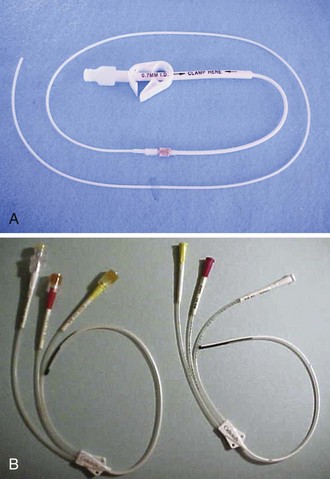
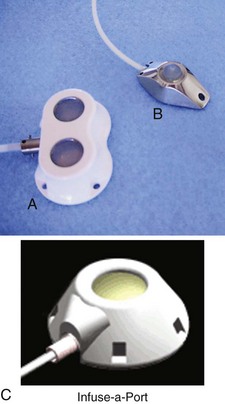
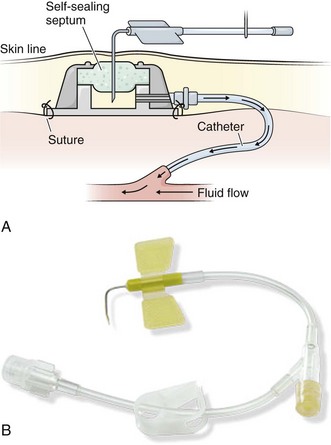
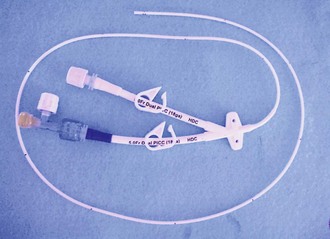
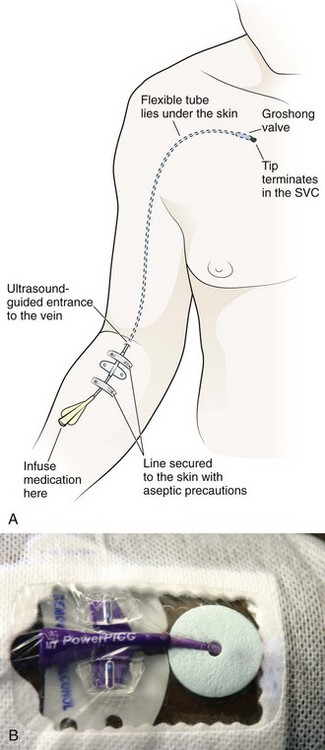
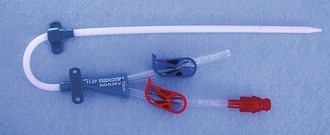
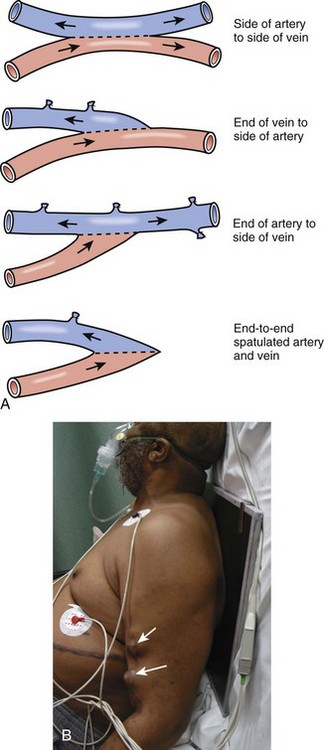
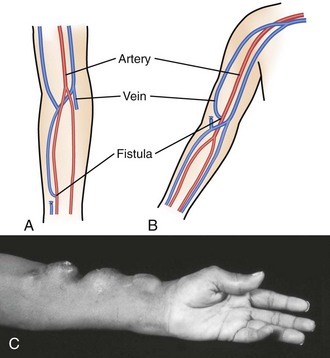
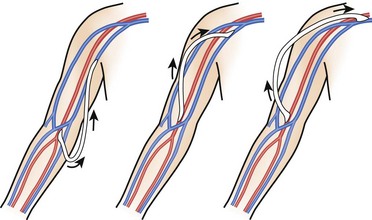
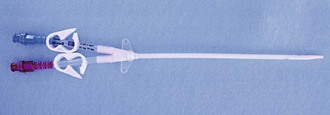
Chapter 24 Indwelling vascular lines provide routes for short- and long-term infusion of antibiotics, antifungal agents, hyperalimentation fluids, chemotherapeutic agents, blood products, analgesics, and anesthetic agents. In addition, they provide access for lifesaving procedures such as hemodialysis (HD) and plasmapheresis. As of 2008, nearly 382,000 patients were receiving HD therapy, with 3 to 5 million central venous catheters being placed yearly in patients in the United States.1,2 For the purpose of this chapter, all implanted devices and intermediate- to long-term catheters for vascular access are considered vascular access devices (VADs). Arteriovenous (AV) fistulas and AV grafts are included because of their similarities to VADs. A major advance that ultimately led to the development of several types of indwelling catheters was the introduction of Silastic (polymerized silicone rubber) in 1948 by the Dow Corning Corporation. This biocompatible material is an ideal substrate for intravenous (IV) catheters because it is chemically inert, antithrombogenic, rigid at room temperature, and pliable at body temperature. In 1973, Broviac and coworkers used this material to develop a 90-cm × 0.22-mm indwelling right atrial (RA) catheter for total parenteral nutrition (TPN).3 In 1979, Hickman and colleagues reported their experience with a 0.32-mm catheter that could be used for blood products and drug therapy in bone marrow transplant recipients.4 A totally implantable vascular access device (TIVAD) was described by Fortner and Pahnke in 1976.5 Since that time, TIVADs have become a mainstay of treatment in oncology patients. TIVADs allow less painful IV access and improve quality of life by permitting unrestricted mobility. Temporary access for HD via an external AV shunt was pioneered by both Quinton and Scribner and their coworkers in 1960.6,7 This original shunt was composed of a loop of tubing lying on the volar aspect of the forearm that connected the radial artery to a wrist vein. Although it provided effective dialysis, it was associated with a high rate of infection, thrombosis, and restriction of patient activity. Brescia and colleagues then introduced the peripheral subcutaneous autogenous AV fistula in 1966.8 This Brescia-Cimino internal fistula used a side-to-side anastomosis (the current procedure of choice for long-term HD) to connect the radial artery to the cephalic vein in the nondominant hand. Erben and associates described the routine use of percutaneous cannulation of the subclavian vein for HD in 1969.9 In 1979, Uldall and coworkers reported the development of a single-needle, subclavian HD catheter.10 VADs are typically chosen based on the least invasive, smallest catheter with the lowest risk for complications that will last as long as the length of therapy that is anticipated.11 Length of therapy is often the major consideration when choosing a device. Long-term VADs consist of cuffed, tunneled RA catheters and implantable ports. Medium-term VADs include midline catheters (lasting weeks), peripherally inserted central catheter (PICC) lines (lasting months), and Silastic subclavian or jugular catheters (percutaneous multilumen catheters). Short-term devices (see Chapter 21) include short peripheral IV, subcutaneous (butterfly), subclavian, and jugular catheters. Additional VADs include those used for dialysis, as well as AV fistulas and grafts. Several cuffed, tunneled RA catheters are available, each with differences tailored to specific applications (Fig. 24-1A). The Broviac is an all-Silastic single-lumen catheter with a 1.0-mm internal diameter (ID). It is 90 cm long with a thin intravascular segment (55 cm). The Hickman, also a Silastic catheter, has a 1.6-mm ID. It allows more frequent blood sampling without jeopardizing luminal patency.12 Single-, double- and triple-lumen variations exist. Hemocath/Permacath has the largest bore of the RA catheters, 2.2 mm ID. Quinton Instrument Company manufactures these catheters for HD, plasmapheresis, long-term nutritional support, and pain control. The main advantage of a cuffed catheter is that it can be used immediately, but it is not recommended for long-term access in patients undergoing dialysis if an AV fistula or graft is possible. Long-term dialysis with tunneled catheters has been associated with an increased risk for death, a 5- to 10-fold increase in the risk for infection, and a decreased likelihood of adequate dialysis.13 Ideally, these catheters should be used only as a bridge to longer-term devices.14 Nonemergency insertion of RA catheters is typically done in an operating room or interventional radiology suite. The device is introduced via the upper anterior chest wall and tunneled subcutaneously to enter the superior vena cava (SVC) system via the cephalic, subclavian, internal, or external jugular vein (Fig. 24-2). The distal tip of the flexible catheter is advanced to the distal SVC or into the mid-RA area. The subcutaneous tunnel isolates the venous puncture site from the skin and decreases the potential for bacterial contamination. Dacron cuffs (one near the venous entrance site and one near the skin exit site) anchor the catheter and are believed to inhibit colonization of the SVC by skin organisms.15 However, no study has been able to support this belief. Advantages of an RA catheter include ease of insertion and use, minimal interference with patient activity, low incidence of major complications or unintended dislodgment, ease of removal, and potential repair via a kit. Disadvantages include the need for regular maintenance and the potential for unacceptable cosmesis. In contrast to the Broviac and Hickman catheters, the Groshong catheter has slitlike openings just proximal to the end of the intravascular portion of the catheter (see Fig. 24-1B). This functions as a one-way valve to stop backbleeding and prevent air entry and embolism from the negative intrathoracic pressure. This feature obviates the need to use a heparin lock (saline may be used). In addition, external catheter clamping is not necessary. Disadvantages are its high cost and requirement for pressurized infusion systems.16 Since 1983, implanted ports have become the mainstay for long-term cancer therapy. TIVADs are tunneled RA catheters, but they differ from Broviac and Hickman catheters in that they have a subcutaneous titanium or plastic portal with a self-sealing septum (Fig. 24-3) that may be accessed by puncturing a specially designed needle (90-degree angled Huber needle) through intact skin (Fig. 24-4). Cosmetically, they are superior to external tunneled catheters, require less maintenance, and afford patients greater freedom of movement and activities such as swimming or bathing. TIVADs may be inserted on an outpatient basis under local anesthesia via a subcutaneous tunnel or open cutdown. The cutdown technique offers potential speed (mean placement time, 15 minutes), safety (negligible risk for pneumothorax), along with avoidance of early and late complications.17 Placement is typically in the nondominant arm with the portal in the upper part of the arm or chest unless a vein is occluded or radiation therapy is planned on that side. Disadvantages of this type of device include increased cost, the need for a specific noncoring Huber access needle, and the small gauge (20 to 22) of the access needle, which limits fluid infusion rates.16 PICC lines are centrally placed lines that were first described in the 1970s and originally developed for the neonatal population. Subsequently, their use expanded into the adult arena for prolonged antibiotic therapy, IV fluids, chemotherapy, TPN, and delivery of medications that are irritating to peripheral vessels. PICCs (Fig. 24-5) are made of two substances, either polyurethane (Intracath) or silicone (Intrasil), are radiopaque, and measure 50 to 60 cm in length with an outside diameter of 2 to 7 Fr. The catheter may have a single- or double-lumen configuration and can be open or closed ended or valved (e.g., Groshong). An open-ended PICC cannot prevent feedback of blood into the catheter and therefore must be flushed one or more times daily with heparinized saline. The Groshong valve reduces backup of blood into the catheter and therefore requires flushing as infrequently as once a week. The most common type of PICC line in use today is the 5-Fr, double-lumen, closed-ended catheter. Selection of the device should be based on the number of lumens necessary for therapy. Selection of the access site depends on many factors, including the suitability of target vessels, body habitus, handedness, ability to manage self-care, comorbid conditions, desired infusion rate, number and compatibility of concurrent infusions, infusate characteristics, and the estimated duration of therapy. Infusate that is hyperosmolar (e.g., TPN) or vesicant requires rapid dilution. Accordingly, the tip must be in the SVC, where the estimated flow rate is 2000 mL/min. PICC lines are most frequently placed in the superficial veins proximal to the antecubital fossa (usually the basilic or cephalic vein) (Fig. 24-6). However, they may also be placed via a transhepatic or translumbar approach when the SVC is thrombosed or occluded.18 Advantages of PICC lines include usefulness in a wide variety of clinical situations, ease of placement, and ease of use and maintenance. They do not require surgical insertion and may be placed in an outpatient setting. A PICC line is an excellent vehicle for medium- to long-term IV therapy. With proper care, PICCs can remain in place for long periods, even months to years.19 To remove a PICC line, simply withdraw it from the vein and apply pressure and a sterile bandage. Vascular access, which is often referred to as the Achilles heel of renal patients, remains problematic. From the moment that the first access is created, an ongoing process is started that will end with loss of all access sites if the patient survives long enough.20 Clinical practice guidelines of the National Kidney Foundation—Disease Outcomes Quality Initiative (NKF-DOQI) recommend early construction of an AV fistula and avoidance of catheters for permanent or prolonged vascular access,17,21 with less than 10% of permanent access being in the form of catheters.22 However, one study demonstrated that more than half the patients began dialysis with a central catheter because a well-developed AV fistula was not available.23 The risk of requiring three or more vascular access sites is almost double in patients who start HD with a central catheter. Temporary vascular access catheters (Fig. 24-7) are used for emergency HD or for temporary HD access if a more permanent dialysis route (AV fistula or graft) is not available or has recently been placed and has not matured yet. The advantage of tunneled catheters is the ability to provide immediate access or temporary access while a more permanent structure matures, but this carries a long-term risk for infection, dysfunction, and central venous stenosis. The majority of bacteremia episodes in patients undergoing HD are caused by HD catheters, with an approximate 20% to 25% risk over the average duration of use. Figure 24-7 Mahurkar 11.5-Fr. × 16-cm Double-Lumen Catheter for temporary hemodialysis, apheresis, and infusion. These large-bore catheters allow the necessary blood flow rate of 300 mL/min for dialysis. The Quinton catheter has two ports, one to deliver the patient’s blood to the dialysis machine and another to return the blood to the patient’s circulation (see Fig. 24-2B). These catheters are placed in a central vein, either the internal jugular, subclavian, or femoral. The right internal jugular approach is preferred, even if permanent access is to be created on the right side, because it has the lowest thrombosis rate. The NKF-DOQI recommends avoiding the subclavian vein unless no other options exist or the ipsilateral arm has no more permanent access sites. For patient comfort, a special 180-degree catheter can be used (Fig. 24-8). There are two avenues to place this catheter: percutaneously or surgically. Emergency percutaneous placement may be performed by the emergency clinician at the bedside. Using sterile technique and after injection of a local anesthetic, insert the catheter by following the same procedure for placing a central line into one of the central veins. The goal of chronic HD vascular access is to provide safe, effective, and repeated easy access to the circulation. The three principal types of access are native AV fistulas, synthetic grafts, and double-lumen tunneled cuffed catheters (described above). The access types differ in failure rates, patency, complications, and other morbidity. In general, fistulas are preferred over grafts because of superior long-term patency and lower complication rates. However, fistulas are more likely than grafts to experience primary failure, defined as being unable to provide reliable access. Both fistulas and grafts must mature before they can be used for HD, a process that may take several weeks to several months. HD is often performed via a Quinton catheter during this hiatus, so a patient in the emergency department (ED) with both a catheter and a shunt either has a nonfunctioning fistula or graft or the access site is still immature. Grafts can usually be cannulated earlier than fistulas, often within weeks of placement. The minimum time for fistula maturation is at least 1 month. Complications common to both grafts and fistulas are thrombosis, infection, steal syndrome, aneurysms, venous hypertension, seromas, and local bleeding (Fig. 24-9). Overall, grafts are more likely to experience infection and thrombosis requiring thrombectomy or require other types of access intervention. The risk for infection with HD grafts is about 10% over prolonged use and 1% to 2% with HD fistulas. Graft infection requires complete excision to eradicate an infection of the foreign material, whereas fistula infections may resolve with IV antibiotic use. An AV fistula is a direct subcutaneous anastomosis of an artery and vein without prosthetic material and is the preferred means of vascular access for HD (see Fig. 24-9). Historically, the percentage of patients with AV fistulas fell well below the recommended goal, with most patients receiving AV grafts or long-term vascular access catheters. The most recent data from the Dialysis Outcomes and Practice Patterns Study (DOPPS) show that from 1996 to 2007, AV fistula use in the United States almost doubled (24% to 47%) and AV graft use fell by 50%.24 Use of an autogenous fistula is associated with the longest period of patency with relative freedom from thrombotic and infectious complications. Once a fistula matures, long-term patency is high (48% of AV fistulas versus 14% of AV grafts at 5 years), with low infection rates relative to grafts.25 An autogenous AV fistula is constructed by anastomosing an artery to a vein (see Fig. 24-9), preferably a nearby one. Various configurations are possible, but AV fistulas are typically an end-to-side vein-to-artery anastomosis. The radial-cephalic (Brescia-Cimino forearm) fistula in the forearm is the most frequently used (Fig. 24-10), with the brachial-cephalic, brachial-basilic, and rarely the proximal part of the thigh being alternatives. Over time, the venous portion of the shunt is subjected to high pressure, and flow becomes arterialized (hypertrophied and dilated), which renders it suitable for repeated vascular access. Full epithelialization of the shunt does not occur for 3 to 6 months, thus necessitating anticipatory placement as renal function worsens. If a forearm radiocephalic fistula cannot be constructed or has failed, an AV bridge graft using a donor vein or synthetic material is a well-accepted alternative. Several synthetic materials are used for grafts. Polytetrafluoroethylene (PTFE) is the most commonly used but takes 3 weeks to mature. An available polyurethane graft (Vectra) has the ability to be accessed within 24 hours. A standard graft is 6 to 8 mm in diameter and usually positioned in a U-shaped subcutaneous tunnel in the forearm. The graft is attached by end-to-side anastomoses to the brachial artery and antecubital vein. If no suitable antecubital vein is available, a straight bridge graft between the brachial artery and either the axillary or the basilic vein is often used. Multiple configurations are possible (Fig. 24-11). The characteristic C shape of the graft can aid in differentiating a graft from a more tortuous fistula. A jump graft between opposite extremities with creation of a loop across the chest or anastomosis of the axillary artery to the iliac vein is a possibility if all other sites have been exhausted. When compared with AV fistulas, AV grafts have a significantly higher incidence of thrombosis, infection, pseudoaneurysm formation, and limb loss. PTFE grafts have a low primary patency rate (29% at 1 year according to one study).26 However, they have a low incidence of aneurysm formation and are comparatively easy to revise. The estimated life span of a PTFE graft in clinical practice is often less than 2 years. The emergency need to administer parenteral medications to patients lacking other means of vascular access is the most common reason to access a VAD in the ED. Assuming that proper access methods are used to prevent infection, the greatest risk is sludging in the catheter with resultant occlusion. After administering medications, follow with a saline flush to clear the catheter and ensure that the medications reach the circulation. Do not administer medications concurrently that are known to be incompatible when mixed (e.g., calcium and bicarbonate), even through separate ports of multilumen catheters. Blood specimens, including samples for culture, can also be obtained via VADs. For phlebotomy specimens, stop the infusion, use appropriate catheter antisepsis, remove fluid occupying dead space in the catheter, and follow the blood draw with a flush of heparinized saline.27 To accomplish phlebotomy, withdraw the dead space solution, reclamp it, and use a separate syringe to remove the desired amount of blood.28 If clots are withdrawn, continue withdrawing blood until it is clot free. Inject bolus medications and infuse IV solutions through the catheter, and clamp it whenever it is unattached. Deliver a 5-mL normal saline flush between medications through a 10-mL syringe. On completion of either blood withdrawal or medication infusion, inject 3 to 4 mL of saline to flush it and then inject 3 to 5 mL of heparin (1000 U/mL). Clamp the line and reposition the cap.28 Note that 1000 U/mL of heparin should be used; less concentrated solutions may promote clotting. Do not inject larger amounts because it can heparinize the patient systemically. Groshong catheters need not be flushed with heparin but instead may be flushed briskly with 5 to 10 mL of saline. Multilumen central catheters have one port for each lumen, so access each one in the same manner. After antiseptic preparation, gain access either by inserting a needle or a syringe into the protective cap or by removing the cap entirely. Flush with 5-mL normal saline or sterile water, and verify backflow before all subsequent procedures. Perform phlebotomy through the proximal lumen to prevent mixing with medications being delivered through the other ports. Deliver IV infusions in similar fashion, and inject a normal saline flush between medications. Terminate the procedure by flushing 3 to 5 mL of heparin (1000 U/mL) through each port.
Indwelling Vascular Devices
Emergency Access and Management
Historical Perspective
Indwelling VADs
Cuffed, Tunneled RA Catheters (Broviac, Hickman, Hemocath, Leonard, Raaf)
Groshong Catheter
TIVADs/Ports (Port-A-Cath, Proport, Infuse-A-Port, Mediport)
PICC (Nontunneled, Noncuffed)
HD VADs
Temporary Dialysis Catheters (Quinton, Mahurkar, Tessio, Vascath, Uldall)
Chronic HD Vascular Access
AV Fistulas
AV Grafts
Accessing Vads in the ED
Accessing Long-Term Venous Access Catheters
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine