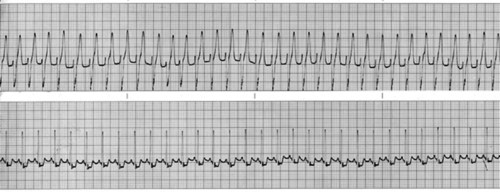
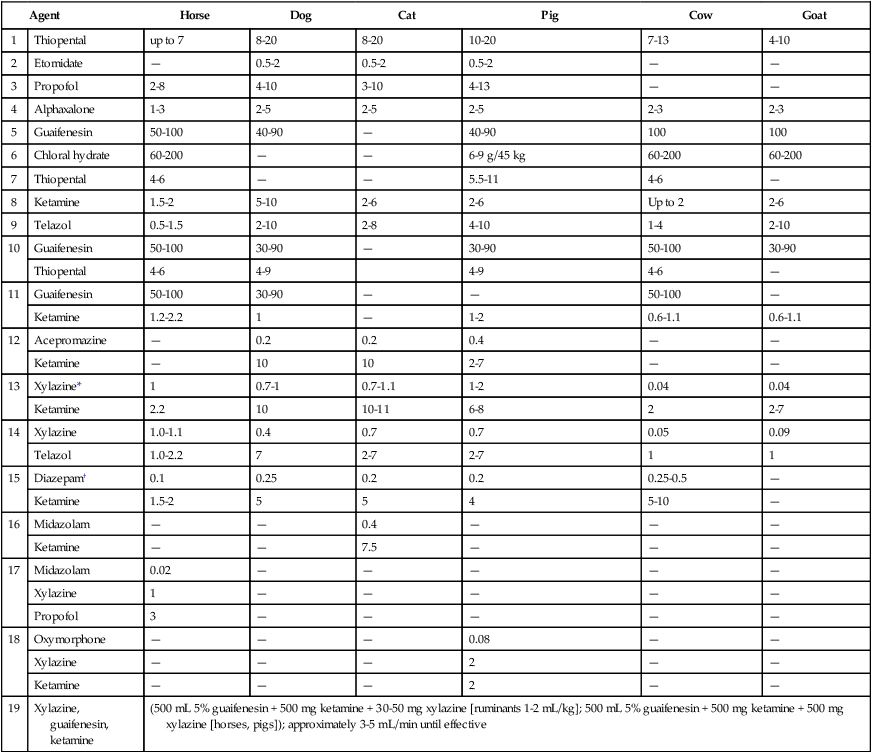
I Increasing intensities of central nervous system (CNS) depression can be produced, ranging from drowsiness and mild sedation to anesthesia and coma II Factors that can determine rate of onset, amount of depression, and duration of anesthesia C Rate of drug administration when administered IV D Route of administration (IV, IM, subcutaneous [SQ], intraperitoneal [IP]) E Drug pharmacokinetics and protein binding 1. Decreased renal function may prolong and intensify drug effects 2. Decreased hepatic function may prolong and intensify drug effects 3. Decreased plasma protein concentrations may increase the effects of drugs that are highly protein bound (barbiturates) F Animal’s level of consciousness (excited versus depressed) when the drug is administered G Acid-base and electrolyte balance (e.g., acidosis enhances barbiturate anesthesia) H Animal’s cardiac output and blood flow distribution I Drug tolerance (age, breed, obesity) III Most injectable anesthetic drugs produce unconsciousness by depressing the CNS A Some are used to control seizures (barbiturates; propofol) B Barbiturates depress spinal reflexes and can be used clinically for the treatment of strychnine poisoning A Most injectable drugs are administered IV 1. Dissociatives (ketamine; tiletamine-zolazepam) and neurosteroids (alphaxalone) can be administered IV or IM B Injectable anesthetic drug diluents can produce side effects 1. The extreme alkalinity of barbiturate solutions (pH 12 to 13), results in necrosis and sloughing if accidentally administered perivascularly; barbiturates should not be injected IM or SC 2. Intralipid, the diluent for propofol, supports bacterial growth and can interfere with some blood chemical tests 3. The pH of the commercially available formulations of ketamine is between 3.5 and 5.5 and is likely responsible for pain on injection when administered IM 4. Etomidate causes perivascular irritation and hemolysis due to high osmolality (4965 mOsmol/L) V Doses should be calculated on the basis of lean body mass (body weight minus fat; Table 8-1) TABLE 8-1 Intravenous Drugs Commonly Used To Produce Anesthesia of Short Duration (mg/kg) *Dexmedetomidine (small animals) or Detomidine (horses; farm animals), 2 to 10 µg/kg IV, can be administered to replace xylazine. †Midazolam, 0.2 to 0.6 mg/kg IV, can be administered to replace diazepam. I Barbiturates are categorized according to their duration of action III General anesthetic actions 1. CNS depression ranging from drowsiness and mild sedation to coma results from interaction with gamma aminobutyric acid A (GABA A) receptors which inhibit CNS activity 2. Response to barbiturate anesthesia a. Pentobarbital and ultrashort-acting barbiturates (thiopental, methohexital) decrease cerebral blood flow (CBF), cerebral metabolic rate of oxygen (CMRO2), and neuronal activity of the brain (e.g., dogs); the CBF/CMRO2 ratio is unchanged or increased; minimal changes in CSF pressure occur if ventilation (PaCO2) is normal b. Anesthetic concentrations of barbiturates decrease cardiac contractile force and vasomotor tone resulting in depression of arterial blood pressure (BP) and a decrease in intracranial pressure c. Ultrashort- and short-acting barbiturates are used to produce general anesthesia or to induce an animal to surgical anesthesia B Organ system effects and responses a. Barbiturates are respiratory depressants (1) Respiratory centers in the medulla and areas of the brain responsible for the characteristic rhythmic pattern of respiratory movement (apneustic and pneumotaxic centers) are depressed (2) Barbiturates depress the ventilatory response (minute ventilation) to increases in PaCO2 (3) The degree of respiratory depression is related to the dose and rate of administration b. Coughing, sneezing, hiccoughing, and laryngospasm occur during induction; these effects are exaggerated by excessive salivary secretion and are minimized by preanesthetic medication (atropine, glycopyrrolate) c. A short period of apnea frequently occurs after IV bolus administration of barbiturates a. Barbiturates produce significant cardiovascular depression. Cardiac contractile force and vasomotor tone are decreased. Induction to anesthesia is generally associated with a transient fall in BP, particularly if a bolus or large dose of drug is administered. b. Cardiac arrhythmias may occur (Fig. 8-1) (1) Thiobarbiturates (thiopental) sensitize the heart to epinephrine and induce autonomic imbalance; arrhythmias, particularly ventricular extrasystoles (ventricular bigeminy, trigeminy) can occur after thiopental administration (2) Thiobarbiturates increase both parasympathetic and sympathetic tone; this may lead to atrial or ventricular arrhythmias; rarely sinus bradycardia; first-, second-, or third-degree heart block and cardiac arrest occur c. Barbiturates usually cause a transient drop in BP; small doses of a barbiturate may cause dramatic decreases in cardiac contractility, cardiac output, and arterial BP in sick, depressed, or debilitated animals (1) Reduced doses should be administered very slowly to sick, debilitated, or depressed animals (2) Concentrations of thiopental greater than 2.5% are toxic to tissues if inadvertently administered subcutaneously and may injure the capillary musculature, causing capillary dilation and thrombophlebitis; injection into an artery causes severe pain, vasoconstriction, and tissue necrosis (3) Induction doses of thiobarbiturates occasionally cause an initial increase in BP and tachycardia in stressed or excited animals due to an increase in sympathetic tone. Note: pentobarbital produces an atropine-like effect. 3. Actions on the gastrointestinal (GI) system a. Depress intestinal motility (1) No direct effect on the kidney has been observed, unless a decrease in renal blood flow occurs; systemic hypotension may cause a decrease or cessation in urine production (2) A single administration of thiopental at therapeutic doses has no effect on liver function; large or repetitive doses of barbiturates do not interfere with liver function providing hemodynamics (BP and blood flow) are maintained 4. Effects on the uterus and fetus a. Pentobarbital is contraindicated in near-term animals because of fetal respiratory depression b. Barbiturates readily diffuse across the placenta into the fetal circulation; thiopental reaches mixed fetal cord blood within 45 seconds c. Doses of barbiturates that do not produce anesthesia in the mother can completely inhibit fetal respiratory movements
Injectable Anesthetic Drugs
Overview
General Considerations
Agent
Horse
Dog
Cat
Pig
Cow
Goat
1
Thiopental
up to 7
8-20
8-20
10-20
7-13
4-10
2
Etomidate
—
0.5-2
0.5-2
0.5-2
—
—
3
Propofol
2-8
4-10
3-10
4-13
—
—
4
Alphaxalone
1-3
2-5
2-5
2-5
2-3
2-3
5
Guaifenesin
50-100
40-90
—
40-90
100
100
6
Chloral hydrate
60-200
—
—
6-9 g/45 kg
60-200
60-200
7
Thiopental
4-6
—
—
5.5-11
4-6
—
8
Ketamine
1.5-2
5-10
2-6
2-6
Up to 2
2-6
9
Telazol
0.5-1.5
2-10
2-8
4-10
1-4
2-10
10
Guaifenesin
50-100
30-90
—
30-90
50-100
30-90
Thiopental
4-6
4-9
4-9
4-6
—
11
Guaifenesin
50-100
30-90
—
—
50-100
—
Ketamine
1.2-2.2
1
—
1-2
0.6-1.1
0.6-1.1
12
Acepromazine
—
0.2
0.2
0.4
—
—
Ketamine
—
10
10
2-7
—
—
13
Xylazine*
1
0.7-1
0.7-1.1
1-2
0.04
0.04
Ketamine
2.2
10
10-11
6-8
2
2-7
14
Xylazine
1.0-1.1
0.4
0.7
0.7
0.05
0.09
Telazol
1.0-2.2
7
2-7
2-7
1
1
15
Diazepam†
0.1
0.25
0.2
0.2
0.25-0.5
—
Ketamine
1.5-2
5
5
4
5-10
—
16
Midazolam
—
—
0.4
—
—
—
Ketamine
—
—
7.5
—
—
—
17
Midazolam
0.02
—
—
—
—
—
Xylazine
1
—
—
—
—
—
Propofol
3
—
—
—
—
—
18
Oxymorphone
—
—
—
0.08
—
—
Xylazine
—
—
—
2
—
—
Ketamine
—
—
—
2
—
—
19
Xylazine, guaifenesin, ketamine
(500 mL 5% guaifenesin + 500 mg ketamine + 30-50 mg xylazine [ruminants 1-2 mL/kg]; 500 mL 5% guaifenesin + 500 mg ketamine + 500 mg xylazine [horses, pigs]); approximately 3-5 mL/min until effective
Barbiturate Anesthesia (Discussed for Historical and Comparative Purposes)
Drug
Appropriate Duration of Action
Phenobarbital sodium
Long
Pentobarbital sodium
Short
Thiopental sodium
Ultrashort
Methohexital
Ultrashort
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Barbiturates
Barbiturates