates with a variety of illnesses (e.g., respiratory distress syndrome, perinatal asphyxia, congenital cardiac anomalies) in whom conventional venous access had failed.48 All survived resuscitation with no long-term effects from IO line placement. Gestational age ranged from 32 to 41 weeks and birth weight ranged from 515 to 4050 g.48 In 2000, Abe and coworkers49 reported on the speed and ease of establishing newborn emergency vascular access by using turkey bones and plastic infant legs to simulate IO access and fresh umbilical cord to simulate umbilical venous catheterization. They demonstrated that for individuals who do not perform newborn resuscitation frequently, IO placement was easier and quicker than umbilical venous catheterization. A comparison of umbilical venous versus IO access in a simulated model of neonatal resuscitation showed that IO access was faster with no difference in error rate or perceived difference in ease of use.50 IO infusion is also indicated for adult patients in whom attempts at peripheral or central venous access have been unsuccessful. This may include adult patients with burns, trauma, shock, dehydration, or status epilepticus.51 Multiple sites, including the iliac crest, femur, proximal and distal ends of the tibia, radius, clavicle, and calcaneus may be used.52–55 Of these, the tibia may be less desirable because red marrow is replaced by less vascular yellow marrow or fat by the fifth year of life. In contrast, the sternum has been advocated as the best site to establish IO access in adults because it is large and flat and can readily be located.56 In addition, the sternum’s cortical bone is thin (1 to 2 mm) and the marrow space relatively uniform (6 to 11 mm).57 There has also been renewed interest in IO access by the U.S. military. In addition to logistic constraints that limit the volume of isotonic crystalloid fluids available to resuscitate injured soldiers, hypotension, environmental and tactical conditions, and the presence of mass casualties can lead to excessive delay in obtaining vascular access.4 The Army Institute for Research has compared several IO infusion devices, including the FAST-1 Intraosseous Infusion System (PYNG Medical Corporation, Richmond, British Columbia, Canada), the Bone Injection Gun (BIG; Waismed, Yokenam, Israel), the Sur-Fast Hand-Driven Threaded-Needle (Cook Critical Care, Bloomington, IL), and the Jamshidi Straight-Needle (Allegence Health Care, McGaw Park, IL).56 Success rates with these devices were similar (94% to 97%), and all were inserted in less than 2 minutes. The participants rated no individual device as being significantly better than the others. It was concluded that each device was easy to master and could be used appropriately during special operations when IV access could not be accomplished.56 A recent randomized controlled trial (RCT) of the BIG device versus the EZ-IO showed no significant differences in success rates or overall ease of use. Of 40 adults in the prehospital setting, vascular access was successfully achieved on the first attempt in 80% to 90% of patients within 2 minutes.58 Another recent RCT showed that a Jamshidi 15-gauge needle could be placed significantly faster than the FAST-1 device but had similar success and complication rates, as well as perceived ease of use.59 In addition to serving as a route for fluid administration, the IO needle may be used to obtain blood for typing, crossmatching, and determining blood chemistry in the marrow cavity. Serum electrolyte, blood urea nitrogen, creatinine, glucose, and calcium levels are very similar to those in samples obtained from an IO aspirate.60,61 Blood gas values obtained from the IO site were similar to those obtained from central venous sites during steady and low-flow states in one animal model.62 Brickman and colleagues63 demonstrated that bone marrow aspirates obtained from an IO needle in the iliac crest could be used reliably to type and screen blood for transfusion. A complete blood cell count may not be reliable because it reflects the marrow cell count rather than the cell count in the peripheral circulation. Furthermore, the aspirated blood usually clots within seconds, even if placed in a tube that contains heparin. Relatively few contraindications to IO infusion exist. Osteoporosis and osteogenesis imperfecta are associated with a high potential for fracture; therefore, unless absolutely necessary, the procedure should be avoided when these diagnoses are known. A fractured bone should be avoided because as fluid is infused, it increases intramedullary pressure and forces fluid to extravasate at the fracture site. This may slow the healing process, cause nonunion of the bone, or lead to a compartment syndrome. Similar extravasation of fluid can occur through recent IO puncture sites placed in the same bone. Hence, recent previous use of the same bone for IO infusion represents a relative contraindication to IO line placement. Needle insertion through areas of cellulitis, infection, or burns should also be avoided. Patients with right-to-left intracardiac shunts (e.g., tetralogy of Fallot, pulmonary atresia) may be at higher risk for fat or bone marrow embolization.64,65 Needles used for IO access range in size from 13 to 20 gauge and must be sturdy enough to penetrate bone without bending or breaking. They must also be long enough to reach the marrow cavity. Standard needles for drawing blood or administering medications are not adequate for IO infusions; they are not sturdy enough to penetrate bone and do not have a stylet to prevent bone from plugging the lumen. A cadaver study of IO puncture suggested that nonstyletted needles (2.5-cm, 18-gauge phlebotomy needles and 7.6-cm, 14-gauge IV needles) enter the marrow space successfully only about half the time.66 In the past, an 18-gauge spinal needle was commonly used in children younger than 12 to 18 months. This needle, though readily available in most EDs, often bends, is too long for rapid infusion of fluid, and has a greater risk for occlusion from clotted blood.67 Very small “butterfly” needles have been used with success in preterm infants.68 Like the Illinois Sternal/Iliac Aspiration Needle, the Jamshidi Disposable Sternal/Iliac Aspiration Needle (Cardinal Health, Dublin, OH) was designed for bone marrow aspiration, but it has a shorter shaft and smaller handle, which makes it easier to use. It comes in either 15 or 18 gauge and also features an adjustable plastic sleeve to prevent overpenetration. Once inserted, the needle protrudes approximately 2 inches from the skin, which increases the risk for accidental dislodgment. In a study using a turkey bone model, participants rated the Jamshidi needle easier to use than the Cook IO needle.69 The Sur-Fast Needle (Cook Critical Care, Bloomington, IN) is also specifically designed for IO insertion and infusion. It has a threaded shaft that helps secure the needle in the bone and a detachable handle that may be reused with multiple needles. In a study by Jun and associates,70 the Sur-Fast IO needle had a success rate similar to that of a standard bone marrow aspiration needle.
Intraosseous Infusion
Historical Perspective
Anatomy and Physiology
Indications
Contraindications
Equipment and Setup
IO Needles (Fig. 25-3)
Jamshidi Disposable Sternal/Iliac Aspiration Needle
Sur-Fast Needle
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Intraosseous Infusion